A 26-year-old lactating mother of a six-week-old baby attended your clinic with a three-day history of fever and a painful lump over the right breast. She had been feeding her baby every 2–3 hours via direct latching. On examination, her temperature was 38.5°C. There was a 1-cm tender breast lump at the 9 o’clock position, 2 cm away from the areola. The patient suspected that she was having an infection of the right breast and wondered if she should continue to breastfeed her baby. She was concerned whether medications were needed for her illness and if the illness and treatment would affect the quantity and quality of her breast milk.
WHAT IS BREASTFEEDING?
Breastfeeding is the process of feeding a mother’s breast milk to her infant, either directly from the breast or after expression.(1) Breastfeeding and breast milk provide an infant with calories and nutrients, including macronutrients (fat, protein and carbohydrates) and micronutrients (vitamins and minerals).(2)
HOW RELEVANT IS THIS TO MY PRACTICE?
The World Health Organization (WHO) and the United Nations International Children’s Emergency Fund (UNICEF) strongly advise exclusive breastfeeding for the first six months of life, followed by the introduction of adequate and safe complementary foods with continued breastfeeding up to two years and beyond.(3) This is also advocated by the American Academy of Pediatrics, the American College of Obstetricians and Gynecologists, the American Academy of Family Physicians and the Academy of Breastfeeding Medicine, and is supported by the Ministry of Health, Singapore.(4-8)
Exclusive breastfeeding offers a multitude of benefits to both mother and child. Benefits to the infant include decreased risk of asthma, atopic dermatitis, gastroenteritis and otitis media, as well as a lower risk of childhood leukaemia, obesity and both Type 1 and Type 2 diabetes mellitus. There is also a lower risk of necrotising enterocolitis and sudden infant death syndrome in preterm babies. Maternal benefits include decreased risk of breast and ovarian cancer, cardiometabolic disease (Type 2 diabetes mellitus, hypertension and cardiovascular disease) and postpartum depression. Successful breastfeeding can also positively influence the bond between the mother and the child.(9,10)
Locally, according to the National Breastfeeding Survey in 2011, 50.3% of mothers exclusively breastfed their children on the day of discharge; however, the rate plunged to 0.8% at six months after delivery.(11) These figures clearly show that our new mothers have ongoing challenges that need to be addressed in order to achieve the recommended breastfeeding duration of six months.
WHAT CAN I DO IN MY PRACTICE?
In Singapore, many hospitals that provide obstetric care have implemented the Baby-Friendly Hospital Initiative (BFHI), a global effort by UNICEF and the WHO to implement practices that protect, promote and support breastfeeding. Components of the BFHI include skin-to-skin contact at birth, early initiation of breastfeeding, lactation support and breastfeeding education.(12) This should be followed by post-discharge primary care support to maintain breastfeeding rates and lengthen the duration of breastfeeding. Support may be provided opportunistically during routine postpartum reviews and child developmental visits, where the mother may be interviewed regarding her current breastfeeding status and given an opportunity to clarify her doubts. Family physicians are also often the first contact points for mothers facing issues with breastfeeding, and it is, therefore, our responsibility to equip ourselves with the required knowledge and skills to provide prompt and accurate evaluation and support to them.
Common breastfeeding problems leading to cessation of breastfeeding in Singapore
The three most common reasons that lead to breastfeeding cessation locally are perceived insufficient milk supply, painful nipples or breasts and difficulty latching.(13-15)
Perceived insufficient milk supply
The best way to determine the adequacy of milk supply is to assess the infant for sufficient milk intake. This can be objectively done by evaluating the infant’s weight, amount of urine and bowel output. Newborns normally feed about 8–12 times per day and should appear content and relaxed after feeds. Babies who are directly latching should have periods of ‘nutritive suckling’, where there is a rhythmic ‘suck and swallow’ pattern. This occurs because the let-down reflex has been activated, and the baby is swallowing larger mouthfuls of milk. They should regain their birth weight by ten days to two weeks of life, and then gain about 105–210 g per week (15–30 g per day).(16,17) Newborns’ stools are initially black, or dark green and sticky. They should have at least 1–2 soiled diapers in the first two days of life. The stools should transit to green by Day 3, then to loose and seedy mustard yellow by Day 4 or 5. The frequency of soiled diapers should also increase to at least 3–4 soiled diapers per day by Day 4 of life. Neonates should also have at least one wet diaper on Day 1, increasing by one wet diaper each day to reach six heavy, wet diapers with pale yellow or clear urine daily.
If the infant puts on weight, with adequate urine and bowel output, the mother can be reassured that she has an adequate milk supply. In such cases, a fussy infant, breasts feeling ‘less full’ or ‘empty’, or low yield on pumping are unreliable symptoms and do not indicate low milk supply. If the infant is not thriving as expected, there may be issues with milk supply or transfer. In such cases, the mother may be referred for professional evaluation, such as to a trained lactation consultant. If supplementation is required, the mother’s own expressed milk or pasteurised donor milk may be offered. For medically necessary formula supplementation, the Academy of Breastfeeding Medicine protocol for supplementation may be used.(18) Meanwhile, the mother should be encouraged to continue breastfeeding on the baby’s demand, as milk production operates on a demand and supply principle, with more frequent emptying stimulating greater production of breast milk.
Lactogenesis II, otherwise known as the time when ‘milk comes in’, occurs between 48 and 96 hours postpartum, and is marked by an increase in lactose secretion in the milk, increase in milk volume, and change in viscosity to a thinner, more watery consistency. Delayed lactogenesis is more common in women with risk factors such as primips, obesity, diabetes mellitus and polycystic ovarian syndrome, and those who had a prolonged second stage of labour or Caesarean sections.(19) These women will benefit from early breastfeeding support and monitoring.
Painful nipples/breast and difficulty latching
A good latch is vital for successful breastfeeding, as it allows for effective milk transfer and complete emptying of the breast. An ineffective latch causes nipple pain and increases the risk of breastfeeding complications such as blocked milk ducts, engorgement, mastitis and abscesses. Milk supply, in turn, can be adversely affected and can lead to premature cessation of breastfeeding. Therefore, assessment and correction of the latch should always occur in tandem with the management of acute breastfeeding problems.
How can one achieve a good latch? The infant should be positioned to face the chest of the mother. The neck of the infant should not be hyperextended or flexed to reach the nipple. The mother should then guide the nipple towards the roof of the infant’s mouth so that the latch can cover as much of the areola as possible. There should be 3–4 cm of breast tissue in the infant’s mouth and her chin should be firmly touching the breast. A video on breastfeeding techniques is available at https://www.youtube.com/watch?v=j2xxJ8Hw_ek. If the mother’s pain persists despite having a good latch during breastfeeding, the infant should be assessed for ankyloglossia. Ankyloglossia is characterised by a short, thickened or abnormally tight lingual frenulum that limits the infant’s range of tongue movement. Referral to a trained lactation consultant is recommended, and some babies may benefit from treatment with frenotomy.
Other causes of nipple pain include ill-fitting breast pump flanges and cracked nipples. A well-fitting flange should allow the nipple to move freely in the breast flange tunnel without much of the areola drawn into the flange with the nipple. Flange sizing guides are available from most of the popular breast pump websites. Breast milk and lanolin ointment may help to heal cracked nipples.
Causes of painful breast lumps include blocked milk ducts, engorgement, mastitis and abscesses. Less common causes are galactocele, enlarged lymph nodes and, most importantly, breast cancer. A blocked milk duct usually presents as a painful breast lump with erythema of the overlying skin, whereas engorgement leads to more generalised pain and swelling of the breast. Mastitis presents similarly as blocked milk ducts but is more often associated with fever and systemic symptoms. It can occasionally progress to an abscess. Blocked milk ducts and engorgement usually resolve with a good latch and continued breastfeeding on the affected side. Additional measures such as warm compress before nursing and altering the breastfeeding position such that the baby’s chin points in the direction of the clogged duct are also helpful. Cold compression can be applied after nursing to relieve pain and swelling. Patients with mastitis require additional support such as oral antibiotics, antipyretics and analgesia. Patients with breast abscess should be referred to breast surgeons for further management, such as needle aspiration or incision and drainage.
Candida infections of the nipple or breast cause burning or shooting pain that begins after a period of pain-free nursing and may continue even after the feeding is over. Infants should be examined for the presence of oral thrush. Nystatin suspension is commonly used to treat oral candidiasis in infants, as it is poorly absorbed from the gastrointestinal tract. Rarely, Raynaud’s phenomenon of the nipples causes symptoms similar to those observed in breast candidiasis. Vasospasm, triggered by cold temperatures, causes blanching followed by cyanosis of the nipple. Treatment options include avoidance of triggers such as cold exposure and vasoconstrictive drugs. Nifedipine has been used successfully to relieve symptoms.
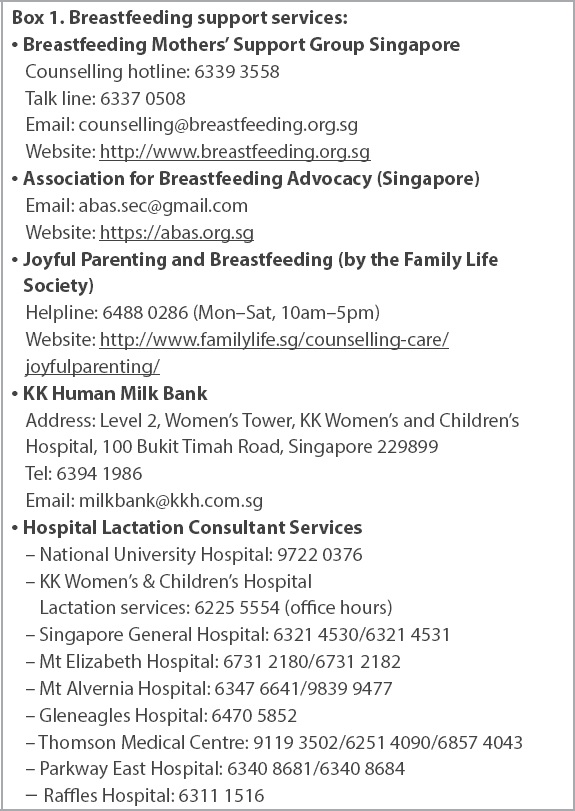
Various breastfeeding support services are available locally to support lactating mothers (
Box 1
Breastfeeding support services:
Other common queries from parents about breastfeeding
What are the contraindications to breastfeeding?
Mothers should neither directly breastfeed nor feed expressed milk to their babies if the infant has classic galatcosaemia, or if the mother is infected with human immunodeficiency virus, human T-cell lymphotrophic virus or Ebola virus, or has active herpes simplex infection with lesions present on the breast. She should also avoid breastfeeding if she has been given radioactive iodine or is using illicit drugs such as cocaine.(20) Some drugs may either affect milk supply or have adverse effects on the fetus. Physicians may refer to online databases such as LactMed (https://ncbi.nlm.gov/books/NBK501922) for information on the use of specific drugs during breastfeeding.
Can I continue breastfeeding when I am acutely sick or on long-term medications for my chronic illness?
It is safe to continue breastfeeding through most acute minor illnesses such as acute respiratory infections and acute gastroenteritis. Interruption of breastfeeding runs the risk of developing complications such as blocked milk ducts or mastitis. It is often challenging to reinstate breastfeeding after stopping, albeit temporarily. Further, continuing breastfeeding confers protection to the infant through the antibodies in the breast milk, making her less likely to fall sick.(21-23) Medications indicated for minor illnesses should be carefully reviewed and prescribed to ensure safety to the breastfed infant without compromising the milk supply and well-being of the mother.(24,25)
Most chronic illnesses are compatible with breastfeeding, unless the medications used by the mother are known to cause harm to the infant. These cases tend to be in the minority. In most instances, breastfeeding should be encouraged in view of the ample benefits that it brings to the mother and the infant. If advised to stop feeding breast milk temporarily by her doctor on medical grounds, a mother can maintain lactation by regularly expressing her milk, which may be discarded until direct breastfeeding can resume.
Should I continue breastfeeding if my baby is ill?
Breastfeeding comforts the sick infant and may aid in his/her recovery. The breast milk provides secretory antibodies and anti-inflammatory agents to fight infection and enhance healing.(26,27) If the infant can feed orally, breast milk is the best choice as it is the most easily digested food available. Disruption to breastfeeding is unnecessary and risks causing breast-related complications, leading to total cessation of breastfeeding. If the infant is hospitalised or unable to feed directly from the breast, the mother can provide expressed breast milk to be fed by cup, spoon or syringe.
How can I maintain my milk supply after returning to work?
Regular expression of breast milk is the key to maintaining the mother’s milk supply after she returns to work. The expressed milk can be chilled if used within the next day. Any excess can be stored in the freezer for emergency or future use.(28) The expressed milk can be fed via bottle, cup or spoon. If the baby is fed by bottle, paced breastfeeding is recommended. It mimics breastfeeding by allowing the infant to be more in control of the feeding pace and reduces the risk of overfeeding. At home, the mother can continue to breastfeed her infant.
Lactating mothers should be encouraged to continue breastfeeding after returning to work. Consideration of the following factors can help lactating mothers to continue breastfeeding after returning to work:
- Expression of breast milk – a good-quality breast pump will reduce the time needed to extract milk; hands-free pumps are also available
- Equipment and receptacles for milk storage and transport such as ice blocks, milk bottles and storage bags
- Ensuring that a good pumping spot is available at work that allows the mother to comfortably express breast milk
- Infant care planning while at work
Is breastfeeding safe for mothers who have confirmed or suspected COVID-19?
The WHO, UNICEF and the United States Centers for Disease Control and Prevention (CDC) recommend that breastfeeding should be supported wherever possible, even in mothers with confirmed or suspected COVID-19.(29-31) This is a reversal from an initial stand that the mother and infant should be separated to minimise the risk of postnatal transmission from maternal respiratory secretions. Vertical transmission from mother to newborn can also occur in utero, intrapartum or through breastfeeding. More recent evidence shows that the risk of vertical transmission is low, and the infection in the infant is typically mild or asymptomatic. Adherence to infection prevention and control measures is more essential to prevent contact transmission between mothers with suspected or confirmed COVID-19 and their newborns and young infants.(32,33)
Can mothers get a COVID-19 vaccination while breastfeeding?
While research on COVID-19 vaccines did not include women who were breastfeeding, the absence of direct data does not mean that the vaccines are not safe. According to the CDC, COVID-19 vaccines are not thought to be a risk to an infant who is being breastfed or receiving breast milk.(34) Neither inactivated nor live-virus vaccines, such as the AstraZeneca and Janssen vaccines, pose a risk to the breastfeeding mothers or their infants. The Pfizer-BioNTech and Moderna vaccines do not contain a live virus. The mRNA in these vaccines does not enter the core of the cell and is degraded quickly. These vaccines are considered to be effective in breastfeeding mothers and can pass on protective antibodies to the infant through breast milk.(34) Therefore, the WHO’s Strategic Advisory Group of Experts on Immunization guidance recommends that mothers who are vaccinated continue breastfeeding.(35) Locally, the Ministry of Health guideline states that it is safe for women who are breastfeeding to be vaccinated. There is no need to suspend breastfeeding to receive the Pfizer-BioNTech or Moderna COVID-19 vaccine.(36)
WHEN SHOULD I REFER TO A SPECIALIST?
Patients should be referred to a specialist in the following instances: (a) presence of a breast abscess that requires further management such as needle aspiration or incision and drainage; (b) when further evaluation is needed, in cases such as a suspicious breast lump; and (c) failure of treatment, such as mastitis not responding to oral antibiotics.
A family physician’s duty extends to educating the mother about the benefits of breastfeeding, helping her to differentiate facts from myths and supporting her by providing interventions directly or by referral. Most mothers are able to achieve successful breastfeeding practice with appropriate breastfeeding routines, maternal motivation to continue breastfeeding and skilled assistance with breastfeeding issues. In this COVID-19 pandemic era with disrupted and limited healthcare services, by enabling and supporting breastfeeding mothers, family physicians can make a positive impact in preventing the long-term clinical and economic impacts of COVID-19 on breastfeeding.
TAKE HOME MESSAGES
- Perceived insufficient milk supply, painful nipples or breasts and difficulty latching are the three most common reasons that lead to breastfeeding cessation in Singapore.
- Accurate counselling and support to breastfeeding mothers are key to avoid disruption of breastfeeding.
- Family physicians should know when to refer to specialists for further evaluation.
After making a clinical diagnosis of a blocked milk duct and mastitis, you provided the mother with online resources on applying warm compression and breast massage techniques to encourage milk flow and unblock the milk duct. You advised her to apply a cold compress on the affected area after nursing to reduce swelling. You prescribed ten days of oral augmentin, with oral paracetamol for fever and pain relief. You also taught her how to reposition her baby to improve latching and encouraged her to continue breastfeeding or empty her breast regularly, assuring her that the breast milk and prescribed medicines were safe for the baby’s consumption. At the review one week later, the mother had no more fever or pain, and the painful lump that you discovered during the initial visit had completely resolved.
SMJ-63-73.pdf


