Abstract
INTRODUCTION
Traumatic displaced femoral neck fractures in the elderly can be treated with cemented or uncemented hemiarthroplasty with good outcomes. Earlier studies reported a higher incidence of deep vein thrombosis (DVT) associated with cemented prostheses in elective total hip or knee arthroplasty. In addition, the hypercoagulable state after a traumatic femoral neck fracture and possible thrombogenic properties of bone cement could put these patients at greater risk for thromboembolism. We aimed to compare the incidence of DVT and progression to pulmonary embolism (PE) or mortality in cemented and uncemented hemiarthroplasty.
METHODS
The data of 271 patients treated with cemented or uncemented hemiarthroplasty after a traumatic displaced femoral neck fracture was retrospectively analysed for the incidence of DVT. The level of thrombosis, progression to PE and mortality were compared.
RESULTS
There were 133 (49.1%) patients with cemented hemiarthroplasty, while 138 (50.9%) had uncemented hemiarthroplasty. The patients had an average age of 76.6 (range 53–99) years and 11 (4.1%) patients had DVT. There were no significant differences in development of DVT, level of thrombosis, PE and mortality regardless of whether a cemented or an uncemented prosthesis was used.
CONCLUSION
Cemented hemiarthroplasty is not associated with higher risks of DVT, PE or mortality in patients with traumatic displaced femoral neck fracture. Cemented prostheses can be safely used for this group of patients.
INTRODUCTION
Hemiarthroplasty is the most common treatment for traumatic displaced femoral neck fractures in the elderly. Both cemented and uncemented hemiarthroplasty have been used with good results; recent literature shows that both techniques lead to good functional outcomes and postoperative pain control, although some authors reported that uncemented hemiarthroplasty was associated with more implant-related complications.(1-5) In earlier studies reported in the 1990s, the cemented prosthesis was associated with a higher incidence of deep vein thrombosis (DVT) in total knee replacements (TKR) and total hip replacements (THR).(6-10) Subsequent studies, however, provided contradictory results and there was a lack of new data thereafter.(11,12) Notably, all of these studies(6-12) used healthy patients for elective surgery, while patients with traumatic femoral neck fractures are potentially in a procoagulable state due to the nature of the trauma sustained in the initial injury.(13,14) In addition, several recent studies have reported on the possible thrombogenic properties of polymethyl methacrylate cement and the activation of platelet aggregation and cytokines, which could contribute to the pathogenesis of DVT.(15-17) With this background of controversy, we aimed to review and compare the incidence of DVT and its progression to pulmonary embolism (PE) or mortality in cemented versus uncemented hemiarthroplasty for traumatic displaced femoral neck fractures.
METHODS
We retrospectively reviewed all patients admitted to National University Hospital, Singapore, with traumatic displaced femoral neck fractures and treated with hemiarthroplasty from January 2011 to December 2013. Patients were identified using the hospital’s diagnosis and operative code system. Their case notes, electronic records and radiographs were reviewed. The local institutional review board approved this study.
Patients on anticoagulant therapy or who had a history of DVT or PE, haematological conditions, malignancy, pathological fractures and open fractures were excluded. From the records of the remaining patients, pertinent data on patient demographics (age and gender), use of aspirin, pre-injury ambulatory status and presence of comorbidities such as hypertension, diabetes mellitus, ischaemic heart disease, American Society of Anesthesiologists (ASA) score,(18) duration of surgery and type of anaesthesia was extracted and analysed statistically. Patients were classified by their pre-injury ambulatory status as independently ambulant, ambulant with walking aids or non-ambulant on wheelchairs. The ASA score was used to assess the overall health status of a patient and fitness for surgery. This grading system categorises patients as follows: ASA I – normal and healthy; ASA II – mild systemic disease; ASA III – severe, non-incapacitating systemic disease; ASA IV – severe, incapacitating systemic disease with a constant threat to life; and ASA V – moribund and not expected to survive with or without the operation. The presence of DVT and PE after surgery, level of thrombosis (proximal or distal) and mortality rate were subsequently reviewed.
Our institution does not routinely use pharmacological thromboprophylaxis for hip fracture patients. However, all patients with hip fractures are fitted with an intermittent pneumatic compression device for mechanical thromboprophylaxis. Doppler ultrasonography is routinely performed for both lower limbs on postoperative day 5. The presence of DVT was defined as the direct visualisation of thrombosis, loss of compressibility and impedance of normal blood flow in the affected vein. Proximal DVT was defined as thrombosis of the vein at the level of the popliteal, iliac or femoral vein, whereas distal DVT involved the calf veins such as the peroneal, posterior tibial and anterior tibial veins. PE was diagnosed using computed tomography pulmonary angiography in patients with a high clinical suspicion of PE. All DVT and PE patients were referred and treated by a haematologist according to the American College of Chest Physician Guidelines on antithrombotic therapy and prevention of thrombosis.
All surgeries were performed by fellowship-trained orthopaedic consultants and specialist registrars. The decision to use cemented or uncemented implants was made at the treating surgeons’ discretion. Postoperative rehabilitative protocol was standardised according to our institution’s hip fracture pathway; if tolerated, patients started early ambulatory exercises using a walking aid at postoperative day 2 with a physiotherapist. All patients were reviewed at two weeks postoperatively for wound inspection and suture removal if needed. Subsequent reviews were at six weeks, and three, six and 12 months with clinical examination and radiographic monitoring. Patients who complained of leg swelling, oedema or pain at follow-up would be further investigated using Doppler ultrasonography of both lower limbs to ensure that any delayed presentation of DVT was detected.
Data entry was performed using Microsoft Excel 2003 (Microsoft Corp, Redmond, WA, USA) and data analysis was performed with SPSS version 16.0 (SPSS Inc, Chicago, IL, USA). Frequency tables and descriptive statistics (mean, standard deviation or median, where appropriate) were presented for all variables. Categorical variables were presented as proportions and continuous variables were presented as mean. Chi-square test and Fisher’s exact test were used for comparisons between categorical variables, while Mann-Whitney U test was used for continuous variables. Multivariate analysis using multiple logistic regressions was performed to control for confounding factors. Statistical significance was set at p ≤ 0.05.
RESULTS
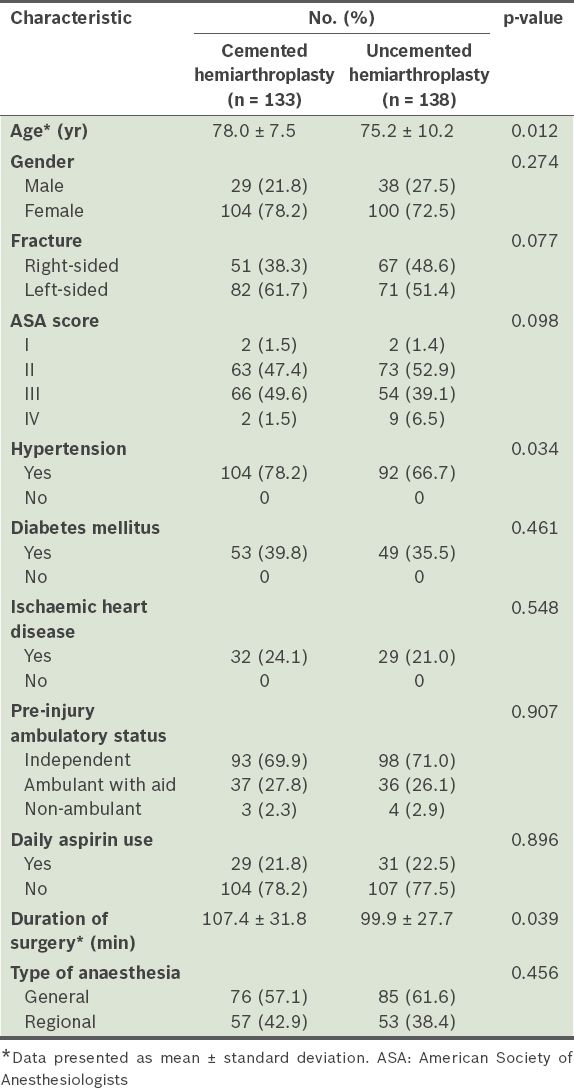
We identified 271 patients from our database who met the inclusion criteria from January 2011 to December 2013. A total of 133 (49.1%) patients underwent cemented hemiarthroplasty, while 138 (50.9%) underwent uncemented hemiarthroplasty. The patients had an average age of 76.6 (range 53–99) years. Of the 271 patients, 204 (75.3%) were female and 153 (56.5%) patients had left-sided femoral neck fractures. Under the ASA classification, the majority of our patients (n = 136, 50.2%) were ASA grade II, followed by 120 (44.3%) patients with ASA grade III, 11 (4.1%) patients with ASA grade IV and only 4 (1.5%) patients with ASA grade I. In terms of pre-injury ambulatory status, 191 (70.5%) patients were independent ambulators and 73 (26.9%) were ambulant with walking aids. Only 7 (2.6%) patients were non-ambulant at the time of injury. A majority of the patients (n = 161, 59.4%) underwent hemiarthroplasty under general anaesthesia. The average duration of surgery was 103.6 (range 23–238) minutes. In addition, it was found that 60 (22.1%) patients took aspirin daily for treatment of their chronic comorbidities. No significant differences were noted between the patients with cemented and uncemented prosthesis, except that those in the cemented group were significantly older (p = 0.012), more hypertensive (p = 0.034) and had a longer duration of surgery compared to the uncemented group (p = 0.039).
Table I
Demographics and characteristics of patients who underwent cemented and uncemented hemiarthroplasty (n = 271).
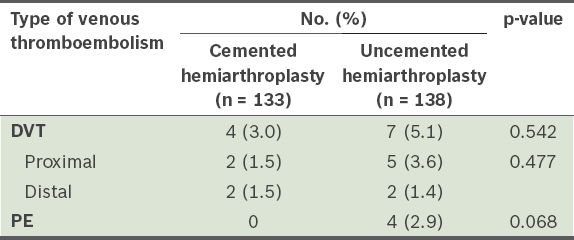
A total of 11 (4.1%) patients had DVT in this study population. The difference in the presence of DVT in the cemented and uncemented groups was not statistically significant. There were 7 (2.6%) patients with proximal DVT and 4 (1.5%) patients with distal DVT. Among those who had DVT, there was no significant difference in the level of thrombosis between the cemented and uncemented group (p = 0.542). In terms of development of PE, no statistically significant difference was noted between the cemented and uncemented groups (p = 0.068), although all four patients with PE underwent uncemented hemiarthroplasty (
Table II
Comparison of deep vein thrombosis (DVT) and pulmonary embolism (PE) in cemented and uncemented hemiarthroplasty (n = 271).
In addition, risk factors for DVT were analysed with univariate and multivariate analysis models using age, gender, ASA score, pre-injury ambulatory status, presence of comorbidities such as hypertension, diabetes mellitus and ischaemic heart disease, aspirin use, duration of surgery and type of anaesthesia. We did not find any significant differences among these factors that may have led to the development of DVT. However, it was notable that all 60 patients who took aspirin daily did not develop DVT, despite the lack of statistical significance (p = 0.071). These patients took aspirin for pre-existing medical comorbidities and not for prophylaxis against DVT.
DISCUSSION
Displaced femoral neck fractures are commonly seen in the elderly population after low-velocity trauma. The most common treatment for this injury is hemiarthroplasty, which can be cemented or uncemented. Both cemented and uncemented hemiarthroplasty have provided good results.(1-5) Earlier studies reported a higher risk of DVT in cemented TKR and THR.(6-10) Several studies have also demonstrated thrombogenic properties of bone cement that may contribute towards the development of DVT.(15-17) In addition, the hypercoagulable state after a traumatic femoral neck fracture would put these patients at greater risk for thromboembolism. Factors that reportedly contribute to this period of hypercoagulability are trauma at the initial injury, subsequent surgery, blood loss secondary to the fracture and at surgery, and fluid resuscitation before and after surgery.(13,14) Given these controversies, we reviewed and compared the incidence of DVT and progression to PE in cemented versus uncemented hemiarthroplasty in this population of patients predisposed to hypercoagulability.
Francis et al reported in their study that significantly more patients who received cemented hip prostheses developed DVT compared to those who received uncemented prostheses.(6) In Lynch et al’s study comparing routine physiotherapy versus continuous passive motion for patients after TKR, there was a higher incidence of DVT in patients who had cemented implants regardless of the use of continuous passive motion.(8) Subsequent studies such as those of Laupacis et al and Clarke et al reported contradictory results.(11,12) Clarke et al showed that the prevalence of DVT was actually higher in the uncemented TKR group, although the thrombi in the cemented TKR group had a significantly greater median length.(12) In our study, we found no statistically significant difference in the development of DVT (cemented 4[3.0%], uncemented 7[5.1%]) and level of thrombosis, regardless of whether cemented or uncemented hemiarthroplasty prostheses were used in the management of traumatic displaced femoral neck fractures. There was also no statistically significant difference in the presence of PE, although all four patients with PE had uncemented hemiarthroplasty (p = 0.068). Our findings show that cemented prostheses can be safely used in this population of patients.
Thrombogenicity of bone cement contributing to the pathogenesis of DVT has been widely investigated by several authors.(15-17) Dahl et al showed that polymethyl methacrylate monomer in concentrations equivalent to those found in mixed venous blood during cemented joint arthroplasty, together with other potential inducers, stimulates monocytes to tissue factor expression that may trigger coagulation.(15) In their study of three types of methacrylate-based cement commonly used for joint arthroplasty, Cenni et al reported that the bone cement induced secretion of factors that induce platelet activation, such as transforming growth factor b and b-thromboglobulin.(16) Cheng et al recently reported that patients with cemented TKR had significantly higher levels of cytokine CD14/42a, which was implicated as a measure of platelet monocyte aggregation in the thrombotic process.(17) Other researchers such as Qiu et al(19) investigated the effect of temperature at the popliteal fossa during cement curing in TKR and its association with the formation of DVT. They found that as bone cement polymerisation is an exothermic process, the temperature increases, but the small rise in heat was not associated with the development of DVT.(19) In spite of these reports, we feel that a significant rise in procoagulant factors or platelet activation after cemented joint arthroplasty in vitro may not translate to clinical manifestations of thromboembolism.
In our study, the group of patients with cemented hemiarthroplasty were older, more likely to be hypertensive and had a longer duration of surgery. A longer duration is expected for cemented prostheses due to additional steps in preparation, pressurisation and injection of cement. Older age and surgery duration have been associated with a higher risk of DVT. However, these three factors (i.e. older age, longer duration of surgery and hypertension) were not significant in our univariate or multivariate analyses.
One limitation of our study was its retrospective nature. The technique of ultrasonography is also operator-dependent. Although the use of Doppler ultrasonography to detect DVT may not be the gold standard compared to venography, it is noninvasive and provides good sensitivity (89%) and specificity (100%) in detecting proximal DVT.(20) In addition, we had a moderately large number of patients and gathered valuable data on the incidence of DVT in cemented and uncemented hemiarthroplasty for traumatic displaced femoral neck fractures in an Asian population. We also attempted to eliminate potential confounders by using multiple logistic regression analysis models.
In conclusion, our findings show that cemented hemiarthroplasty in traumatic displaced femoral neck patients is not associated with a higher incidence of DVT compared to uncemented hemiarthroplasty. There was no difference in progression to PE or rate of mortality between the two groups of patients.
ACKNOWLEDGEMENTS
We are exceedingly grateful for the help of Ms Teo Siew Ling and Ms Wang Xin Yu from the Department of Orthopaedic Surgery, University Orthopaedics, Hand and Reconstructive Microsurgery Cluster, at National University Hospital, Singapore, for their impeccable assistance in data collection.


