Abstract
INTRODUCTION
The clinical outcomes and factors associated with treatment failure of post-traumatic osteomyelitis have been investigated in many studies. However, limb functionality and quality of life following treatment for this condition have not been thoroughly studied.
METHODS
This cross-sectional study included 47 patients with post-traumatic osteomyelitis of the lower limb. Functional outcome was assessed using the Lower Extremity Functional Score (LEFS), and quality of life was assessed using the validated Malay version of the Short Form-36 questionnaire version 2.
RESULTS
The mean follow-up period was 4.6 (range 2.3–9.5) years, and the median age of the patients was 44 years. Osteomyelitis was located in the tibia for 26 patients and in the femur for 21 patients. Osteomyelitis was consequent to internal infection in 38 patients and due to infected open fractures in nine patients. 42 (89.4%) patients had fracture union and control of infection. Bone defect was found to be a significant contributing factor for treatment failure (p = 0.008). The median LEFS for the success group was 65, compared to 49 for the failure group. Although the success group showed better scores with regard to quality of life, the difference between the two groups was not statistically significant.
CONCLUSION
Treatment of post-traumatic osteomyelitis of the lower limb had a high success rate. The presence of a bone defect was associated with treatment failure. Successfully treated patients had significantly better functional outcomes than in those in whom treatment failed.
INTRODUCTION
The treatment of chronic post-traumatic osteomyelitis (PTO) of long bones is difficult, expensive and lengthy.(1) Treatment includes debridement of the infected bones and unhealthy tissues as well as removal of the implant, adequate and specific antibiotics for the causative micro-organism, good dead space management, and definitive reconstruction after the infection is controlled.(2,3) Treatment success depends on the margin of excision, types of bacteria, physiological status of the host and the site of osteomyelitis.(4,5) The failure rate ranges from 10% to 30%.(4-6)
Many studies have reported on the clinical outcomes, treatment methods and reconstruction techniques for PTO. However, few have examined the functional outcome and quality of life following treatment in these patients.
This study aimed to investigate the clinical and functional outcomes and quality of life in patients treated for PTO of the femur and tibia. The study also identified factors associated with the failure of PTO treatment.
METHODS
A cross-sectional study of patients treated for PTO of the femur or tibia at Hospital Tengku Ampuan Afzan Kuantan, Pahang, Malaysia, was performed from July 2007 to June 2014. Ethics approval was obtained from the institutional research ethics committee (IREC 437).
The diagnosis of osteomyelitis was established based on clinical signs and symptoms, radiographic changes, intraoperative findings and bacteriological cultures. The clinical signs and symptoms included low-grade fever with chronic bone pain, redness, swelling and the presence of sinus tracts. Plain radiographic features included periosteal reactions or osteopenia. Intraoperative findings included the presence of pus, loosening of the implant and the presence of sequestrum or cloaca.
Patients who had haematogenous osteomyelitis or malignancy, those who did not complete the treatment or those who had less than two years of follow-up were excluded from the study.
The sample size was calculated using a single proportion formula assuming treatment failure of 10%, with a margin of error 10%, based on a study by Gonzalez and Weinzweig.(7) This gave a sample size of 35 patients at 95% confidence level. Assuming a response rate of 60%, the minimum total number of patients required for the study was set at 50.
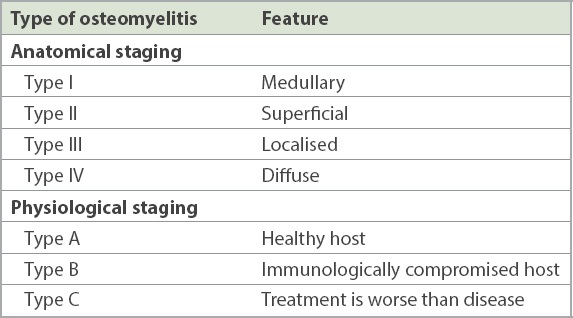
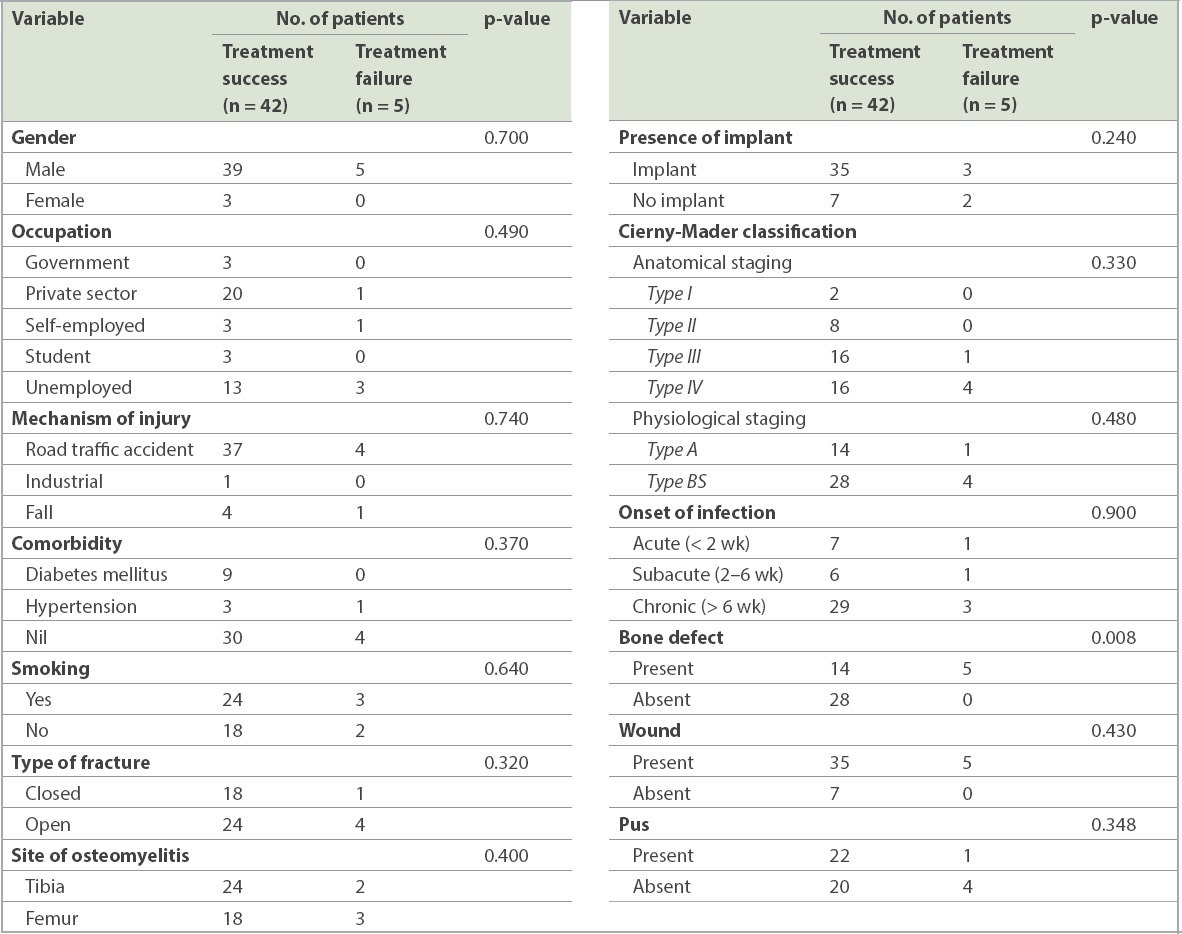
A total of 57 patients fulfilled the inclusion and exclusion criteria. However, ten patients failed to attend the final assessment, leaving 47 patients in the study. The following predictive factors were analysed: age; gender; occupation; mechanism of injury; underlying medical problems or comorbidities; smoking habit; type of fractures (open or closed); site of osteomyelitis; presence of a metal implant; onset of symptoms; presence of a wound, pus or bone defect; and categorisation of osteomyelitis according to the Cierny-Mader classification. The onset of infection was divided into: acute, when the infection occurred within two weeks of injury or surgery; subacute, when the infection occurred between two and six weeks of injury or surgery; and chronic, when the infection occurred after six weeks of injury or surgery. The Cierny-Mader classification is divided into two categories to incorporate anatomic and physiological status (
Table I
Cierny-Mader classification of osteomyelitis.
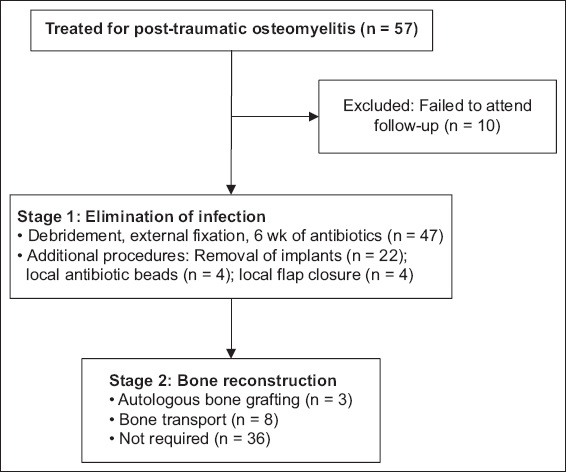
PTO was managed in two stages (
Fig. 1
Flowchart shows distribution of 57 patients treated for post-traumatic osteomyelitis.
During patient review, a physical examination was performed to evaluate the clinical outcome of the procedures. The success of treatment was established when participants demonstrated fracture union, with a stable wound and absence of infection.(7) Union was defined as the ability to bear weight without pain, with radiological evidence of fracture union.(8) Failure of treatment was established when participants had non-union and/or infection.(7)
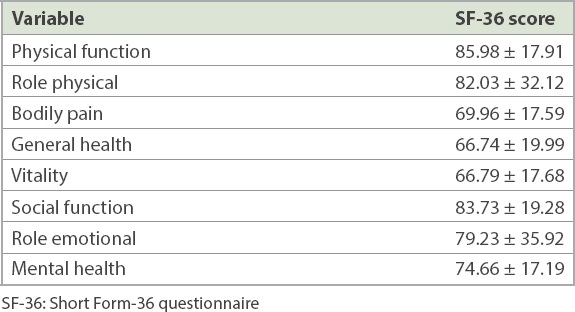
Once consent was obtained for the study, patients were provided two sets of questionnaires. The first one was the Short Form-36 version 2 (SF-36v2) questionnaire to assess quality of life, which had been translated and validated in the Malay language.(9) Patients were assessed by an author not involved in their clinical management.
SF-36 is a generic outcome tool with 36 questions related to physical and mental health. The physical health components included physical function, physical role, bodily pain and general health. The mental health component contained four measurements: vitality, social functioning, emotional role and mental health. Scoring was performed by entering data using the QualityMetric Health Outcomes™ scoring software 4.5 (QualityMetric Incorporated, Lincoln, RI, USA). The software produced a T-score based on the mean and standard deviation of the 2009 United States (US) general population. Scores below 50 were interpreted as below those of the US general population, and scores above 50 were interpreted as above those of the US general population.
The second questionnaire was the Lower Extremity Functional Score (LEFS), which contained 20 questions regarding the participant’s ability to perform everyday tasks. The maximum score was 80, and lower scores indicated an increasing disability. LEFS was sensitive to changes in participants’ physical function and was easy to administer and score.(10)
The questionnaire results were calculated using the scoring system and analysed with IBM SPSS Statistics for Windows version 21.0 (IBM Corp, Armonk, NY, USA) using the Spearman correlation test, Mann-Whitney U test, Kruskal-Wallis test and UNIANOVA. Median and interquartile ranges were calculated for all data.
RESULTS
Patients were followed up for a mean duration of 4.6 (range 2.3–9.5) years. The median age of the patients was 44 years, with an interquartile range of 31 years. A majority of the patients were male (n = 44, 93.6%) and only 3 (6.4%) were female (
Table II
Treatment outcome based on patient factors.
The most common comorbidities observed were diabetes mellitus (n = 9, 19.1%) and hypertension (n = 4, 8.5%). More than half of the patients were smokers (n = 27, 57.4%).
The fracture profile showed that a majority of patients (n = 41, 87.2%) sustained PTO due to traffic accidents. Only 1 (2.1%) patient had an industrial injury and another 5 (10.6%) patients were injured in a fall. Slightly more than half of our patients (n = 28, 59.6%) sustained an open fracture, while the rest had a closed fracture (n = 19, 40.4%). The incidence of tibia fracture was slightly higher (n = 26, 55.3%) than the incidence of femur fracture (n = 21, 44.7%). Also, a majority of patients (n = 38, 80.9%) received an implant: either a plate (66%) or an intramedullary device (34%).
In general, more than two-thirds of patients (n = 32, 68.1%) were classified as Cierny-Mader type B, with Cierny-Mader type A making up the rest (n = 15, 31.9%). No patient was classified as Cierny-Mader type C. Anatomically, a majority of patients were classified as Cierny-Mader type IV (n = 20, 42.6%), followed by Cierny-Mader type III (n = 17, 36.2%), Cierny-Mader type II (n = 8, 17.0%) and Cierny-Mader type I (n = 2, 4.3%). A majority of participants (n = 32, 68.1%) presented after six weeks of infection or had infections that were chronic in nature.
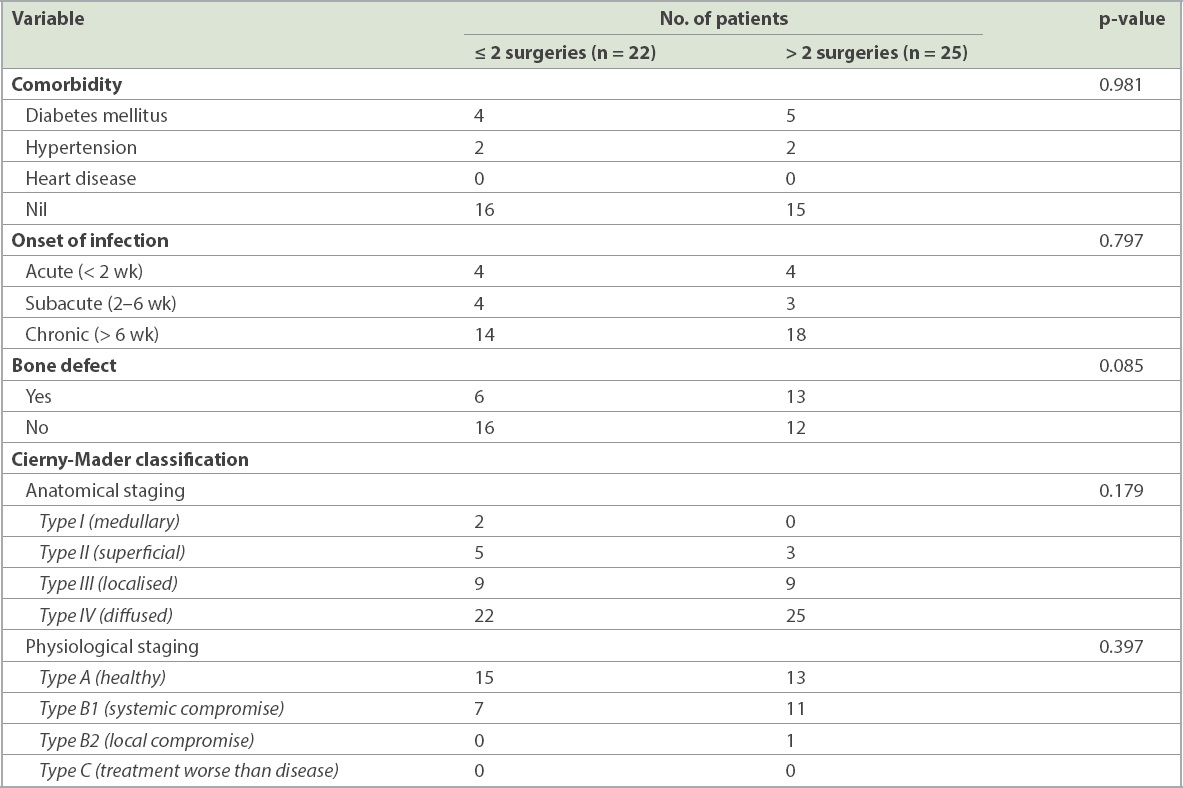
Overall, 22 (46.8%) patients had two or fewer surgeries when compared to 25 (53.2%) patients, who had more than two surgeries (
Table III
Association of patient factors and the number of surgeries performed.
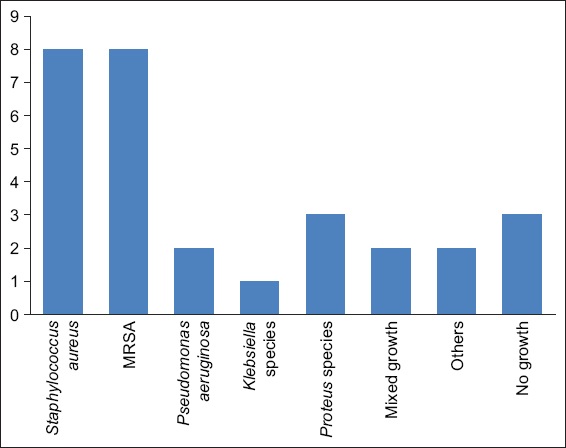
Microbiology results were available for 29 patients. The two most common micro-organisms isolated were Staphylococcus aureus and methicillin-resistant Staphylococcus aureus. Other micro-organisms cultured included Pseudomonas aeruginosa, Klebsiella species, Proteus species, Enterobacter species, Acinetobacter baumannii and mixed growth (
Fig. 2
Chart shows the microbiological results of 29 patients. MRSA: methicillin-resistant Staphylococcus aureus. Others: Enterobacter species (n = 1), Acinetobacter baumannii (n = 1)
In our study, 42 (89.4%) patients demonstrated fracture union and infection control. Only 5 (10.6%) patients had failure of treatment (or non-union with or without infection). Two patients had infected non-union, two patients had non-union with control of infection and one patient had fracture union with persistent infection.
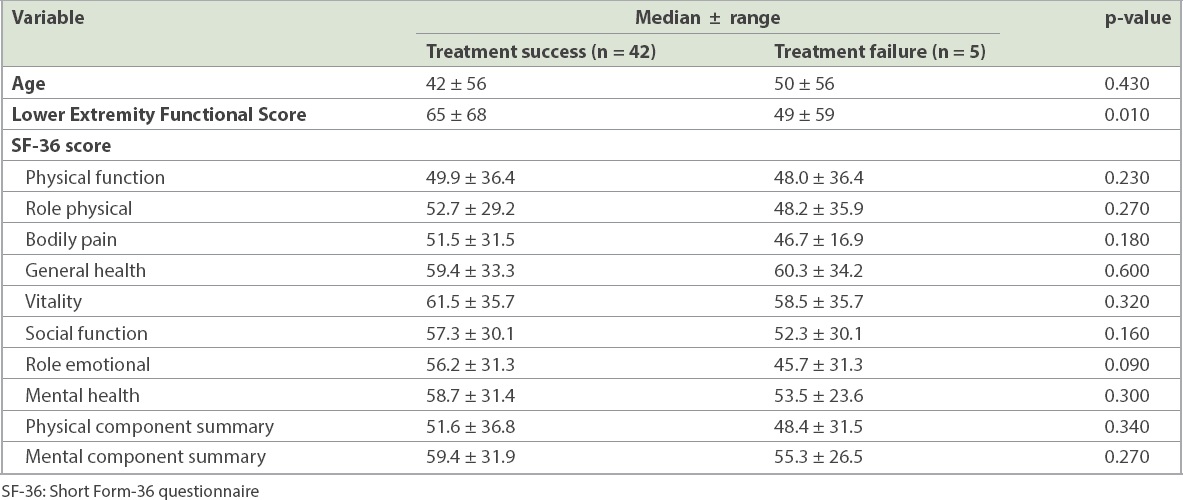
Age of patients was not associated with treatment failure (
Table IV
Functional outcome and quality of life of patients based on treatment outcome.
DISCUSSION
Nearly 90% of patients with PTO in our study had a successful clinical outcome. This result was similar to other studies that described a failure rate of approximately 10%–30%.(6,7) At long-term follow-up, Egol et al achieved a 94% success rate in their study population (n = 43).(11) Tice et al documented that their success rate following treatment was only 69.4% in a much larger population, with a sample size of 454 patients.(12) Jorge et al achieved only an 80% success rate for 193 patients with PTO, while Liener et al achieved a success rate of 88%.(13)
We found that the presence of a bone defect was the only significant factor associated with treatment failure. Tice et al reported that P. aeruginosa infection and treatment with vancomycin were important factors for the recurrence of osteomyelitis.(12) Jorge et al reported that P. aeruginosa infection was a significant factor for recurrence.(14) They noted that elderly patients and intraoperative blood transfusion were also independently associated with the recurrence of PTO. There were only two patients with PTO caused by P. aeruginosa, with one failure. Gonzalez and Weinzweig found that diffuse osteomyelitis (Cierny-Mader type IV) was a significant factor for treatment failure.(7) Impaired host factor (Cierny-Mader type B) was an important variable for failure in some studies.(4,7)
We observed that the LEFS of patients who had successful treatment was significantly better than that of patients whose treatment failed. The LEFS of our successful patients was better (median 65) when compared to the results of Schep et al, who reported an LEFS of 47 for bone transport and 61 for lengthening.(15) Campbell et al reported an average LEFS of 51 among 12 patients treated for tibial osteomyelitis.(16) Egol et al noted that following eradication of osteomyelitis, patients’ function was not significantly different from that of the normal population when measured using the Short Musculoskeletal Functional Assessment.(11) Unfortunately, we were unable to compare our findings with those of the normal population owing to unavailability of these values.
The quality of life of patients who were successfully treated was not significantly different from that of patients whose treatment failed. However, these values were lower than the SF-36 values of the normal Malaysian population (
In conclusion, the success rate for PTO in the lower limb was high in our cohort of patients. The presence of a bone defect was associated with treatment failure. The functional outcome of successfully treated patients was significantly better than that of patients with treatment failure. However, the difference in quality of life was not statistically significant between the two groups.
About the Second Author

Prof Dr Nazri Mohd Yusof is an Advanced and Trauma Limb Reconstruction Surgeon at the Sultan Ahmad Shah Medical Centre @IIUM (International Islamic University Malaysia). His special interest is in the management of severe long bone open fracture of lower limbs and fracture-related infections. He is actively involved in the education and training programme on the Ilizarov technique and deformity correction.