Abstract
INTRODUCTION
This study aimed to assess the effectiveness of the emergency department observation unit (EDOU) for patients with acute pyelonephritis in a Singapore tertiary academic medical centre.
METHODS
We reviewed the clinical records of consecutive patients who presented with pyelonephritis between 1 July 2012 and 31 October 2014 to collect information on demographics, symptoms, signs, laboratory and radiological results, treatment, and clinical outcomes.
RESULTS
Of 459 emergency department (ED) patients who were identified as having pyelonephritis, 164 (35.7%) were managed in the EDOU. Successful management in the EDOU was achieved in 100 (61.0%) patients. Escherichia coli was the predominant (64.6%) micro-organism in urine cultures and was positive in 106 patients. Patients diagnosed with acute pyelonephritis who were successfully managed in the EDOU had a lower incidence of nausea (32.0% vs. 60.9%, p < 0.001) and vomiting (15.0% vs. 50.0%, p < 0.001) compared to those who were not successful.
CONCLUSION
EDOU is useful for both observation and treatment of patients with acute pyelonephritis. Urine cultures are sufficient for the identification of the culprit micro-organism. Patients who present with prominent symptoms of vomiting should have routine administration of antiemetics, while consideration for second-line antiemetics is recommended for those with persistent symptoms.
INTRODUCTION
Acute pyelonephritis, an illness caused by bacterial infection of the kidney, is suggested by the presence of flank pain, nausea or vomiting, fever, and costovertebral angle tenderness with or without the typical symptoms of cystitis, and is confirmed by the finding of bacteriuria in the setting of these symptoms.(1) It occurs in more than 250,000 adults in the United States yearly, costing an estimated USD 2 billion a year.(2,3)
The recommendations for treatment vary from inpatient management to outpatient therapy for different groups of patients.(4-8) Older studies have shown that observational care is feasible in managing acute pyelonephritis and reducing hospital admissions.(9,10) Given the known complications of septic shock, multi-organ failure and death in severe cases, patient care can be optimised by appropriate unit selection, which can reduce morbidity and mortality and allow limited hospital resources to be used more judiciously.
The primary aim of this study was to assess the effectiveness of the emergency department observation unit (EDOU) for patients with acute pyelonephritis, defined as successful discharge from the EDOU without re-admission within seven days. The secondary aim was to identify the risk factors and predictors for requiring subsequent inpatient management in patients with pyelonephritis admitted to the EDOU, in order to improve the effectiveness of the EDOU.
METHODS
A retrospective chart review was conducted of consecutive adult patients presenting to the emergency department (ED) of National University Hospital, Singapore, with a primary or secondary diagnosis of pyelonephritis between 1 July 2012 and 31 October 2014. Ethical approval was obtained from the National Healthcare Group Domain Specific Review Board (2014/00791), which granted waiver of informed consent.
The EDOU at our institution is a 16-bed facility that is under the oversight of an ED physician for 24 hours daily. A variety of EDOU protocols are available on the department intranet, one of which is the acute pyelonephritis protocol (Appendix). The protocol was created in tandem with infectious disease physicians based on expert opinion. Patients with suspected acute pyelonephritis can be admitted to the EDOU and managed for up to 24 hours. Within 24 hours, patients may be discharged home to continue outpatient treatment if their vital signs are stable and they are able to take well orally. Patients are admitted to an inpatient unit if they turn unwell with unstable vital signs, deteriorating renal function, increasing lactate, white blood cell count > 20 × 109/L, persistent vomiting or inadequate oral intake, increasing loin pain, pyuria, or ballotable kidneys.
Cases were identified using EDOU and inpatient unit primary and secondary discharge diagnosis codes according to the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM – N10, N11*, N12, N13* and A41.9). A total of 705 ED visits were identified, and all visit records were located and reviewed.
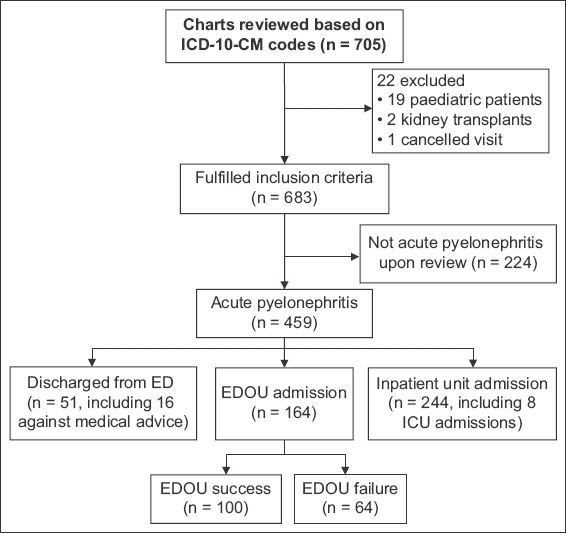
Identified patients were screened for enrolment by a single reviewer (Khoo KSM) who reviewed electronic and physical case records, with 20% of cases verified independently by a second reviewer (Kuan WS) for accuracy. The second reviewer provided independent input for borderline cases with ambiguous documentation in the medical records or inconclusive comments in reports of imaging modalities. The reviewers were not blinded to the purpose of the study. Patients with at least two out of the following three inclusion criteria(11) were recruited into the study: (a) flank pain or costovertebral angle tenderness; (b) urinary symptoms or bacteriuria/pyuria; and (c) fever. Subjects were also included if they were labelled as having pyelonephritis based on imaging (ultrasonography of the kidneys or computed tomography of the kidneys, ureters and bladder) or by the managing team. Patients who were below 18 years of age, had transplanted kidneys or cancelled their visits before being seen by a physician were excluded. Each ED visit was treated as a separate episode. A total of 459 ED visits satisfied the aforementioned criteria (
Fig. 1
Flowchart shows the enrolment process. ED: emergency department; EDOU: emergency department observation unit; ICD-10-CM: International Classification of Diseases, 10th Revision, Clinical Modification; ICU: intensive care unit
All data was recorded using a standardised abstraction form on Microsoft Excel 2013 (Microsoft Corp, Redmond, WA, USA). Data was collected using an electronic medical record system. Where electronic charts were unavailable, paper charts were retrieved and reviewed.
Data evaluated included demographic information, presenting symptoms, physical findings, laboratory results, imaging, therapy and disposition.
EDOU success was defined as the discharge of a patient who was treated in the EDOU without any repeat hospital admission in the following week. EDOU failure referred to cases in which patients required hospitalisation despite treatment in the EDOU, or returned and were hospitalised within one week.
Upon completion of electronic data collection, charts were reviewed for missing or duplicate data and verified. Data was exported to Stata 14 (StataCorp LP, College Station, TX, USA) for statistical analysis. Categorical variables were reported as frequency and percentage values. For continuous variables, mean ± standard deviation and median (interquartile range [IQR]) were reported for normal and skewed distributions, respectively. Differences in categorical variables between the EDOU success and failure groups were compared using chi-square test or Fisher’s exact test. Normally distributed continuous outcomes were compared using Student’s t-test, whereas highly-skewed continuous outcomes were compared using Mann-Whitney U test. Multivariate logistic regression analysis was performed to determine the characteristic differences between the two groups using odds ratios (ORs) and 95% confidence intervals (CIs). A stepwise approach was used while including only variables with p < 0.10 into the model.
RESULTS
The majority of the 459 patients were female (88.9%) and young, with a median age of 36 (IQR 28–50) years (
Table I
Baseline demographics, symptoms, signs and disposition of the patients (n = 459).
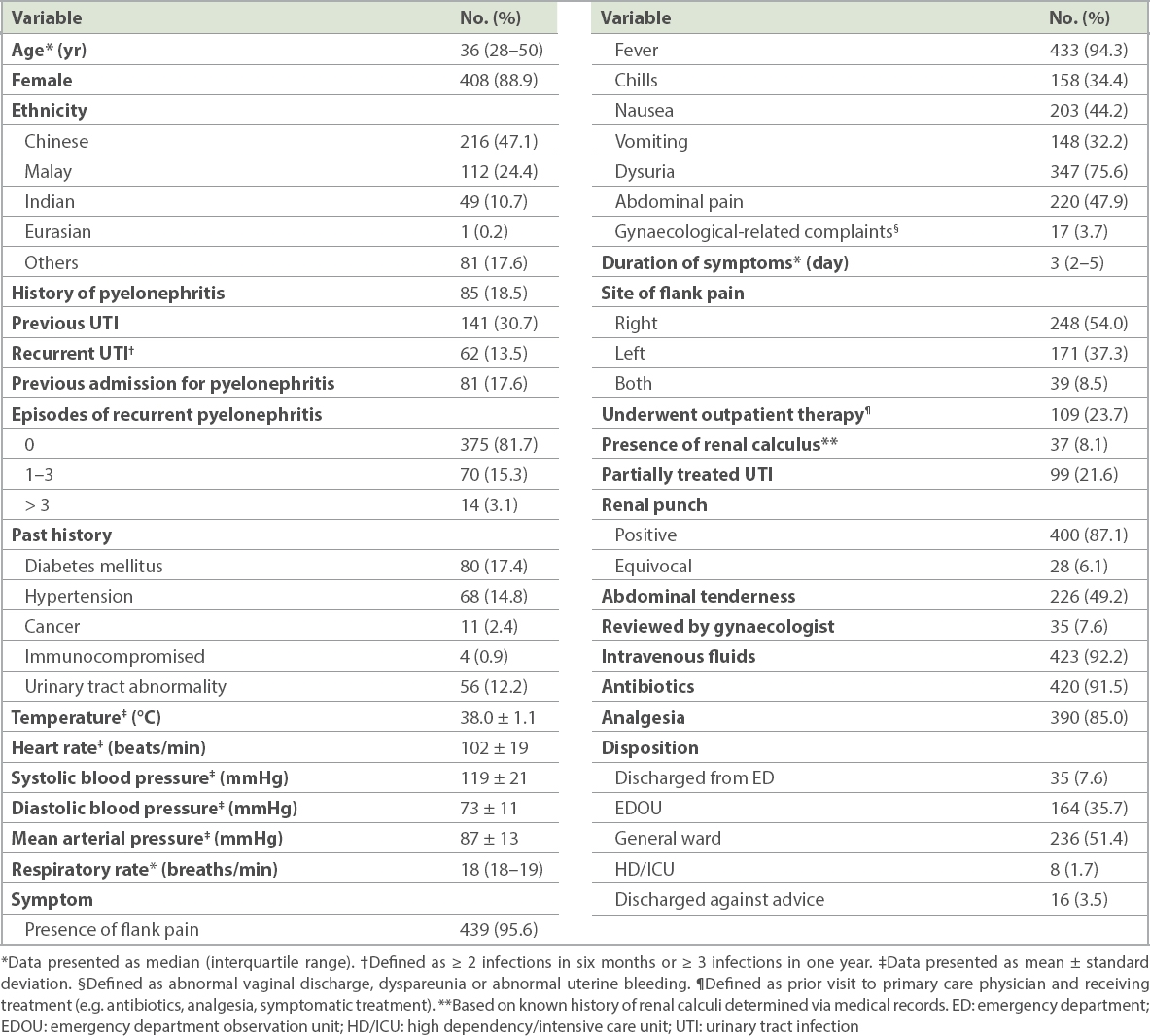
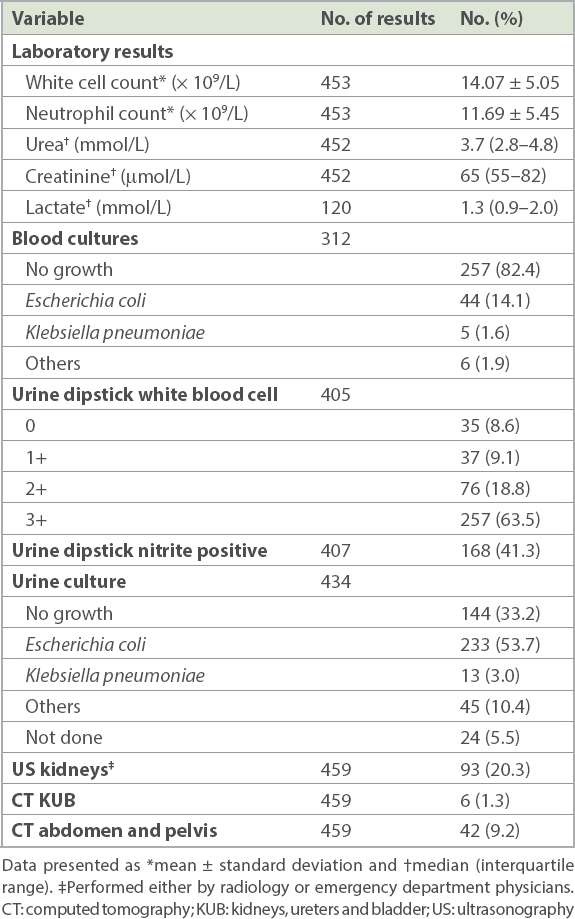
Table II
Laboratory and radiological investigations.
210 patients were admitted to the EDOU under the acute pyelonephritis protocol. 46 (21.9%) of these patients were found to have other diagnoses such as lower urinary tract infection (n = 25), renal colic (n = 5), musculoskeletal pain (n = 5), gastroenteritis (n = 3), non-specific abdominal pain (n = 3), appendicitis (n = 2), dengue (n = 2) and gastritis (n = 1). 9 (19.6%) of these 46 patients were admitted to the general ward, while the rest were discharged from the EDOU.
Of the 164 patients admitted to the EDOU with an adjudicated diagnosis of acute pyelonephritis, 100 (61.0%) were discharged, while 61 (37.2%) were admitted to the inpatient wards, of whom 3 (1.8%) required high dependency care (
Table III
Characteristics of the EDOU patients.
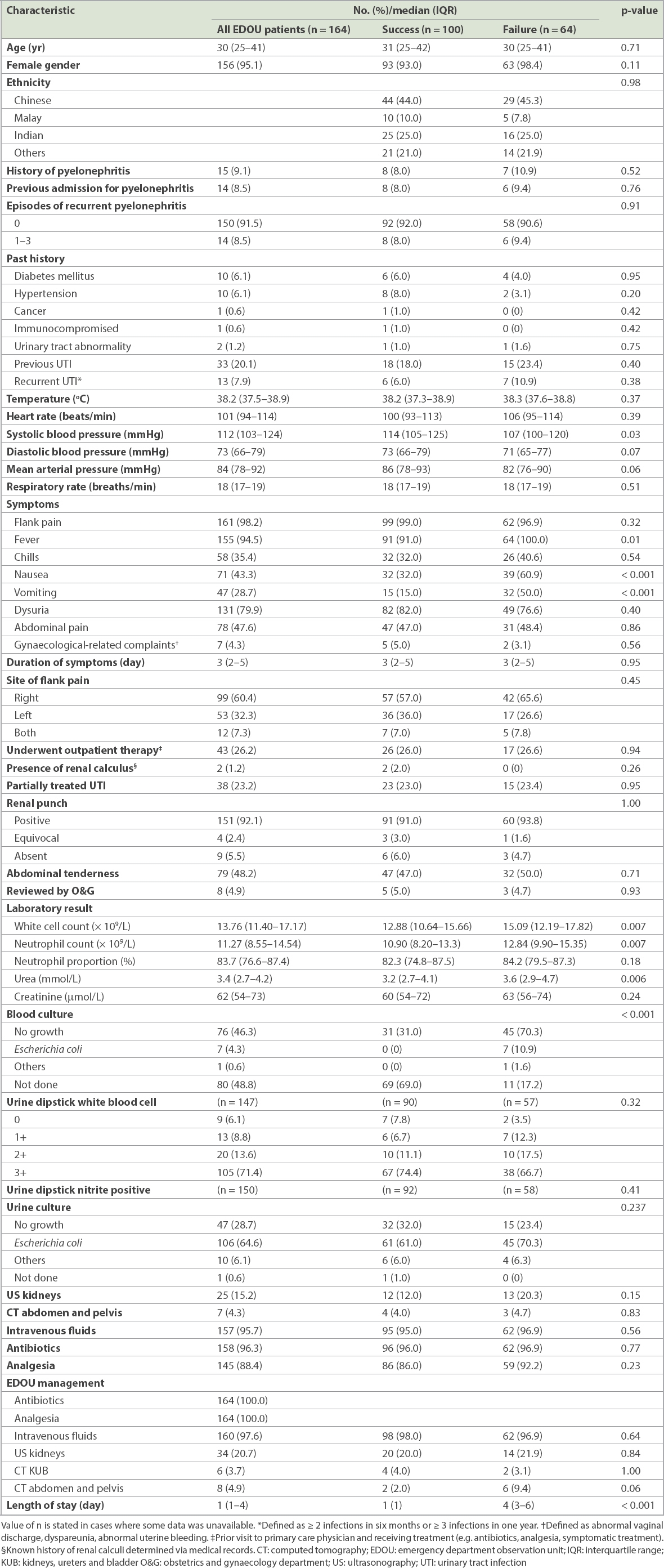
Lower systolic blood pressure at triage, fever, higher urea levels and a higher white blood cell count all had a statistically significant association with EDOU failure (
84 (51.2%) of the 164 patients admitted to the EDOU had blood cultures done, of which only eight were positive: seven for Escherichia coli and one for Bacillus species (which was deemed to be a contaminant). Among the 459 patients, the 144 (31.4%) patients who were finally classified as having pyelonephritis had a negative urine culture.
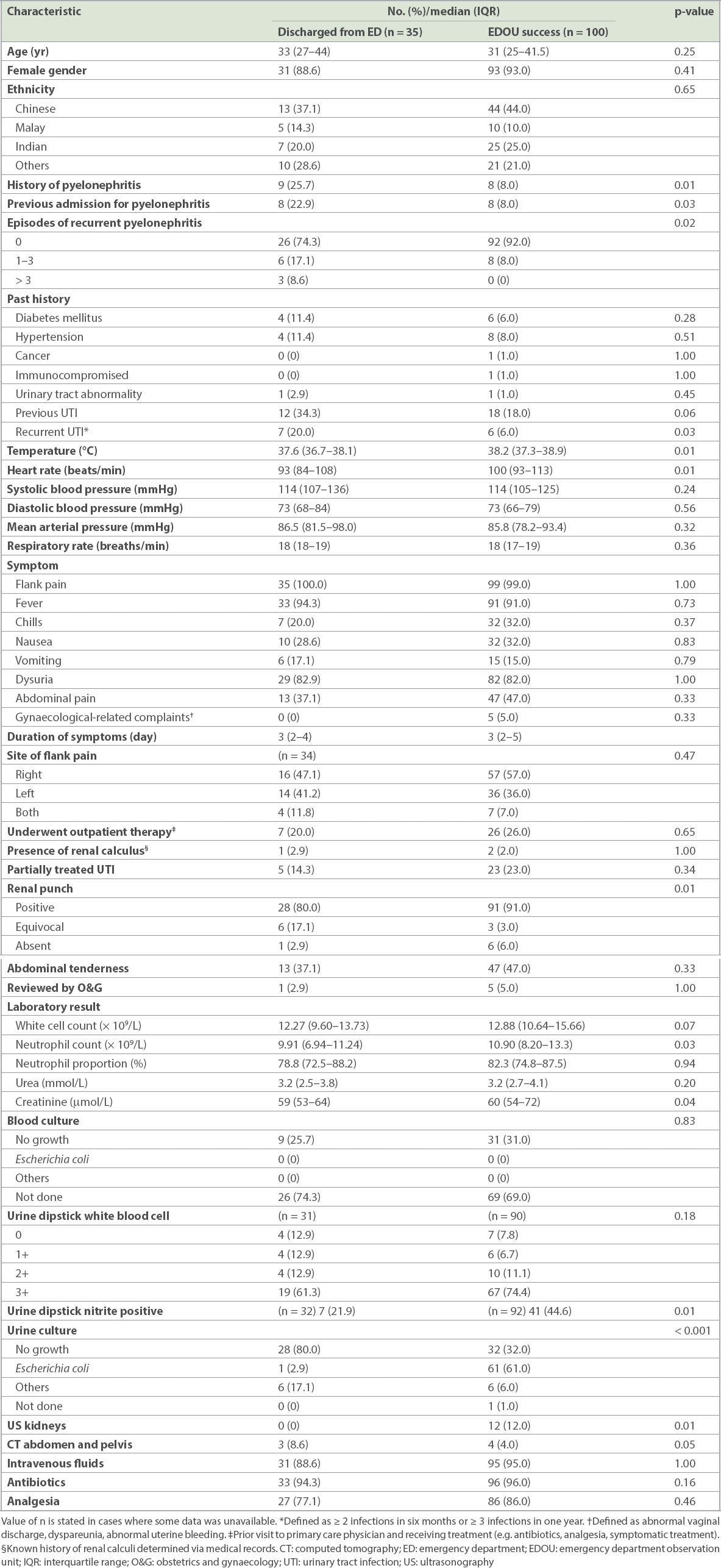
Patients who had EDOU success had a higher temperature, heart rate, neutrophil count and urine dipstick nitrite positive rate compared to those discharged directly from the ED, although the association was not clinically significant (
Table IV
Comparison of patients discharged from the ED and those in the EDOU success group.
DISCUSSION
In our study, the EDOU acute pyelonephritis protocol was shown to be useful for treatment and observation for evolving symptoms and signs. Over one-third of patients presenting to our ED with pyelonephritis were managed in the EDOU. To the best of our knowledge, there is little data in the literature regarding EDOU admission rates for pyelonephritis in other centres. Schrock and colleagues demonstrated an EDOU admission rate of 24%, but their EDOU was newly created when the data was collected, which possibly accounted for the lower rate.(12)
Unresolved fever was the most commonly cited reason for EDOU failure in the present study. Of note, unresolved fever is not listed as an admission criterion in our protocol and some patients were successfully discharged from the ED despite unresolved fever. The reason for admitting patients with unresolved fever was not always documented in the case records. Based on clinical experience, we postulate that unresolved fever is associated with an overall fatigued and dehydrated state, and such patients tend to have poor oral intake, which indirectly leads to EDOU failure. In the local population, patients have expectations that fever should lyse by the time they are discharged, and patients may not feel confident of managing their illness at home if they are still febrile when leaving the EDOU, leading to increased admissions. However, it is not always possible to predict which group of patients will end up getting admitted, as there are no clear predictors to indicate the pattern of fever.
The results of this study suggest that fewer patients in the EDOU success group tend to have nausea or vomiting. We note that the inability to retain feeds was not the top reason for EDOU failure in this study. The decision for admission is often influenced by a constellation of factors, as illustrated in this study, and we postulate that these factors may not have been adequately documented in the case records. As listed in the discharge criteria (Appendix), patients should be able to retain feeds before discharge, which may explain why fewer patients in the EDOU success group have nausea or vomiting. Hence, for patients with pronounced symptoms of vomiting on presentation to the ED, we strongly recommend routine administration of antiemetics to control symptoms, with consideration of second-line therapy if the symptoms of vomiting remain protracted. These measures may help to maximise EDOU effectiveness.
In our study, only a minority (11.1%) of patients were discharged from the ED, in contrast to results from overseas centres. Possible explanations include patient expectations and the perceived risk of failure of outpatient therapy with subsequent reattendance. The patient characteristics of those discharged directly from the ED were largely similar to those with EDOU success. This gives rise to the question of whether these patients could potentially have been discharged directly from the ED. However, it would be difficult to predict which of the patients fall into this category given the relatively high failure rate in the EDOU.
144 (31.4%) patients who were finally classified as having pyelonephritis had a negative urine culture. The percentage of patients with negative urine cultures in other studies ranged from 3.6% to 32.3% depending on the inclusion and exclusion criteria of each study.(7,11) The high percentage of negative urine cultures found could be due to 109 (23.7%) patients having received outpatient antibiotics before the ED visit, although the details of the type of antibiotics and duration of treatment were often unspecified. Another reason could be the commencement of empirical antibiotics in the ED after obtaining blood cultures, with a delay in obtaining urine cultures, particularly for patients who appeared ill. A previous study had shown that negative urine cultures can coexist with imaging-proven pyelonephritis.(13)
For patients with uncomplicated pyelonephritis, blood cultures are not routinely recommended, as the results do not alter clinical management and seldom vary from urine culture results.(12) From previous studies, the discordance between blood and urine cultures does not exceed 3%.(14,15) Uncomplicated pyelonephritis is defined as pyelonephritis occurring in young females without structural or functional urinary tract abnormalities and without relevant comorbidities, which fits the general characteristics of the vast majority of patients in this study.(16-18) Over half of the patients admitted to the EDOU had blood cultures done; only eight were positive, of which two had uncomplicated pyelonephritis. The results of the blood cultures did not alter the antibiotic regimen of all eight patients. Given the cost associated with negative blood cultures as well as the risk of false positives, it would be prudent to avoid collecting blood cultures if they are not clinically indicated.
From our centre’s data on the antibiotic resistance pattern of Enterobacteriaceae for community-acquired urinary tract infections in 2011, 29.8% of patients were resistant to ciprofloxacin and 33% were resistant to cotrimoxazole. Our laboratory did not report on the presence of extended-spectrum beta-lactamase producers but only on carbapenem resistance. As a result of emerging resistance, ciprofloxacin is only reserved for cases of pyelonephritis that require deep tissue penetration. Nitrofurantoin had a low resistance rate of 1% and hence was deemed the antibiotic of choice for simple urinary tract infections, in line with local recommendations.(19)
This study had several limitations. First, given the setup of our national electronic healthcare records system, we were unable to ascertain if patients included in the study had been re-admitted to hospitals that were not restructured government hospitals, which would have skewed the results towards successful EDOU treatment. However, we postulate that this proportion would be very low, as almost all patients who were admitted to the EDOU received healthcare subsidies and were likely to opt to continue receiving them. Second, this was a single-centre retrospective study and had missing data on certain variables. As a single-centre study, the results may not be reproducible in other healthcare settings or apply to institutions with different patient demographics and prevalence of pyelonephritis. In addition, variables that had not been documented were regarded as being absent, and it is likely that the missing data led to underreporting of potential symptoms related to pyelonephritis.
Lastly, we relied upon clinical details, which can be ambiguous and challenging, to define the diagnosis.(13,20) Furthermore, the reviewers were not blinded to the study purpose, a possible source of selection bias. Our inclusion criteria may have been overly strict, as we wanted a high degree of certainty in the diagnosis. While the criteria were in line with the existing definition of acute pyelonephritis, patients may also present atypically, especially those who are pretreated with antibiotics in the outpatient setting, or geriatric patients.(21) This limitation may lead to misclassification bias, such that patients with acute pyelonephritis may not have been recognised. However, the misclassification would be non-differential in nature and had a similar chance of being in the EDOU success or failure groups.
In conclusion, the EDOU has been shown to be useful for both treatment of and observation for evolving signs of acute pyelonephritis in order to refine the eventual diagnosis. In our study, successful management in the EDOU was achieved in 100 (61.0%) patients. Urine cultures were sufficient for the identification of the culprit micro-organism. Patients who present with prominent symptoms of vomiting should have routine administration of antiemetics, while consideration for second-line antiemetics is recommended for those with persistent symptoms. Controlling symptoms of vomiting would promote better oral intake and may increase EDOU discharge rates.


