Abstract
The Health Promotion Board (HPB) has developed the Clinical Practice Guidelines (CPG) on Obesity to provide health professionals in Singapore with recommendations for evidence-based interventions for obesity. This article summarises the introduction, epidemiology and executive summary of the key recommendations from the HPB-MOH CPG on Obesity for the information of SMJ readers. The chapters and page numbers mentioned in the reproduced extract refer to the full text of the guidelines, which are available from the Health Promotion Board website:
INTRODUCTION
1.1 Objective of the guidelines
This Clinical Practice Guidelines (CPG) on Obesity is an update of the Obesity CPG developed by the Ministry of Health in 2004. The revised guidelines aim to provide health and allied healthcare professionals updated, evidence-based recommendations to support effective interventions to manage obesity.
These guidelines are not to be viewed as a protocol, but they provide a framework to:
assist health and allied healthcare professionals in the management of overweight and obesity in the community and clinical setting;
provide an update of various lifestyle, behavioural, medical, surgical and ancillary intervention modalities in the management of obesity; and
address the management concerns of specific populations (e.g. children, adolescents, pregnant women).
1.2 Target users
These guidelines are intended for all medical and allied healthcare professionals who have a role in managing overweight or obese patients. This includes medical professionals such as general practitioners, endocrinologists, paediatricians, surgeons, family physicians, advanced practice nurse clinicians, as well as allied healthcare professionals such as nutritionists, dietitians, pharmacists, exercise and behavioural therapists.
1.3 The epidemiology of obesity
Obesity can be defined as a condition of abnormal or excessive accumulation of body fat to the extent that health may be adversely affected, and is associated with various major chronic diseases including cardiovascular disease, Type 2 diabetes and cancer.
1.3.1 Overweight and obesity in Singaporean adults
The prevalence of overweight (body mass index [BMI] ≥ 25 kg/m2) among all Singapore adults in 2013 was 34.3% with 40.2% of males and 28.6% of females considered overweight. The prevalence of pre-obesity (BMI 25–29.9 kg/m2) was 25.7% and was also higher in males (30.8%) than in females (20.7%).
The prevalence of obesity (BMI ≥ 30 kg/m2) among Singapore adults is on an upward trend, increasing from 5.5% in 1992 to 8.6% in 2013 (
Fig. 1
Age-standardised prevalence of obesity (BMI≥30 kg/m2) in Singapore adults (1992–2013) [Ministry of Health, Singapore. National Health Survey 1992, 1998, 2004 & 2010; National Health Surveillance Survey 2013. 2013 data is not directly comparable with previous years’ due to differences in research methodology].
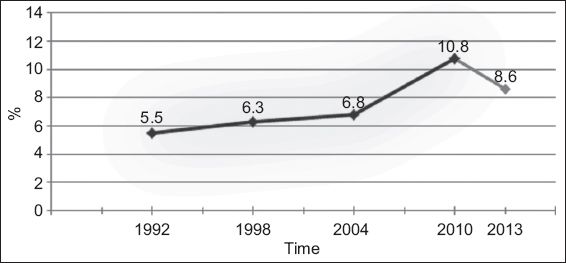
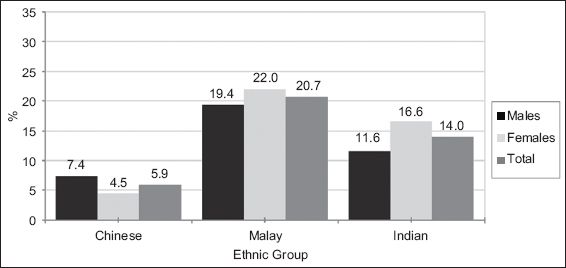
Fig. 2
Crude prevalence of obesity (BMI ≥ 30 kg/m2) among Singapore residents aged 18–69 years, by gender and ethnic group in 2013 [Ministry of Health, Singapore. National Health Surveillance Survey 2013].
The World Health Organization (WHO) has revised the BMI risk categories for cardiovascular disease and diabetes in Asian populations into low-risk (18.5–22.9 kg/m2), moderate-risk (23.0–27.4 kg/m2) and high-risk (≥ 27.5kg/m2). Based on these categories, 39.7% of Singapore adults aged 18–69 years have a low-risk BMI, 34.8% have a moderate-risk BMI (
Fig. 3
Prevalence of moderate-risk BMI among Singapore adults by gender and ethnic group in 2013 [Ministry of Health, Singapore. National Health Surveillance Survey 2013].
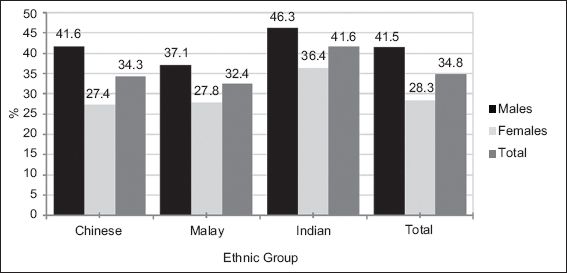
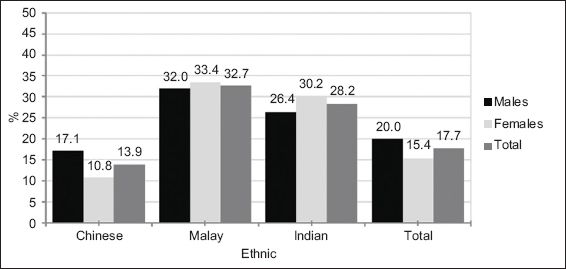
Fig. 4
Prevalence of high-risk BMI among Singapore adults by gender and ethnic group in 2013 [Ministry of Health, Singapore. National Health Surveillance Survey 2013].
1.3.2 Obesity in childhood and adolescence in Singapore
The prevalence of childhood overweight/obesity has increased worldwide over the past few decades, though there are signs of stabilisation in some age groups of children in certain countries. In Singapore, a review of eight anthropometric studies conducted over the past five decades (from 1957 to 2002) found that although the height of pre-schoolers and school-age children appeared to have optimised according to their genetic potential, their weight was found to be still increasing, and as such BMI was also increasing.
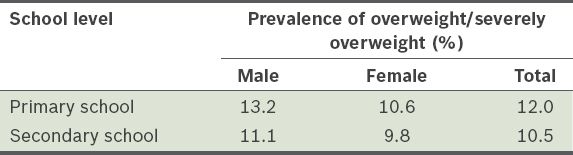
From July 2010, BMI-for-age norms replaced the weight-for-height norms measures in schools. As both measures are different, direct comparison between 2010 statistics and those from earlier years cannot be made for trend analysis. Using the BMI-for-age norm, the prevalence of overweight/severely overweight for students in primary and secondary schools in Singapore for 2010 is shown in
Table I
Prevalence of overweight/severely overweight among students in primary and secondary schools in Singapore, 2010.
Childhood overweight/obesity is a public health concern given the adverse effects on the health and quality of life in childhood, as well as the increased risk of obesity and associated health complications in adulthood.
1.4 Conclusion
Overweight and obesity are growing problems in Singapore adults and in children and adolescents. Strategies for our population are required to address this rising trend so as to reduce the morbidity and mortality rate attributable to obesity.
EXECUTIVE SUMMARY OF KEY GUIDELINE RECOMMENDATIONS
Details of recommendations are located in the main text at the pages indicated.
Diagnosis and Classification
C
Current WHO and international guidelines recommend BMI cut-offs of 25 kg/m2 and 30 kg/m2 to define overweight and obesity, respectively. Based on body fat equivalence and comorbid disease risk, BMIs of 23 kg/m2 and 27.5 kg/m2, respectively, have been recommended as the cut-off points for public health action in Asians (pg 32).
Grade C, Level 2+
C
Waist circumference is the most practical anthropometric measurement for assessing a patient’s abdominal fat content before and during weight loss treatment, and should be used in conjunction with BMI to identify increased disease risk. The current international guidelines recommend waist circumference cut-offs of 102 cm and 88 cm to define excess risk in males and females, respectively. Based on an Asian-Pacific consensus, cut-offs of 90 cm and 80 cm, respectively, may be more appropriate for Asians (pg 34).
Grade C, Level 2+
Assessment
GPP
In clinical evaluation of patients, practitioners should consider and exclude predisposing factors for and secondary causes of obesity (pg 37).
GPP
C
Overweight and obese adults should be screened for comorbid conditions, and should be stratified according to their health risks, in particular for cardiovascular disease, prior to the commencement of treatment (pg 38).
Grade C, Level 2+
GPP
Table
Clinical and laboratory assessment (pg 38).
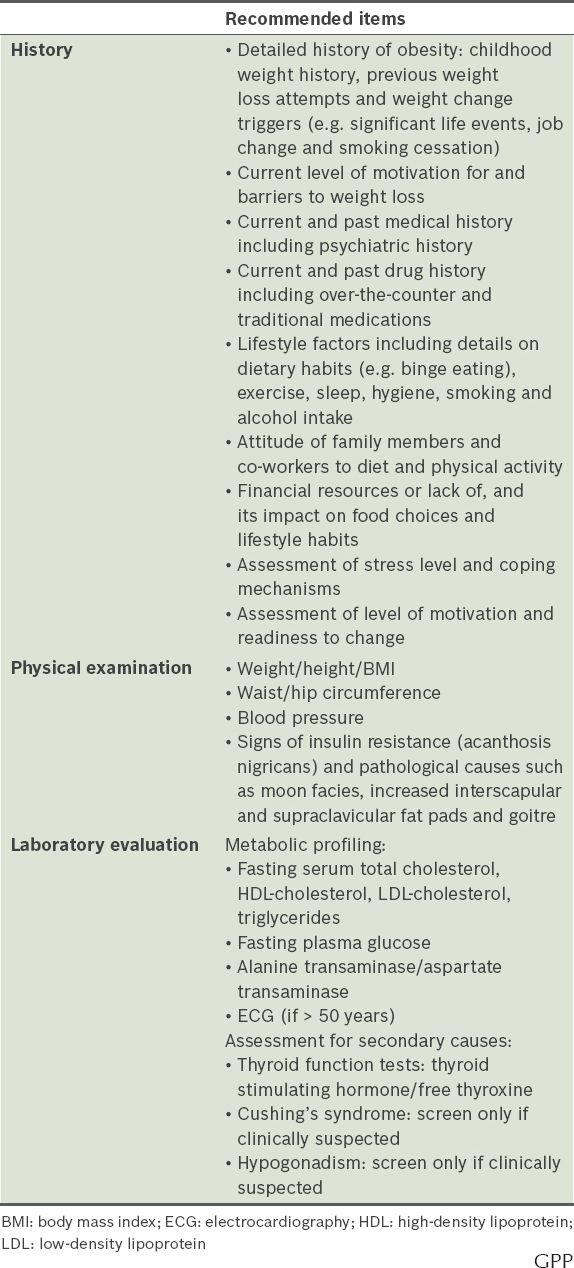
GPP
C
Patient motivation – an important prerequisite in weight loss management – should be relatively high before initiating therapy. Proper evaluation of issues related to motivation should be undertaken (pg 40).
Grade C, Level 2+
Treatment: Introduction
A
A multi-faceted or a multi-disciplinary strategy should be utilised to achieve and maintain weight loss. This could be adequately achieved at the primary health care level depending on the patient’s response (pg 41).
Grade A, Level 2+
A
The appropriate short-term treatment goals are an initial 5%–10% weight loss over six months, and if this is not attainable, then a prevention of further weight gain may be recommended, which can improve mechanical symptoms and metabolic parameters. Long-term goals should continue in the same vein as the short-term goals, and the patient should be encouraged to lose more weight if possible (e.g. 10%–20% of initial body weight) (pg 42).
Grade A, Level 1++
A
Realistic weight loss should be safe and should preferably not exceed 0.5–1 kg a week (pg 42).
Grade A, Level 1++
Treatment: Diet
C
Nutritional counselling should aim to facilitate long-term adherence to reduced-calorie diets to achieve sustainable weight loss. Every 24 kcal/day reduction in energy intake will eventually lead to approximately a 1 kg loss in body weight with half of the weight loss occurring in about one year (pg 44).
Grade C, Level 2++
B
Physical activity should be recommended in addition to dietary changes as it can contribute to the maintenance of weight loss (pg 44).
Grade B, Level 1+
A
Diets that contribute to a calorie deficit of at least 500 kcal below estimated daily energy requirements are recommended to aid weight loss. The prescribed diets may be adjusted to meet the individual’s nutritional needs and to encourage prolonged compliance (pg 47).
Grade A, Level 1+
B
Because of the lack of evidence for long-term beneficial effect, caution should be exercised when recommending a high-protein, low-carbohydrate diet, especially to individuals who have osteoporosis, kidney disease or elevated low-density lipoprotein cholesterol (pg 47).
Grade B, Level 2++
B
Long-term compliance with a reduced-calorie diet and the adoption of positive lifestyle and behavioural changes should be encouraged to aid successful weight loss maintenance (pg 49).
Grade B, Level 1+
GPP
In order for weight loss or weight maintenance to be successful, food intake should ideally be distributed regularly throughout the day. Skipping of meals should be discouraged. Food portions at each meal should be adequate so as to prevent the need for frequent snacking between meals (pg 50).
GPP
A
Sugar-sweetened beverages should be avoided to prevent excess weight gain (pg 51).
Grade A, Level 1+
C
Maintain a diet that is higher in vegetables, legumes, fruit and whole grains, and lower in sugar and refined carbohydrates (pg 51).
Grade C, Level 2+
D
Adequate amounts of low energy density, lean, high-protein foods (e.g. chicken breast, fish, egg white, beans and tofu) should be included in weight loss diets to help control hunger (pg 51).
Grade D, Level 4
GPP
Dietary advice should consider foods that are locally available and match culinary preferences to facilitate long-term compliance (pg 51).
GPP
D
Caution should be exercised when making choices regarding processed foods as these can be energy dense and high in sugar (pg 51).
Grade D, Level 4
Treatment: Physical Activity
A
To maintain health and prevent diseases, overweight or obese adults should engage in ≥ 150 minutes of moderate-intensity physical activity per week (pg 53).
Grade A, Level 1+
D
Physicians should provide advice on physical activity regardless of BMI status. The exercise prescription should be tailored to individual patients, taking into consideration their body weight and comorbidities (pg 53).
Grade D, Level 3
Screening
GPP
Patients should be screened for common comorbidities, current physical and behavioural readiness before participating in physical activities (pg 54).
GPP
GPP
For inactive/unfit individuals, the recommended weekly volume of activity should be gradually increased over time as fitness improves (pg 54).
GPP
Aerobic Physical Activity
C
For weight loss, a negative energy balance (approximately 1,000 kcal per day) achieved through both dietary restriction and physical activity is encouraged (pg 55).
Grade C, Level 2+
Frequency
GPP
Physical activity should be established as a regular behaviour throughout the week (pg 55).
GPP
Intensity
D
Moderate-intensity aerobic activity should be recommended for the management of body weight (pg 55).
Grade D, Level 3
GPP
For unfit/inactive individuals, light-intensity physical activity may be considered first before progressing to moderate-intensity over time (pg 55).
GPP
Time
A
For weight loss, adults should engage in 150–420 minutes of moderate-intensity physical activity per week (pg 56).
Grade A, Level 1+
B
To maintain weight loss, adults should engage in 200–300 minutes of moderate-intensity physical activity per week (pg 56).
Grade B, Level 1+
B
Physical activity can be accumulated in short bouts of at least 10 minutes per session or one long bout of up to 60 minutes (pg 56).
Grade B, Level 2++
GPP
A total of 10–60 minutes of physical activity is recommended per day, with a gradual increase for unfit/inactive individuals over time (pg 56).
GPP
Type
GPP
Low-impact physical activities and cross training may be recommended (pg 56).
GPP
Strength or Resistance Activity
A
Adults should engage in strength activities on two non-consecutive days per week to provide additional health benefits (pg 57).
Grade A, Level 1+
Lifestyle and Sedentary Behaviour
A
Adults should be encouraged to spend less time engaging in sedentary behaviours. They should also break up prolonged periods of sitting (pg 57).
Grade B, Level 2+
GPP
Individuals should be encouraged to work towards taking 10,000 steps per day (pg 57).
GPP
Treatment: Behavioural Modifications and Related Therapy
D
Healthcare professionals working with weight loss patients should strive to have the patient adopt a more ‘internal’ style of motivation over time, such as ‘I want to’ lose weight for personal satisfaction and enjoyment of activities (pg 58).
Grade D, Level 2+
A
Weight loss programmes should incorporate cognitive behavioural interventions for achieving weight loss and weight maintenance of up to 10% between 1–5 years of follow-up (pg 60).
Grade A, Level 1+
B
Interventions need to combine behavioural strategies, such as self-monitoring and goal-setting, with dietary modification and increased physical activity (pg 60).
Grade B, Level 2+
A
After initial weight loss treatment, it is recommended that participants continue at least 6–12 months of a weight maintenance programme that combines dietary modification and physical activity (pg 62).
Grade A, Level 1+
Treatment: Information and Communication Technology (ICT) and Tools for Weight Loss
B
Clinicians who implement or recommend ICT interventions to their overweight and obese patients should ensure that such interventions include established treatment components such as tailoring, goal setting, self-monitoring, social support and targeted feedback (pg 64).
Grade B, Level 2+
Treatment: Medical Treatment of Obesity and Related Comorbidities
A
Lifestyle modification should be the main treatment strategy for weight management. Pharmacotherapy, if used, should be adjunctive to lifestyle modification and be combined with diet, physical activity and behaviour modification (pg 65).
Grade A, Level 1+
C
Drug therapy may be considered when BMI is ≥ 30 kg/m2, or when BMI is 27.5–29.9 kg/m2 in Asians with comorbidities or complications of obesity such as hypertension, Type 2 diabetes mellitus (pg 65).
Grade C, Level 2+
A
Phentermine and mazindol may be used for weight management for the short-term (6–12 months). Liraglutide may be used for weight management up to two years. Orlistat may be used as an anti-obesity drug for long-term therapy (up to four years) (pg 70).
Grade A, Level 1+
B
Acupuncture by trained/qualified professionals may be considered as short-term, adjunctive anti-obesity therapeutic option on a case-by-case basis (pg 70).
Grade B, Level 2++
Treatment: Surgical and Related Options
C
Bariatric surgery should be part of a programme of care delivered by a multidisciplinary team including surgeons, dietitians, nurses, psychologist, physicians and physical therapists. It should only be carried out in institutions where a full range of facilities and services are available 24 hours a day. These include (but are not limited to): specialist medical and nursing staff, access to operating rooms and intensive care units and radiology service with interventional capability (pg 71).
Grade C, Level 2+
A
Patients with BMI above 40 kg/m2, or above 35 kg/m2 with at least one obesity-related comorbidity, especially if difficult to control with lifestyle and pharmacological therapy, may be considered for bariatric surgery as a medical treatment (based on WHO BMI data, Asian BMI data is estimated to be about 2.5 kg/m2 lower) (pg 73).
Grade A, Level 1+
B
A bariatric procedure should only be offered after extensive work-up and discussions with the relevant stakeholders (pg 74).
Grade B, Level 2++
A
Patients with Type 2 diabetes and other medical comorbidities should be followed up by appropriate physicians according to the usual protocols for management of the respective conditions (pg 75).
Grade A, Level 1++
C
Lifelong follow-up by a multi-disciplinary team is mandatory for patients who undergo bariatric surgery (pg 76).
Grade C, Level 2+
B
Regular laboratory tests should be made available to monitor nutritional deficiencies. Regular supplementation is mandatory following bariatric procedures with a malabsorptive component (pg 77).
Grade B, Level 2++
Fertility and Pregnancy
C
Female patients should avoid getting pregnant post-bariatric surgery until weight loss has been stabilised. Appropriate contraceptive advice should be given (pg 77).
Grade C, Level 2+
C
Close liaison between the obstetrician and the bariatric team is highly desirable. For pregnant women who have undergone bariatric surgery, nutritional supplements over and above the usual requirements in a normal pregnancy are recommended (pg 77).
Grade C, Level 2+
Older Population
C
Among the older population, each case of bariatric surgery should be considered on its own merit, taking into account the special circumstances affecting the older age group (pg 78).
Grade C, Level 2+
Adolescents
B
Bariatric surgery should be considered only for obese paediatric patients who fulfil the following criteria (pg 79):
-
The adolescent has attained Tanner 4 or 5 pubertal development, and final or near-final adult height.
-
The adolescent has BMI greater than 50 kg/m2 or has BMI above 40 kg/m2 and significant severe comorbidities.
-
Severe obesity and comorbidities persist despite a formal programme of lifestyle modification, with or without a trial of pharmacotherapy.
-
Psychological evaluation confirms the stability and competence of the family unit.
-
There is access to an experienced surgeon in a medical centre employing a team capable of long-term follow-up of metabolic and psychosocial needs of the patient and the family. The institution must also be either participating in a study of the outcome of bariatric surgery or sharing data.
-
The adolescent demonstrates the ability to adhere to the principles of healthy dietary and activity habits.
Grade B, Level 2++
B
Adolescents undergoing bariatric surgery must be able to provide informed consent and understand the nature of the operation, the risks involved, and the need for long-term follow-up (pg 80).
Grade B, Level 2++
Special Focus: Children and Adolescents
GPP
During the transition to young adulthood, there may be discrepancy in weight status due to difference in the two classification systems. For the older adolescents (e.g. > 16 years old), obesity may be defined as a BMI-for-age equal to or greater than 97th percentile, or BMI equal to or greater than 30 kg/m2,
GPP
GPP
The majority of overweight and obese children may be managed in primary care. Referral to tertiary general paediatric, paediatric endocrine or medical genetic clinics should be guided by the degree of obesity, presence or likelihood of comorbidities (e.g. family history), or where pathological cause of obesity is suspected (pg 84).
GPP
GPP
In children, investigations for comorbidities should not be regarded as routine, but may be ordered as indicated clinically. Screening may include glucose levels, lipid profile, liver function test or other investigations if clinically indicated (pg 87).
GPP
C
Obese children and adolescents (BMI ≥ 97th percentile) should be evaluated for obesity-related comorbidities or complications. Overweight children (BMI ≥ 90–97th percentile) should be screened for comorbidities, especially if risk factors are present (pg 87).
Grade C, Level 2+
D
Screening for Type 2 diabetes mellitus may be performed for Asian overweight and obese children who are in puberty or ≥ 10 years old, and have any one of these risk factors: family history of Type 2 diabetes in first- or second-degree relatives, maternal gestational diabetes, and features of insulin resistance (acanthosis nigricans, hypertension, dyslipidaemia, non-alcoholic fatty liver disease, polycystic ovarian syndrome). Repeat screening with fasting glucose or oral glucose tolerance test can be offered every two years if excessive adiposity persists (pg 87).
Grade D, Level 4
GPP
The vast majority (> 95%) will have common or primary obesity. Pathological causes or secondary obesity (inclusive of monogenic causes) are uncommon but should be carefully considered. If there are no significant abnormalities in the history and examination indicative of pathological causes of obesity, investigations for these pathologies are generally not necessary. Testing may be limited to thyroid function. If there are clinical suspicions of pathological causes, these patients should be referred to tertiary centres for proper investigations and interpretation of the results (pg 87).
GPP
D
Weight management in children and adolescents should emphasise behavioural modifications that influence weight status, e.g. healthy eating habits and regular physical activity, rather than focus on actual weight loss. Weight maintenance or a slower weight gain to allow a gradual decline in BMI is an acceptable approach for pre-pubertal children with obesity. Weight loss should be limited to post-pubertal adolescents who are severely overweight and are supervised by paediatric specialists (pg 89).
Grade D, Level 4
D
Referral to a paediatric specialist or structured weight management programme for children and adolescents should be considered for the following cases: children with a suspected secondary cause of obesity, severely overweight children and adolescents with comorbidities that require weight loss (pg 89).
Grade D, Level 4
A
Obese children and adolescents should enrol in multi-component lifestyle interventions, which consist of nutrition, physical activity and behavioural modifications, which can result in a modest, but significant reduction in obesity and cardiovascular risk, compared to standard care, self-help or no treatment (pg 90).
Grade A, Level 1+
A
Parental involvement can enhance the effectiveness of lifestyle interventions, particularly in pre-adolescent children, by changing and adapting parenting styles, parenting skills and child management strategies during the intervention, such as role modelling and active parental participation (pg 90).
Grade A, Level 1+
C
Dietary interventions for obese children and adolescents should comprise the following strategies: reducing intake of calorie-dense, nutrient-poor foods (sweetened beverages, fruit drinks and juices, fast foods, calorie-dense snacks), portion control, reducing saturated fat intake (for children > 2 years), encouraging intake of fibre/whole grains, fruits and vegetables, as well as encouraging healthy eating behaviours such as eating regular meals (especially breakfast), avoiding having meals in front of the television (TV)/computer and avoiding frequent food nibbling or ‘grazing’ during the day, especially after school. Diets should also be adequate in micronutrient intake to promote optimal linear growth (pg 91).
Grade C, Level 2++
D
The use of restrictive diets is not appropriate for children and adolescents except when combined with specialist supervision and intensive follow-up (pg 92).
Grade D, Level 4
A
Physical activity should be routinely included within a multi-component lifestyle intervention for reducing overweight and obesity in school-age children and adolescents (pg 92).
Grade A, Level 1+
D
Obese children and adolescents should be encouraged first to meet the National Physical Activity Guidelines for children and youths by increasing their daily physical activity level progressively. Additional physical activity on top of the recommended guidelines may be needed for general health benefits for this group of youths (pg 93).
Grade D, Level 4
D
Sedentary activities (TV viewing, playing video games etc.) should be limited to not more than two hours a day, or equivalent to 14 hours per week for all children (pg 93).
Grade D, Level 4
A
Pharmacotherapy for weight loss should only be considered as an adjunct to lifestyle interventions in obese adolescents with severe comorbidities or when lifestyle interventions have failed. It should only be administered by experienced clinicians. The decision should be carefully weighed against the potential for adverse effects, the lack of evidence for persistent weight loss after active treatment and the long-term safety in adolescents (pg 94).
Grade A, Level 1+
Special Focus: Pregnancy
Screening
B
Women of childbearing age, especially overweight and obese women, should receive information and advice from healthcare providers about the benefits of weight loss before pregnancy and the risks of being overweight or obese. An ideal preconception weight will optimise pregnancy outcome for both mother and baby (pg 95).
Grade B, Level 2+
B
Height and pre-pregnancy weight should be recorded in the health record for all women at the initial antenatal visit. Pre-pregnancy BMI can be calculated and classified using the WHO BMI cut-off points (Table II) (pg 95).
Grade B, Level 2+
D
Prior to attempting to conceive, women of childbearing age should stop taking medication for weight loss (pg 95).
Grade D, Level 4
Pregnancy weight management
B
The range of desirable total weight gain and the rate of gain should be discussed with the woman early in her pregnancy. A plan to achieve these goals should be documented (pg 96).
Grade B, Level 2+
B
Nutritional advice should be routinely provided to all pregnant women (refer to Chapter 7 on Treatment: Diet for an explanation of a healthy diet). General advice should include (pg 96):
Eating a healthy, balanced diet as per ‘Pregnancy and Diet, Health Promotion Board, Singapore’ including foods rich in calcium, folate and iron.
Not restricting dietary intake below the recommended food group requirements for pregnancy.
Avoiding certain foods and drinks (such as raw foods, coffee/tea and alcohol) which can be harmful to the pregnancy.
Taking folic acid supplements.
Adhering to recommended weight gain ranges (Table II).
Grade B, Level 2+
B
In the absence of obstetric or medical complications, all pregnant women should accumulate 150 minutes per week of moderate-intensity exercise (e.g. accumulate 30 minutes per day, best to spread this activity throughout the week). Qualified supervision may be offered to assist with assessment and individual exercise prescription (pg 97).
Grade B, Level 2+
Complications of obesity in pregnancy
B
Consider booking an early visit to plan pregnancy care. A pregnancy care plan with increased clinical surveillance is recommended for obese, pregnant women in the antenatal, intrapartum and postnatal periods. Consider a cardiac risk assessment for women with pre-existing medical conditions, especially those with Class III obesity and who have other risk factors such as smoking or Type 2 diabetes (pg 97).
Grade B, Level 2++
B
All overweight or obese women should be screened for diabetes with a 75 g Oral Glucose Tolerance Test at 24–28 weeks gestation. For women with Class II and III obesity (pre-pregnancy BMI ≥ 35.0 kg/m2), consider an early oral glucose tolerance test (below 14 weeks gestation if possible) to assess for pre-existing diabetes. If the initial oral glucose tolerance test is negative, consider repeating at 28 weeks if the risk of diabetes is significantly high or if the patient exhibits clinical symptoms of diabetes (pg 97).
Grade B, Level 2++
B
For women with Class III obesity (pre-pregnancy BMI ≥ 40 kg/m2), co-manage with a physician who will establish baseline renal (presence of proteinuria, serum creatinine and urea) and liver function to assist in distinguishing chronic renal dysfunction secondary to maternal chronic hypertension and/or diabetes from pregnancy-associated hypertensive/diabetic disorders (pg 98).
Grade B, Level 2+
B
The risk of venous thromboembolism for every obese woman should be evaluated in the presence of additional clinical risk factors. Thromboprophylaxis for antenatal and postnatal, if indicated, should be individualised (pg 98).
Grade B, Level 2++
B
Consider antenatal anaesthetic consultation to review analgesic options, especially for women with pre-pregnancy BMI > 35 kg/m2, and consider facility capabilities including equipment and extra staffing when performing Caesarean section and other surgeries (pg 99).
Grade B, Level 2+
Post-natal management
D
Discuss healthy eating, physical activity and breastfeeding as strategies for returning to pre-pregnancy weight with all postpartum women. Women in a healthy pre-pregnancy BMI range should be advised of the importance of maintaining a healthy pre-pregnancy BMI between pregnancies. Overweight and obese women should be encouraged to lose weight before considering a future pregnancy (pg 99).
Grade D, Level 4
D
Offer obese women additional support for breastfeeding. Consider referral to a lactation consultant, increasing supervision during breastfeeding and providing early postpartum breastfeeding support (pg 99).
Grade D, Level 4


