Abstract
INTRODUCTION
This study aimed to determine whether patient loads, infant status on admission and treatment interventions were significantly associated with inter-institutional variations in sepsis rates in very-low-birth-weight (VLBW) infants in the Malaysian National Neonatal Registry (MNNR).
METHODS
This was a retrospective study of 3,880 VLBW (≤ 1,500 g) infants admitted to 34 neonatal intensive care units (NICUs) in the MNNR. Sepsis was diagnosed in symptomatic infants with positive blood culture.
RESULTS
Sepsis developed in 623 (16.1%) infants; 61 (9.8%) had early-onset sepsis (EOS) and 562 (90.2%) had late-onset sepsis (LOS). The median EOS rate of all NICUs was 1.0% (interquartile range [IQR] 0%, 2.0%). Compared with NICUs reporting no EOS (n = 14), NICUs reporting EOS (n = 20) had significantly higher patient loads (total live births, admissions, VLBW infants, outborns); more mothers with a history of abortions, and antenatal steroids and intrapartum antibiotic use; more infants requiring resuscitation procedures at birth; higher rates of surfactant therapy, pneumonia and insertion of central venous catheters. The median LOS rate of all NICUs was 14.5% (IQR 7.8%, 19.2%). Compared with NICUs with LOS rates below the first quartile (n = 8), those above the third quartile (n = 8) used less intrapartum antibiotics, and had significantly bigger and more mature infants, more outborns, as well as a higher number of sick infants requiring ventilator support and total parenteral nutrition.
CONCLUSION
Patient loads, resuscitation at birth, status of infants on admission and treatment interventions were significantly associated with inter-institutional variations in sepsis.
INTRODUCTION
Neonatal sepsis in very-low-birth-weight (VLBW) infants weighing 1,500 g or less is a common problem in neonatal intensive care units (NICUs), with high morbidity and mortality rates reported in the literature.(1-4) Reports from various neonatal networks showed wide variations in sepsis rates (8.5%–42.0%) among NICUs.(1,5-7) For this study, data was collected from the Malaysian National Neonatal Registry (MNNR), which was established in 2003. One of the MNNR’s aims was to improve standards of neonatal care among its NICUs through systematic learning from other units based on evidence. We aimed to determine whether differences in patient loads; demographic, perinatal and patient characteristics; and resuscitation measures at birth were significantly associated with inter-institutional variations in sepsis rates.
METHODS
This was a retrospective study using data from the MNNR, which had a membership of 34 NICUs from Malaysian government hospitals in 2010. The MNNR database was anonymised. Approval for the study was obtained from the National Institutes of Health Malaysia. The inclusion criteria were VLBW infants born between 1 January 2010 and 31 December 2010, either in MNNR hospitals (i.e. inborn) or other facilities (i.e. outborn), and who were admitted to NICUs at these hospitals. The demographic and clinical data of the infants was submitted to the MNNR by trained staff in a standard format. Each infant was a unique case that was not duplicated in the registry, irrespective of the number of times the infant had been admitted to different participating NICUs.
Sepsis was diagnosed in symptomatic infants with a positive blood or cerebrospinal culture. If the infant had confirmed sepsis, data was collected on whether the first episode of sepsis occurred on or before Day 3 of life (early-onset sepsis [EOS]), or after Day 3 of life (late-onset sepsis [LOS]). Data on the following organisms was collected: group B streptococcus (GBS), methicillin-resistant Staphylococcus aureus, coagulase-negative staphylococcus (CoNS), fungus, Staphylococcus aureus, Klebsiella spp., Pseudomonas spp., and Acinetobacter spp. Other organisms that were isolated were specified. Gestational assessment was based on the mother’s last menstrual period, antenatal ultrasonography or Ballard’s score.(8) Infants were classified as appropriate for gestational age (AGA), small for gestational age and large for gestational age when their birth weights were between the 10th and 90th percentile, below the 10th percentile and above the 90th percentile for their gestational age, respectively.(9) Intrapartum antibiotics were administered to the infants’ mothers within 24 hours before delivery. Respiratory distress syndrome (RDS) was diagnosed based on clinical and chest radiography findings. Necrotising enterocolitis (NEC) was diagnosed based on Stage II or III of Bell’s criteria.(10) Patent ductus arteriosus (PDA) was diagnosed based on echocardiographic evidence or the presence of a continuous heart murmur in the left second intercostal space. The central venous catheters used were umbilical, or percutaneously or surgically placed.
Statistical analysis was performed using PASW Statistics version 18.0 (SPSS Inc, Chicago, IL, USA). Descriptive statistics were reported as mean ± standard deviation for continuous variables with a normal distribution, and median (interquartile range [IQR]) for those with a skewed distribution; categorical variables were reported as frequency and percentage. For comparison between groups in univariate analysis, chi-square test was used for categorical variables, Student’s t-test for numerical variables with normal distribution and Mann-Whitney U test for numerical variables with skewed distributions. For comparison of variables among three groups, the one-way analysis of variance (with Tukey and Games-Howell tests for post hoc analysis, where appropriate) and Kruskal-Wallis test were used for continuous variables, and chi-square test for categorical variables. Logistic regression analysis was performed to identify significant risk factors associated with EOS and LOS in VLBW infants between different groups. Potential risk factors used for logistic regression analysis were variables with p-value < 0.05 identified in the univariate analysis. All tests were two-sided and p-value < 0.05 indicated statistical significance.
RESULTS
The 34 NICUs received a total of 3,880 VLBW infants during the study period (
Fig. 1
STROBE diagram shows the details of very-low-birth-weight (VLBW) infants registered in the Malaysian National Neonatal Registry in 2010.
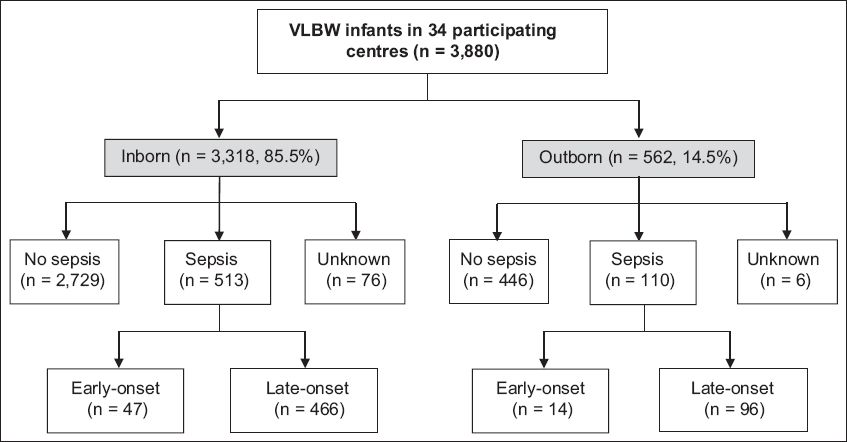
Fig. 2
Bar graphs show (a) early-onset sepsis (EOS) and (b) late-onset sepsis (LOS) rates of very-low-birth-weight (VLBW) infants in 34 neonatal intensive care units in 2010.
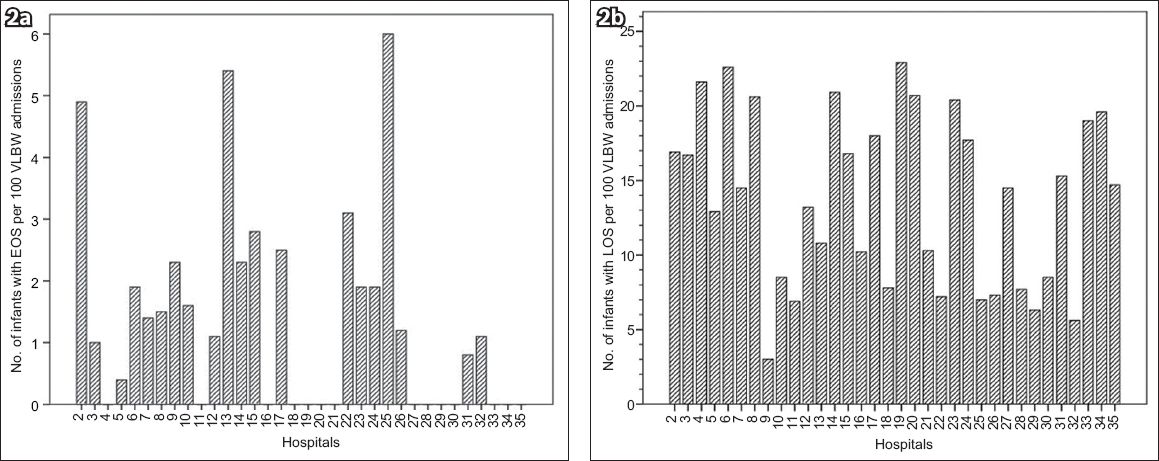
Table I
Mortality rates of very-low-birth-weight infants and the causative organisms.
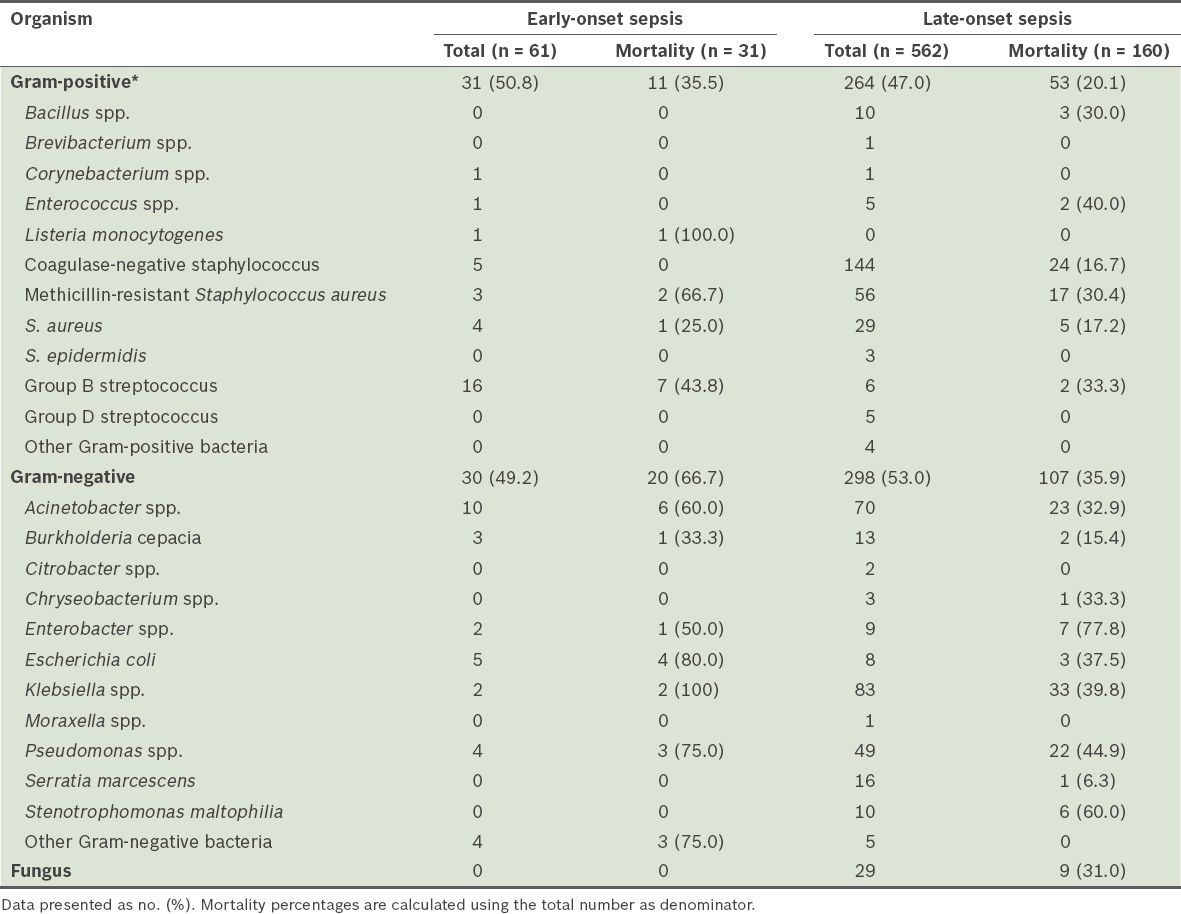
Table II
Comparison of maternal, perinatal and neonatal variables of very-low-birth-weight infants with and without sepsis.
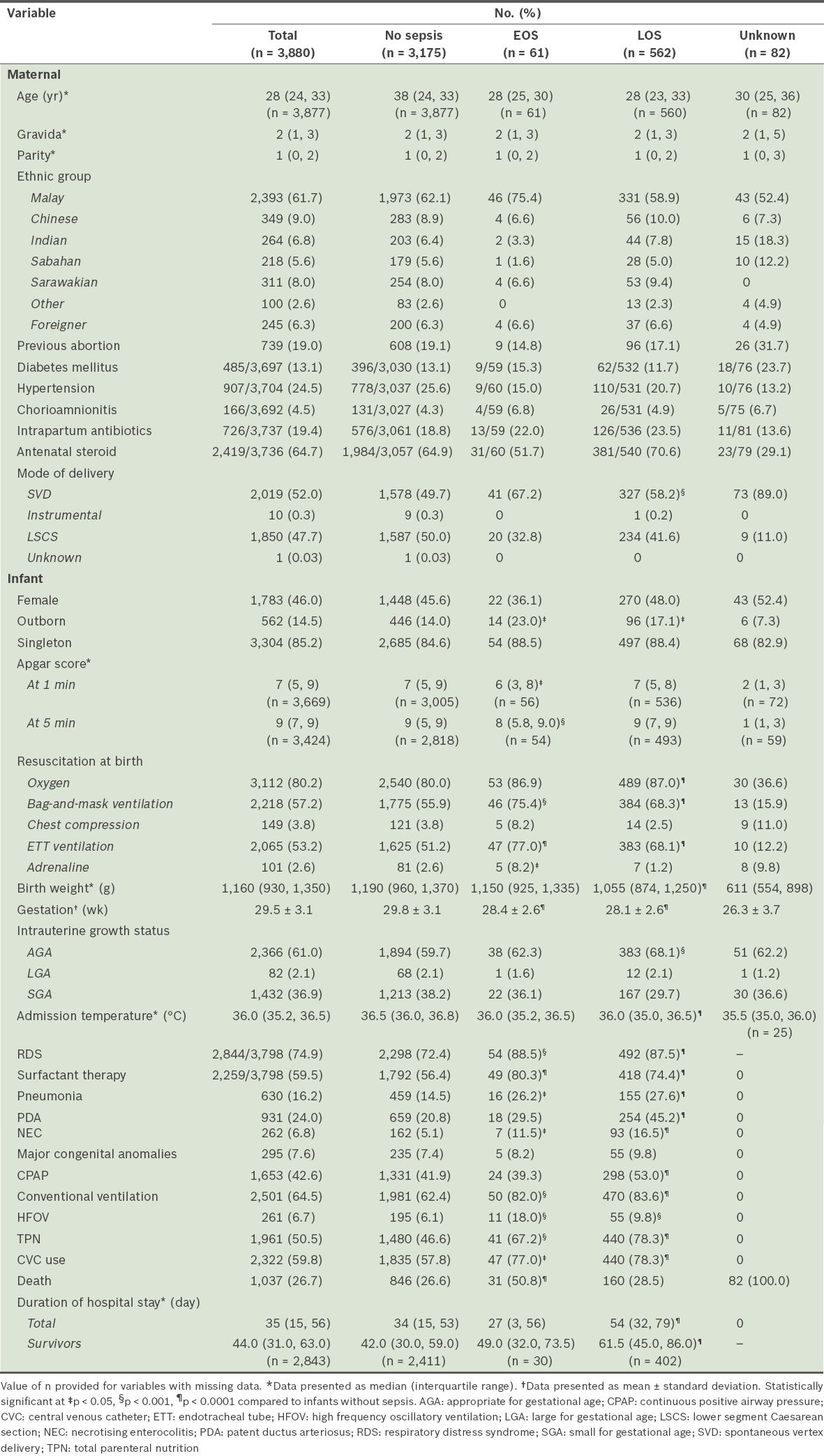
Compared with infants without sepsis (
There were no significant differences in maternal, intrapartum and neonatal variables (
Tables
Table III
Comparison of patient loads of Malaysian neonatal intensive care units (NICUs) with and without early-onset sepsis (EOS) in infants with very low birth weight (VLBW) and extremely low birth weight (ELBW).
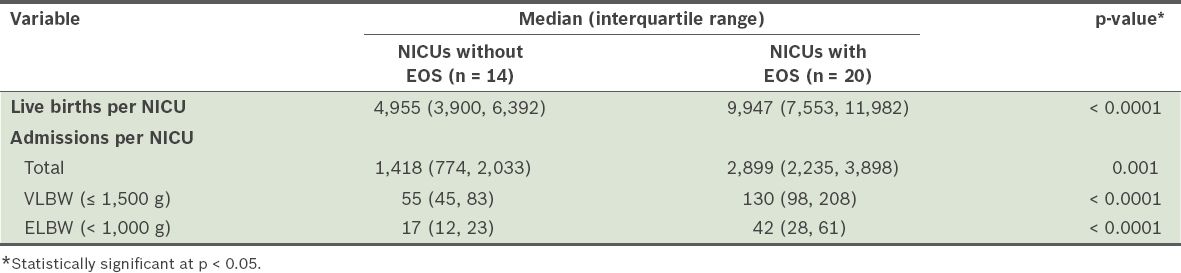
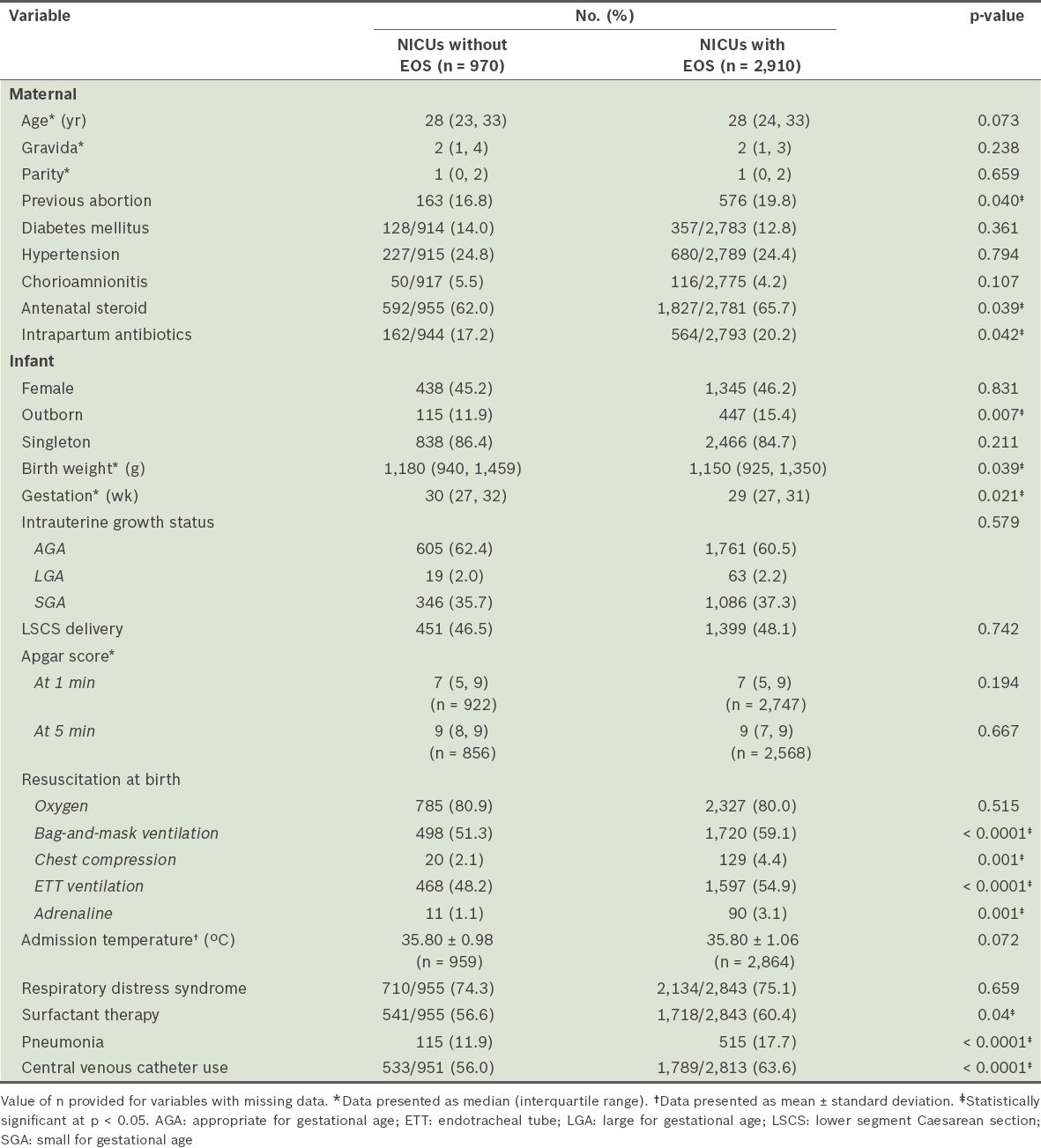
Table IV
Comparison of maternal, perinatal and neonatal variables in very-low-birth-weight infants in Malaysian neonatal intensive care units (NICUs) with and without early-onset sepsis (EOS).
Tables
Table V
Comparison of patient loads of Malaysian neonatal intensive care units (NICUs) with differing late-onset sepsis (LOS) rates in very-low-birth-weight (VLBW) infants.
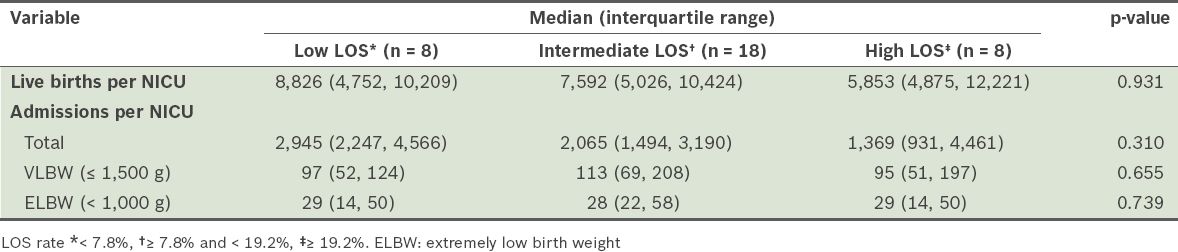
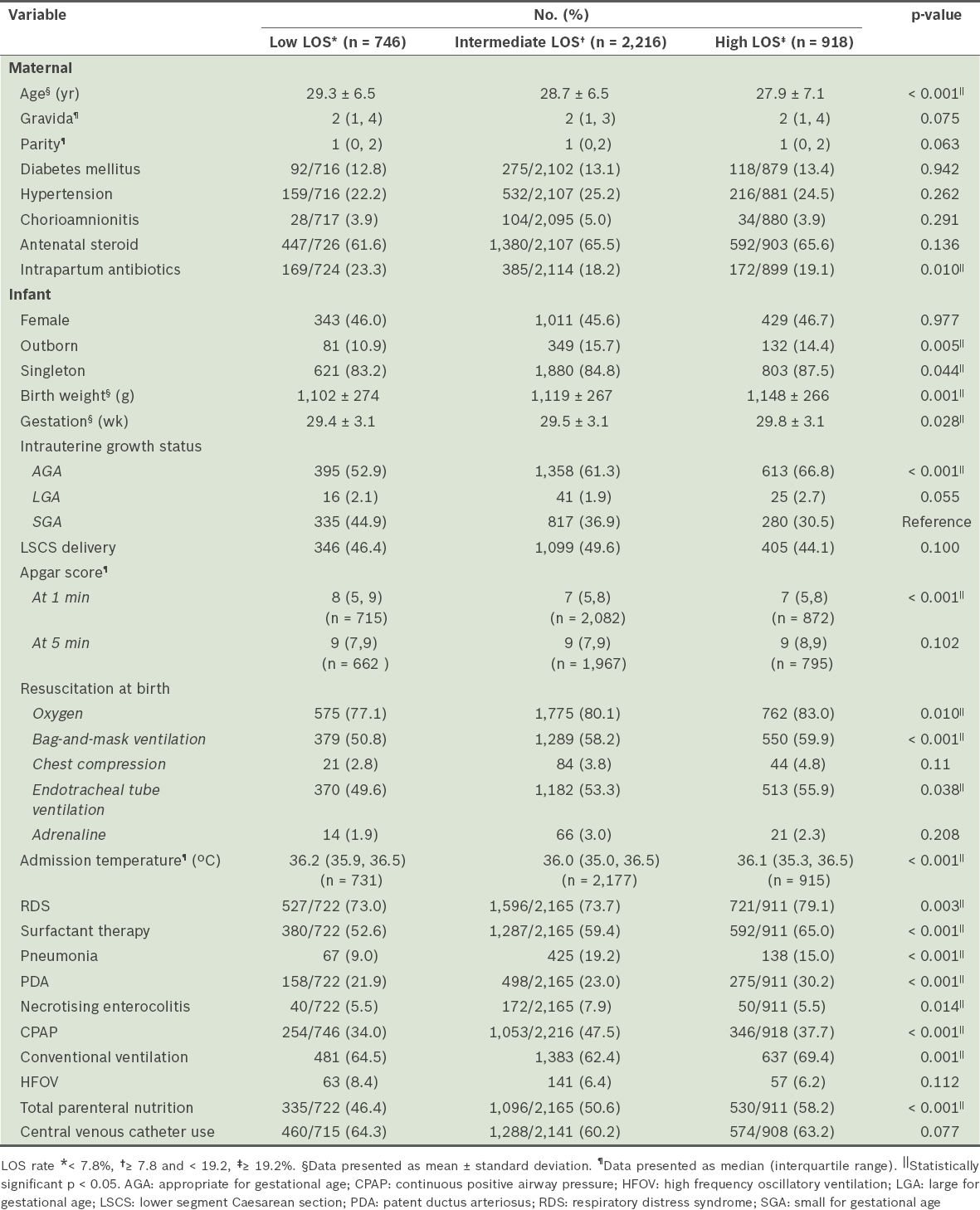
Table VI
Comparison of maternal, perinatal and neonatal variables in Malaysian neonatal intensive care units with differing late-onset sepsis (LOS) rates in very-low-birth-weight infants.
DISCUSSION
This study showed that EOS was not common in Malaysian VLBW infants, but that it had a high mortality rate. The EOS and LOS rates of Malaysian NICUs were comparable with those of some networks/registries,(3,11) but lower than the rates reported by others.(12,13)
Unlike reports in which Gram-negative organisms were the predominant pathogens(3,11,14-16) both Gram-positive and -negative organisms were common EOS pathogens in Malaysian VLBW infants. GBS, the most common pathogen of EOS in our NICUs, produced a higher mortality rate than in other reports.(11,17) Multivariate analysis showed that lower gestational age, resuscitation at birth with ETT ventilation and pneumonia were the only significant risk factors associated with EOS among VLBW infants, compared to those without EOS. Stoll et al have proposed that ascending amniotic infections by maternal vaginal flora are responsible for most cases of EOS.(15) In the present study, we suspect that chorioamnionitis was underreported, as almost a quarter of EOS infants received intrapartum antibiotics.(18) Intrapartum antibiotics have been reported to be effective in the prevention and treatment of chorioamnionitis.(15) Similar to Klinger et al,(18) we found that delivery room ETT ventilation was a significant risk factor for EOS. Compromise of respiratory mucosa due to endotracheal intubation and contamination of the ETT during resuscitation were possible underlying mechanisms of EOS and pneumonia.
Some networks have found that Gram-positive organisms were the most common pathogens of LOS.(1-3,11,12,16,19,20) However, in the current study, both Gram-positive and -negative organisms were found to be common pathogens of LOS, with CoNS being the most common Gram-positive pathogen in Malaysian NICUs. Unlike NICUs in other countries,(1,11,19-21) Escherichia coli was not found to be the most common Gram-negative LOS pathogen in Malaysian NICUs in our study. Fungal infection was also less common (4.7%) than in other networks/registries, which reported an incidence of more than 10.0%.(1,11,12,19,20,22) In our study, multivariate analysis showed that, when compared with VLBW infants without LOS, the significant risk factors associated with VLBW infants with LOS were lower birth weight, SVD, pneumonia, PDA, NEC, CPAP therapy, conventional ventilation and TPN.
This study also showed that there were differences between EOS and LOS infants. EOS infants had significantly lower Apgar scores, hence requiring more extensive resuscitation procedures at birth than LOS infants. However, LOS infants had significantly higher rates of exposure to antenatal steroids, lower admission temperature, more PDA and higher rates of respiratory support. A possible mechanism underlying the increased risk of LOS is the suppression of the immature immune system by antenatal steroids. Generally, infants with hypothermia and PDA necessitated more intervention and a longer duration of respiratory support, which could subsequently contribute to sepsis.
Similar to the findings in other networks,(1,5-7) we also observed a wide variability in sepsis rates. When compared with Malaysian NICUs that reported no EOS in their VLBW infants, those with reported EOS in their VLBW infants had significantly higher patient loads (number of live births, admissions, VLBW and ELBW infants, outborn infants) and more therapeutic interventions at birth (resuscitation procedures, surfactant therapy and insertion of CVCs). Furthermore, they had a significantly larger number of mothers with a previous history of abortions and use of intrapartum antibiotics, suggesting that intrapartum infections were more common among populations giving birth to VLBW infants served by these NICUs. Unfortunately, data on prolonged rupture of membranes and maternal intrapartum fever were not available in the MNNR database. When compared with NICUs with low LOS rates, those with high LOS rates had bigger, more mature infants, more outborn infants, and used less intrapartum antibiotics. These NICUs also had significantly more sick infants (lower one-minute Apgar scores, more resuscitation at birth, lower admission temperature, more RDS, pneumonia and PDA) who required more ventilator support and TPN, which increased their risk of LOS.
A literature review showed that no studies have reported on the association of these risk factors with inter-institutional variability. Our findings suggest that when comparing outcomes of infection control strategies among different NICUs, the factors listed are potential confounders. Therefore, the ability to cope with higher patient loads and improvement of standards of perinatal care are issues that need to be addressed concomitantly when undertaking evidence-based preventive strategies to reduce sepsis rates in Malaysian NICUs.
The limitations of this study include: possible underreporting of LOS, as only the first episode of sepsis was entered in the database; lack of data on the incidence of prolonged rupture of membranes and maternal intrapartum fever; and lack of data on the duration of CVC use, which could be a significant factor associated with inter-institutional variations in sepsis rates.
In conclusion, the current study found that patient loads, patient characteristics and perinatal interventions were significant factors associated with inter-institutional variations of sepsis rates in Malaysian NICUs.
ACKNOWLEDGEMENTS
We would like to thank the Director General of the Ministry of Health, Malaysia, for giving us permission to publish this paper. The following were members of the 2009/2010 Steering Committee of the MNNR: Irene Guat-Sim Cheah, Jimmy Kok-Foo Lee, Thian-Lian Soo, Seok-Chiong Chee, Noraida Ramli, Zuraidah Abdul Latif, Siew-Hong Neoh, Meow-Keong Thong and Nem-Yun Boo. The following were site coordinators of participating hospitals: Zuraidah Abdul Latif (Hospital Ampang), Zainah Shaik Hedra (Hospital Batu Pahat), Ananda Mohan Lal (Hospital Bintulu), Baizura Jamaluddin (Hospital Kajang), Song-Hai Lim (Hospital Keningau), Siew-Hong Neoh (Hospital Kuala Lumpur), Anusha Palakrishanan (Hospital Kuala Pilah), Poy-Lee Leow (Hospital Melaka), Siao-Hean Teh (Miri Hospital), Revathy Nallusamy (Pulau Pinang Hospital), Nor Diana Yahya (Putrajaya Hospital), Noor Khatijah Nurani (Hospital Raja Permaisuri Bainun), Hasmawati Hassan (Hospital Raja Perempuan Zainab II), Maneet Kaur (Sabah Women and Children Hospital), Lee-Gaik Chan (Sarawak General Hospital), Angeline Yeoh (Seberang Jaya Hospital), Rohaizah Borhan (Serdang Hospital), Seok-Chiong Chee (Selayang Hospital), Sow-Keng Chan (Seri Manjung Hospital), Audrey Chae-Hee Chieng (Sibu Hospital), Thiyagar Nadarajah (Hospital Sultan Abdul Halim), Keng-Hwang Teh (Hospital Sultanah Bahiyah), Neesa Amran (Hospital Sultan Haji Ahmad Shah), Unnikrishnan Gopinathan (Sultanah Aminah Hospital), Pui-Ying Tam (Sultanah Fatimah Hospital), Sharifah Huda Engku Alwi (Sultanah Nur Zahirah Hospital), Kwee-Ching See (Sungai Buloh Hospital), Saiful Rijal (Taiping Hospital), Nizam Malik Bali Mohamed (Teluk Intan Hospital), Choy-Nyok Chin (Tengku Ampuan Afzan Hospital), Yogeswary Sithamparanathan (Tengku Ampuan Rahimah Hospital), Hazimah Mohd Yusoff (Tuanku Fauziah Hospital), Umathevi Paramasivam (Tuanku Ja’afar Hospital), Noraida Ramli (Universiti Sains Malaysia Hospital).


