Abstract
INTRODUCTION
Obstructive sleep apnoea (OSA) is the most common sleep-related breathing disorder associated with multisystemic organ involvement. The STOP-BANG questionnaire is a concise, validated questionnaire that is used to screen for OSA. This study aimed to establish the use of the STOP-BANG questionnaire for perioperative patient risk stratification.
METHODS
In this retrospective cohort study, we extracted the demographic, medical and perioperative outcome data of all patients who underwent elective surgery, excluding ophthalmic surgeries, from January to December 2011. Multivariate regression analysis was used to predict independent risk factors for intraoperative and early postoperative adverse events.
RESULTS
Of the 5,432 patients analysed, 7.4% had unexpected intraoperative and early postoperative adverse events. We found that the risk of unexpected intraoperative and early postoperative adverse events was greater in patients with STOP-BANG scores ≥ 3 compared to those with a STOP-BANG score of 0 (score 3: odds ratio [OR] 3.6, 95% confidence interval [CI] 2.1–6.3, p < 0.001; score 4: OR 3.4, 95% CI 1.8–6.5, p < 0.001; score 5: OR 6.4, 95% CI 2.7–15.0, p < 0.001; score ≥ 6: OR 5.6, 95% CI 2.1–15.4, p < 0.001). Patients with STOP-BANG scores ≥ 5 had a fivefold increased risk of unexpected intraoperative and early postoperative adverse events, while patients with STOP-BANG scores ≥ 3 had a ‘one in four’ chance of having an adverse event. Other independent predictors included older age (p < 0.001), American Society of Anesthesiologists class ≥ 2 (p < 0.003) and uncontrolled hypertension (p = 0.028).
CONCLUSION
STOP-BANG score may be used as a preoperative risk stratification tool to predict the risk of intraoperative and early postoperative adverse events.
INTRODUCTION
Obstructive sleep apnoea (OSA) is the most common sleep-related breathing disorder. It is a clinical syndrome that is characterised by recurrent, episodic cessation of breathing that lasts for ten seconds or more during sleep. The prevalence of OSA is estimated to be 41.5% among patients presenting for elective surgery.(1) This number increases up to 80% in high-risk patients such as those who are scheduled to receive bariatric surgery.(2)
OSA remains undiagnosed in about four out of five patients at the time of surgery;(2) this is likely due to logistical difficulties and cost considerations in diagnosing patients via a formal polysomnography study. As OSA has been associated with increased postoperative cardiac complications, respiratory failure, emergent reintubations and postoperative intensive care unit admissions,(3) patients with undiagnosed OSA may unknowingly be placed at an increased risk for perioperative complications, due to the untreated nature of their disease. Furthermore, OSA poses an economic burden, as it increases the length of hospital stay and healthcare costs.(4) As such, various clinical prediction scores have been employed to screen for OSA preoperatively.
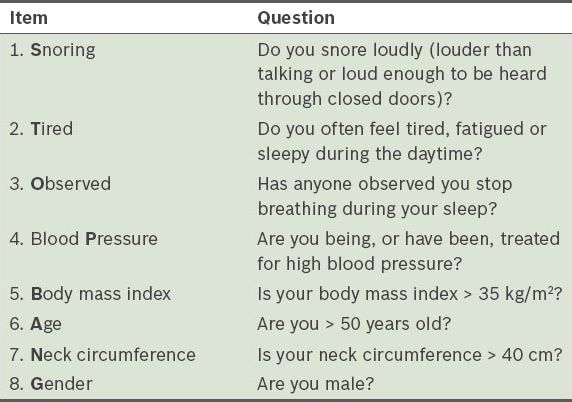
The STOP-BANG questionnaire (
Table I
STOP-BANG questionnaire for screening of obstructive sleep apnoea.
Recent studies have demonstrated the utility of the STOP-BANG questionnaire in stratifying patients undergoing elective surgery.(1,7) Vasu et al showed that patients categorised as having a high risk of OSA using the STOP-BANG questionnaire (i.e. had scores ≥ 3) were associated with a higher rate of postoperative complications as compared to patients with STOP-BANG scores < 3 (19.6% vs. 1.3%, p < 0.001).(1) Chia et al showed that higher preoperative STOP-BANG scores were significantly associated with postoperative critical care admission.(7)
In the present study, we hypothesised that elective surgical patients with higher preoperative STOP-BANG scores are associated with an increased likelihood of intraoperative and early postoperative adverse outcomes. We explored the novel use of STOP-BANG scores for preoperative risk stratification of adverse events for elective surgical patients.
METHODS
This retrospective cohort study was approved by the Domain Specific Review Board and funded by the Alexandra Health Enabling Grant 2011. Preoperative assessment of the patients who underwent elective surgery was performed in the preoperative anaesthesia clinic of Khoo Teck Puat Hospital, Alexandra Health Services, Singapore, a tertiary teaching hospital. The preoperative assessment was conducted over a one-year period, from 1 January 2011 to 31 December 2011. Patients who underwent elective ophthalmic surgeries or emergency surgeries were excluded from this study.
Information obtained from the preoperative assessment of elective surgical patients was recorded and digitised into the OTSystem (Medisys Innovation Pte Ltd, Singapore), the hospital’s proprietary, customised perioperative electronic medical record system. Mandatory information collected in the perioperative records included demographic data (i.e. age, gender and ethnicity), clinical data (i.e. American Society of Anesthesiologists [ASA] physical status, comorbidities, body mass index [BMI] and STOP-BANG score), surgical data (i.e. nature of surgery and type of anaesthesia used) and unexpected perioperative adverse events as reported by the attending anaesthetist. The perioperative adverse events recorded (detailed in
Data was analysed using the IBM Statistical Package for the Social Sciences software for Windows version 20.0 (IBM Corp, Armonk, NY, USA). Continuous variables were reported as mean ± standard deviation, while categorical variables were reported as number (percentage). Multiple logistic regression analysis was used to assess the effect of individual risk factors on unexpected perioperative adverse events, after adjustment for other factors. Odds ratios (ORs) and their corresponding 95% confidence intervals (CIs) were reported. A p-value < 0.05 was considered statistically significant.
RESULTS
A total of 9,178 patients were administered the STOP-BANG questionnaire during their review in the preoperative anaesthesia clinic. Among these patients, 3,746 patients were excluded from the present study as they underwent either ophthalmic surgery or emergency surgery. Thus, a total of 5,432 patients were included in the study.
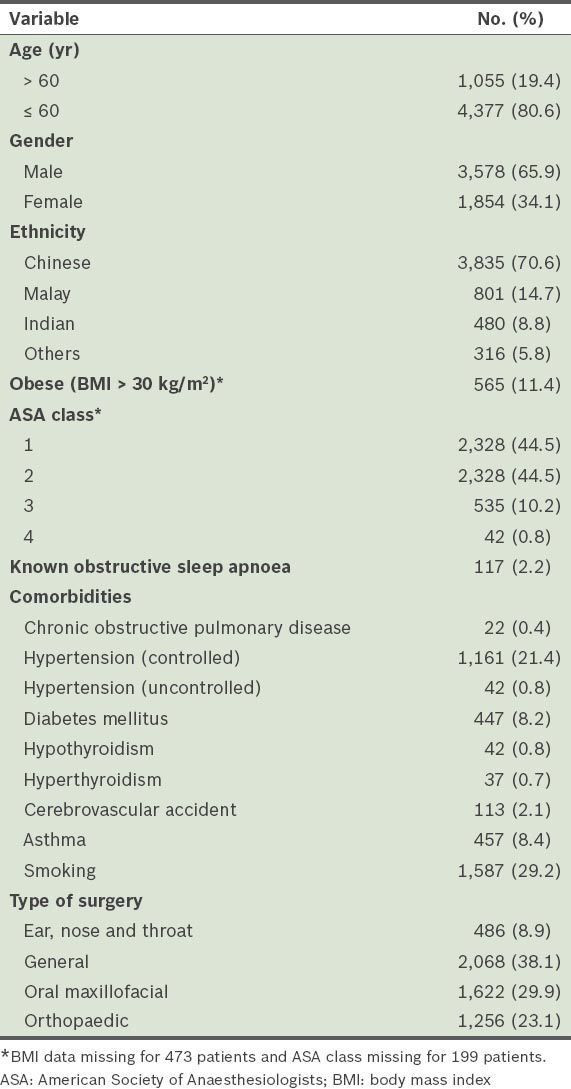
The baseline demographic data of the 5,432 patients is shown in
Table II
Demographic data of the patients (n = 5,432).
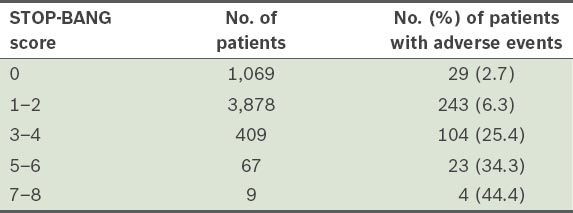
Of the 5,432 patients, 485 (8.9%) patients had STOP-BANG scores of 3–8, and 76 (1.4%) patients had STOP-BANG scores of 5–8; 7.4% had unexpected intraoperative and early postoperative adverse events. Patients with higher STOP-BANG scores were found to have a higher risk of unexpected intraoperative and early postoperative adverse events (
Table III
Risk estimates for unexpected perioperative adverse events.
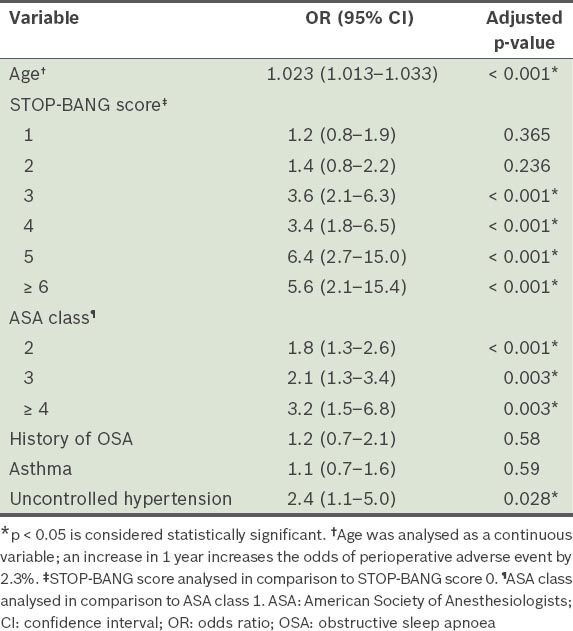
Table IV
Number of patients with perioperative adverse events according to stratified STOP-BANG scores.
DISCUSSION
OSA is a chronic multisystem disorder that has been associated with cardiovascular diseases (e.g. ischaemic heart disease, heart failure, arrhythmias and hypertension), cerebrovascular diseases (stroke and transient ischaemic attack) and endocrine disorders (e.g. metabolic syndrome and obesity).(8) These comorbidities, together with the pathophysiological effects of sedatives and/or analgesic and anaesthetic agents, may aggravate the symptoms of OSA by reducing pharyngeal tone, ventilatory reflexes and arousal responses, consequently leading to airway obstruction, hypoxia, hypercarbia, haemodynamic aberrations and other adverse events during the perioperative period.(9) A meta-analysis by Kaw et al showed that OSA increased the odds of postoperative complications such as myocardial infarction, cardiac arrest, arrhythmias, respiratory failure, desaturation, intensive care unit transfers and reintubations.(3)
Higher STOP-BANG scores were shown to be correlated to higher rates of postoperative respiratory and cardiovascular complications in a study conducted by Vasu et al.(1) In the present study, we investigated the relationship between the rate of unexpected intraoperative and early postoperative complications (not limited to respiratory and cardiovascular complications) and STOP-BANG scores. We found that STOP-BANG scores were useful for stratifying patients who are at risk of unexpected intraoperative and early postoperative adverse events. Patients with higher STOP-BANG scores (i.e. ≥ 3) were found to have higher risks of perioperative adverse events. The ORs of unexpected adverse events for patients with STOP-BANG scores of 3 and 4 (vs. 0) were 3.6 and 3.4, respectively. STOP-BANG scores of 5 and ≥ 6 were associated with at least a fivefold increased rate of perioperative adverse events (OR 6.4, 95% CI 2.7–15.0, p < 0.001 and OR 5.6, 95% CI 2.1–15.4, p < 0.001, respectively). As the number of patients with STOP-BANG scores ≥ 6 was small, this could have contributed to the lower OR observed for these patients as compared to that of the patients with a STOP-BANG score of 5.
In the present study, stratification of the STOP-BANG scores also showed that increasing scores were associated with an increasing risk of unexpected intraoperative and early postoperative adverse events. This means that the STOP-BANG score may be ideal for the stratification of intraoperative and early postoperative risk. In our study, patients with STOP-BANG scores ≥ 3 were shown to have at least a ‘one in four’ chance of an adverse event in the intraoperative and early postoperative period. Approximately 44.4% of the patients with STOP-BANG scores of 7 and 8 were at risk of an adverse event. This finding is in keeping with the results of a smaller sample size study by Vasu et al.(1) In that study, 135 mixed surgical patients who had STOP-BANG scores ≥ 3 and ASA class ≥ 3, were found to have a higher risk of postoperative pulmonary or cardiac complications, and an increased length of hospital stay.(1) A recent study by Chia et al also showed that a STOP-BANG score ≥ 4 was significantly associated with an increased risk of critical care admission.(7)
Interestingly, we did not find a correlation between patients known to have OSA and perioperative adverse events in our study. However, the number of patients with known OSA in this study was small and this may have led to the inability to detect a statistically significant correlation. As pointed out by Memtsoudis et al, about four out of five patients presenting for surgery have undetected OSA.(2) Other than that, patients with known or diagnosed OSA may be on treatment and continuous positive airway pressure therapy, thus reducing their perioperative risks.
Previous studies have described other risk factors associated with perioperative complications, including advanced age, ASA class ≥ 3, congestive heart failure, obesity and hypoalbuminaemia.(1,10) Some of these independent predictors of unexpected perioperative adverse events were also detected in the present study, namely older age (p < 0.001), ASA class ≥ 2 (p < 0.003) and uncontrolled hypertension (p = 0.028).
OSA may be incorrectly diagnosed if the diagnosis is based solely on the STOP-BANG questionnaire; this is because the STOP-BANG questionnaire has low specificity.(11) In the present study, the diagnosis of OSA was not confirmed with polysomnography for the patients who had high STOP-BANG scores, as this was not part of the study protocol. In view of the evidence that suggests a correlation between OSA and increased perioperative adverse events, it may be prudent for patients with STOP-BANG scores ≥ 5 to undergo polysomnography prior to elective surgery. Risk mitigation strategies would be important in these high-risk patient groups.
The present study was not without limitations. It was limited by the attending anaesthetist’s reporting of information (e.g. comorbidities, STOP-BANG score and perioperative adverse events) on the OTSystem. Also, as the study was done retrospectively, we were not able to account for missing data or include other data that may be of importance (e.g. the timing of the perioperative adverse events and/or specific data regarding cardiovascular or respiratory adverse events).
In conclusion, the present study demonstrated that akin to the ASA physical status classification, the STOP-BANG score may be used as a novel preoperative risk-stratification tool. A STOP-BANG score ≥ 5 was found to be associated with a fivefold increased risk of unexpected intraoperative and early postoperative events. One in four patients with STOP-BANG scores ≥ 3 was found to be at risk of an adverse event. Therefore, attending anaesthetists should be vigilant in the management of these at-risk patients.
SMJ-56-216-appendix.pdf
ACKNOWLEDGEMENTS
We thank A/Prof Ng Tze Pin from Yong Loo Lin School of Medicine, National University of Singapore, Singapore, for his assistance with the statistical analyses.


