Elvis, a 62-year-old man, visited your clinic for his diabetes mellitus and gout follow-up. You wondered how his right knee pain was and whether it might have been affecting his delivery work, which involved carrying heavy goods in and out of a truck. He often lamented that he was not as fit as he used to be and had stopped all impact sports after his right knee injury ten years ago. He said that his right knee pain and swelling were limiting his climb up and down his truck and asked for analgesia.
WHAT IS KNEE SWELLING?
The normal knee joint contains 2–3 mL of synovial fluid that lines its articulating surfaces. Knee swelling is a common presentation for knee pathology and can be generalised or localised. A generalised swelling occurs when the joint cavity is filled with excess joint fluid in response to knee pathologies such as fracture (trauma), septic arthritis (infection) or inflammation (gout, osteoarthritis). Examples of common, localised knee swelling include bruise, haematoma (trauma), abscess (infection), cyst (meniscus, sebaceous, popliteal) or lipoma (
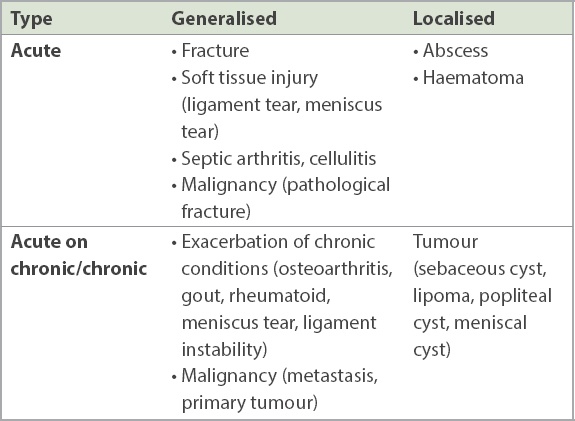
Table I
Causes of knee swelling.
HOW RELEVANT IS THIS TO MY PRACTICE?
In the primary care setting, a generalised swelling can present as an early symptom for various knee pathologies. It is important to differentiate the urgent conditions from the rest, as timely management can change the course of the disease. Urgent conditions include fractures, infections (abscess and septic arthritis) and malignancy (musculoskeletal). These three conditions require timely specialist referral and likely surgical intervention.(1)
The causes of generalised knee swelling can be classified into acute and acute-on-chronic (
WHAT CAN I DO IN MY PRACTICE?
History
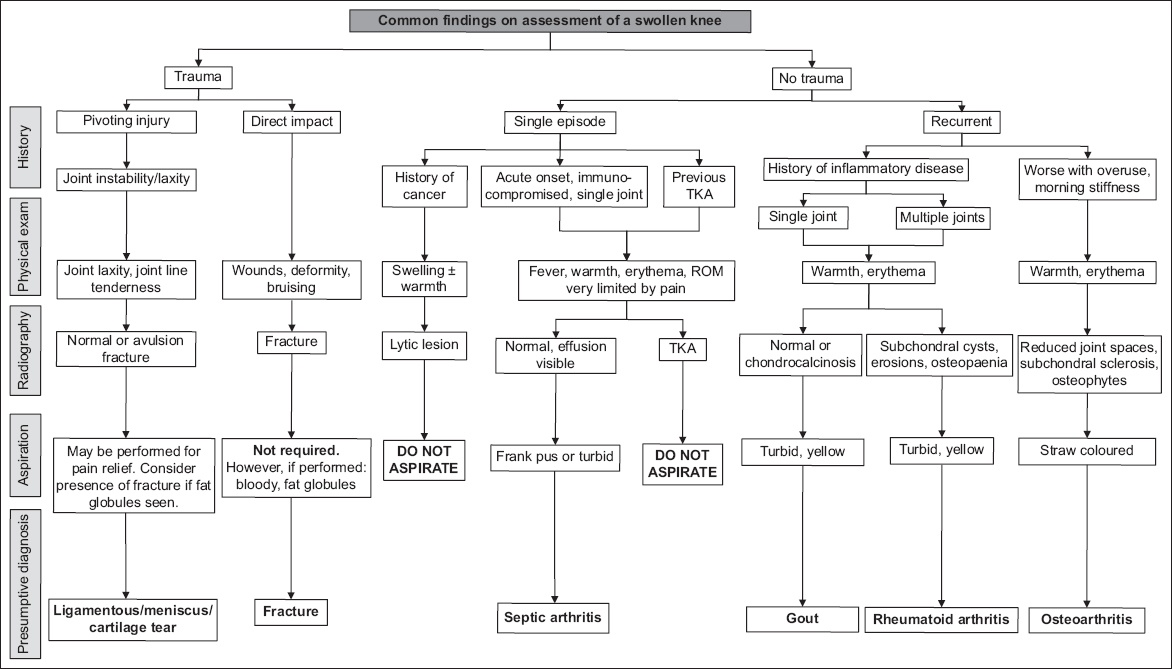
A thorough history will provide valuable diagnostic clues. The following demonstrates possible common aetiologies that may be elicited with comprehensive clerking (
Fig. 1
Flowchart shows common findings on assessment of a generalised swollen knee. ROM: range of motion; TKA: total knee arthroplasty
Acute onset
In patients with a history of trauma, important considerations would include fractures or soft tissue injuries such as tears of the anterior cruciate ligament or meniscus, and cartilage injury. An example is a sports injury. The onset of swelling can be immediate or delayed. In elderly patients with osteoporotic bone, a fracture needs to be excluded, although the trauma might be mild.
Another possible aetiology is infection (septic arthritis). Predisposing factors include a history of diabetes mellitus and immunosuppressive medications such as steroids. Other known causes are poor surrounding skin conditions such as chronic eczema, a recent infection such as pneumonia and penetrating injury to the knee. Septic arthritis is an orthopaedic emergency and carries a guarded prognosis. The chance of a good outcome dwindles with a delayed diagnosis.
Although tumours are not common, this differential diagnosis needs to be considered in a patient with a positive history of cancer, and the risk of metastasis needs to be excluded. Tumours usually present with night or rest pain and are not relieved by analgesia. The patient might have a low-grade fever as the sole presenting symptom.
Acute-on-chronic/chronic onset
The presence of inflammatory conditions can be a diagnostic clue. An attack of gout, a common inflammatory condition, classically presents as a swollen first metatarsophalangeal joint. It can also present as a swollen knee joint.(2) An accurate diagnosis is difficult after a first attack. However, in a patient with a history of gout, it is usually possible to confirm the diagnosis based on a similar past experience. There is usually a precipitating factor, such as dietary non-compliance with high-purine foods such as alcohol and peanuts.(2) Rheumatoid arthritis or other systemic inflammatory joint conditions can present as monoarticular arthritis with low-grade fever, pain and swelling.(2) Young female patients may have a predilection to developing such inflammatory arthropathies, and a first presentation in this patient demographic might warrant a diagnostic work-up after the treatment of the initial knee swelling. Specific diagnostic criteria for inflammatory joint conditions is beyond the scope of this article.
Degenerative changes in the knee such as cartilage and meniscal tears may be present in patients aged more than 40 years. These present as pain and swelling following weight-bearing activities, with minimal or no trauma involved. Patients tend to have no systemic symptoms and may report symptoms of intermittent acute synovitis.(3,4)
Post-surgery patients such as those who had a total knee replacement or other metal implants placed in the knee may also present with knee swelling. It is important to determine whether the swelling is a postoperative swelling, which can be present for a few months after surgery. Knee swelling after a physiotherapy session can also be associated with tightness and pain. A key differentiating factor is that this resolves with rest, in comparison to a prosthetic joint infection or fracture, which is unlikely to improve. If the diagnosis warrants an urgent review, the patient should be sent to the emergency department (ED). If there are concerns about other postoperative complications, patients should be advised to contact their surgeon’s clinic for an early appointment.
Physical examination
An accurate physical examination is important for proper treatment, as a generalised knee swelling could have various causes. In a suspected fracture or soft tissue injury, the patient shows limited movement at the knee and weight bearing is limited. There may be bruising, obvious deformity or tenderness on examination. It is always important to examine the joint above and the joint below to assess for any other associated injuries.(5)
In septic arthritis, the knee is intensely swollen and the skin is ‘shiny’. There might be a history of innocuous penetrating injury by a sharp object such as a needle. The patient is unable to mobilise the knee and it is very tender (the patient is likely to stop the physician from touching the knee).(3) He/she is unable to weight bear and experiences pain at rest.(6) The patient usually has a high fever and is septic. It might be difficult to differentiate a gout attack from septic arthritis, as the patient also presents with a tense and angry-looking knee.
In established knee osteoarthritis, there are obvious features such as knee deformity and limited range of motion, especially in the late stages of the disease. However, such signs might not be obvious in the early stages of the disease.(4) In the rare cases of a malignancy, a palpable mass might be present. It can also present as a pathological fracture.(6)
Investigations and scans
Blood tests, radiographic imaging and, in some cases, knee aspiration can be useful for providing additional information in the work-up of a swollen knee.
Blood tests can provide useful information in the work-up for septic arthritis, as the white blood cell count tends to be markedly raised (> 20.0 × 109/L). However, blood testing alone is not specific, as the white blood cell count can also be raised in gout attacks, osteoarthritis exacerbation and trauma, although the increase is less significant (< 20.0 × 109/L) in these conditions.
Plain radiographs are often useful for assessing a swollen knee, particularly in looking for fractures, gas shadows or the presence of radio-opaque implants. The most commonly used views are the anteroposterior (AP), lateral and skyline views. Weight-bearing AP views should be obtained, especially when osteoarthritis is suspected.(5,7) However, in an acute exacerbation, patients are in pain and it might not be possible for them to stand comfortably for this view to be performed. In a knee with early degeneration, the radiographs might be normal, with no significant arthritic changes such as osteophytes.(4) Magnetic resonance imaging might be indicated in selected patients, such as those with a suspected degenerated meniscus that is persistently symptomatic, to discuss further treatment.(1)
A skyline view radiograph is needed for a patient with anterior knee pain or patellofemoral osteoarthritis. This should also be done if there is a history of trauma to the knee, to exclude a vertical fracture in the patella.
In a ligament, meniscus or cartilage injury, plain radiographs may appear normal. An avulsion fracture, such as that of the tibial spine, raises the suspicion of an anterior cruciate ligament injury.(3)
Knee aspiration can be both diagnostic and therapeutic. It can provide symptomatic relief of conditions such as effusion from an exacerbation of osteoarthritis or haemarthrosis in a soft tissue injury (e.g. anterior cruciate ligament tear). Practitioners should bear in mind that aspiration has its risks and should be considered only if a benign diagnosis is certain. If in doubt, the patient should be sent to the ED for further management. It is important to note that an aspiration must not be done in: (a) the presence of cellulitis or other infective skin changes on the knee, as this can result in septic arthritis; or (b) a patient with a prosthetic joint. A resultant periprosthetic joint infection is a serious adverse outcome. Any finding needs to be interpreted in correlation with the clinical picture.
Common findings(7) are as follows (pictorial references for each aspirate characteristic can be found in the study by Courtney and Doherty(8)):
-
Blood – This is seen in traumas such as an anterior cruciate ligament tear. A fracture needs to be excluded when fat globules (from the bone marrow) are present.(5,7)
-
Pus or turbid fluid – It is not always frank pus. The possibility of septic arthritis cannot be excluded in the presence of turbid fluid in the context of fever and elevated total white blood cell count. Turbid or mildly clouded aspirate might be present in inflammatory conditions such as rheumatoid arthritis or gout.(2,3)
-
Straw-coloured fluid – This is seen in exacerbation of degenerative arthritis, or meniscus or cartilage injury.(9)
The aspirated sample should be sent for Gram stain, microscopy and culture. In septic arthritis, a bacterial infection is confirmed when all three are positive, while gout is diagnosed when the microscopy shows crystal formation. Aspiration is a helpful tool provided that the indications are right and there is access to a laboratory.
Follow-up visit
After the knee swelling has settled, the patient should be encouraged to maintain good knee health and reverse deconditioning. General knee health advice includes:
-
Exercise – Resources such as the ActiveSG website provide simple exercises that patients can follow in the comfort of their own home. The Health Promotion Board’s Healthy 365 application can link patients to ‘Active Ageing’ programmes near them. Other resources include physiotherapy, which is available in some polyclinics.
-
Proper footwear – Patients should be advised to choose shoes that fit well and have good support.
- Maintaining a healthy weight
WHEN SHOULD I REFER THE PATIENT?
Referral to emergency department
Urgent orthopaedic conditions such as a fracture and septic arthritis need to be referred to the ED. A patient with an acute knee swelling associated with constitutional symptoms such as fever or night pain needs a specialist review to exclude the possibility of septic arthritis.
A knee swelling may be difficult to characterise in a patient who recently had knee surgery, as postoperative swelling is expected in the initial months. However, postoperative swelling is usually associated with pain and a limited range of movement, which improve with time and do not require a hospital referral. However, when there is an objective fever or a suspicion of periprosthetic joint infection, the patient needs an urgent referral back to the hospital where the initial surgery was performed. When in doubt, the patient should be referred to the ED.
Referral to orthopaedic clinic
A soft tissue injury with suggestion of ligament or meniscus tear with persistent or worsening symptoms (without suspicion of the aforementioned urgent conditions) would benefit from an orthopaedic opinion. Similarly, a patient with knee osteoarthritis who is considering surgical intervention would benefit from an orthopaedic opinion. Otherwise, a trial of conservative management with pain relief and physiotherapy should be prescribed.
The various knee conditions can be triaged to different specialists, including sports medicine or rheumatology, depending on the working diagnosis.
TAKE HOME MESSAGES
- When faced with a generalised knee swelling, the physician must first ascertain the speed of onset of the swelling. This helps to narrow down the differential diagnoses.
- Red flags in a patient’s history include fever, immunocompromised state, minor trauma in the elderly with osteoporotic bone, loss of weight, loss of appetite, night sweats, night pain and presence of knee prostheses. On examination, the physician should watch out for severe pain, an intensely swollen knee, ‘shiny skin’ and limited range of motion (suggestive of septic arthritis). Investigations showing raised infective markers or fractures on radiographs should also prompt urgent referral.
- AP and lateral view radiographs are recommended to identify fractures, gas shadows and radio-opaque implants. Skyline views should be included if there is a history of knee trauma or any suspicion of patellar pathology. The possibility of soft tissue injury should be considered even if the radiographs are normal.
- Aspiration can be diagnostic or therapeutic. Depending on the practitioner’s experience and assessment, therapeutic aspiration can be performed for benign knee swellings in primary care, but patients should be referred to the ED in case of any doubt.
- Urgent differentials that should prompt an immediate referral to the ED include septic arthritis, periprosthetic joint infection, malignancy and fractures. Other conditions that might warrant surgical intervention such as osteoarthritis and ligamentous injuries can be referred to the orthopaedic clinic.
You found that Elvis’ history and clinical examination were reassuring. His pain was chronic, with no red flag symptoms of night pain, rest pain, recent trauma or predisposing factors for infection. On examination, he was afebrile and had ambulated into the clinic, albeit with an antalgic gait. His knee range of motion was limited by pain. Blood investigations and a knee aspiration performed ruled out septic arthritis. Radiography showed degenerative changes. Elvis was prescribed a short course of anti-inflammatories and analgesics for pain control. He was counselled on the importance of weight control and wearing appropriate footwear, and referred for physiotherapy, including aqua aerobics. A month later, he was happy to report that his knee symptoms had resolved and he had returned to work.
SMJ-63-191.pdf


