Abstract
INTRODUCTION
Epidural steroid injections are an integral part of nonsurgical management of radicular pain from lumbar spine disorders. We studied the effect of dexamethasone 8 mg epidural injections on the hypothalamic-pituitary-adrenal axis and serum glucose control of Asian patients.
METHODS
18 patients were recruited: six diabetics and 12 non-diabetics. Each patient received a total of dexamethasone 8 mg mixed with a local anaesthetic solution of lignocaine or bupivacaine, delivered into the epidural space. Levels of plasma cortisol, adrenocorticotropic hormone (ACTH), serum glucose after an overnight fast and two-hour postprandial glucose, as well as weight, body mass index, blood pressure and heart rate were measured within one week prior to the procedure (baseline) and at one, seven and 21 days after the procedure.
RESULTS
Median fasting blood glucose levels were significantly higher on post-procedure Day 1 than at baseline. However, there was no significant change in median two-hour postprandial blood glucose from baseline levels. At seven and 21 days, there was no significant difference in fasting or two-hour postprandial glucose levels. Both ACTH and serum cortisol were significantly reduced on Day 1 compared to baseline in all patients. There was no significant difference in ACTH and serum cortisol levels from baseline at Days 7 and 21.
CONCLUSION
Our study shows that epidural steroid injections with dexamethasone have a real, albeit limited, side effect on glucose and cortisol homeostasis in an Asian population presenting with lower back pain or sciatica.
INTRODUCTION
Administration of epidural steroids has been an accepted treatment modality for lower back pain and sciatica from degenerative spine disease for more than 50 years. Epidural steroid injections have been endorsed by the North American Spine Society and the Agency for Healthcare Research and Quality (formerly the Agency for Health Care Policy and Research) of the United States Department of Health and Human Services as an integral part of nonsurgical management of radicular pain from lumbar spine disorders.(1)
Robecchi and Capra first reported their treatment of a herniated lumbar disc in 1952 using hydrocortisone delivered epidurally, in order to place the steroid directly at the site of the affected nerve root.(2) This was followed by Lievre’s usage of peridurally placed steroids in 1957, with some success.(3) Adverse endocrine effects of systemic glucocorticoid therapy are well known. Data on adverse endocrine sequelae from epidural glucocorticoid injections exists,(4,5) but there are considerable variations in the dose, regime and type of steroids studied. Most studies used steroid-equivalent doses that were much higher than the dexamethasone 8 mg used routinely in our practice. Additionally, data from Asian patients is lacking.
Most previous studies examined the effects of particulate steroids, especially triamcinolone and methylprednisolone. Current evidence suggests that non-particulate epidural steroids are safer compared to particulate steroids.(6,7) In our centre, non-particulate dexamethasone is routinely used. Therefore, we studied the effect of dexamethasone 8 mg epidural injections on the hypothalamic-pituitary-adrenal (HPA) axis and serum glucose control of Asian patients.
METHODS
The study was approved by the local Institutional Review Board. A statistical power analysis indicated that at least ten patients needed to be recruited. Non-Asians with contraindications to epidural steroids and patients aged < 21 years and > 80 years were excluded. Patients who had deranged levels of baseline blood glucose, adrenocorticotropic hormone (ACTH) and cortisol would also be excluded, but none of the patients we recruited had these features.
After obtaining consent, 18 patients were recruited: six diabetics and 12 non-diabetics. Each patient received a total of dexamethasone 8 mg mixed with a local anaesthetic solution of lignocaine or bupivacaine, delivered into the epidural space. All patients were being treated for degenerative spine disease causing low back pain or sciatica, or both, and the procedure was part of their normal treatment plan. Within one week prior to the procedure (baseline), and at one, seven and 21 days after the procedure, plasma cortisol, ACTH and serum glucose levels (both after an overnight fast and two hours postprandial) as well as weight, body mass index (BMI), blood pressure and heart rate were measured. On the day of the procedure, only fasting blood sugar level was measured.
Results were analysed using IBM SPSS Statistics for Windows version 23.0 (IBM Corp, Armonk, NY, USA). Sample size calculation was based on ACTH levels. To achieve 80% power for the detection of an average ACTH decrease of 11 ng/L from baseline at the three time-point measurements (Days 1, 7 and 21), a sample size of ten patients was needed, assuming that the standard deviation was 9 ng/L.(8) Wilcoxon signed-rank test was used to compare baseline and post-procedure blood glucose, ACTH and cortisol levels. Multivariate analysis of variance with repeated measures was used to compare blood glucose, ACTH and cortisol levels at various time-points between diabetic and non-diabetic patients.
RESULTS
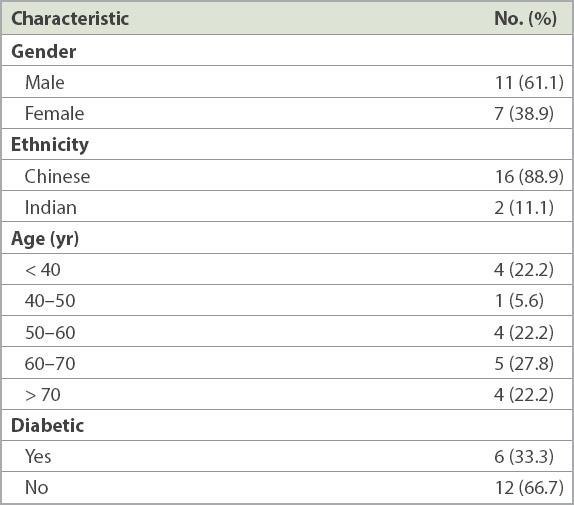
There were six diabetic and 12 non-diabetic Asian patients. Their median age was 59 years, and seven of the patients were women. There were two Indian patients and the rest were Chinese (
Table I
Characteristics of the study population (n = 18).
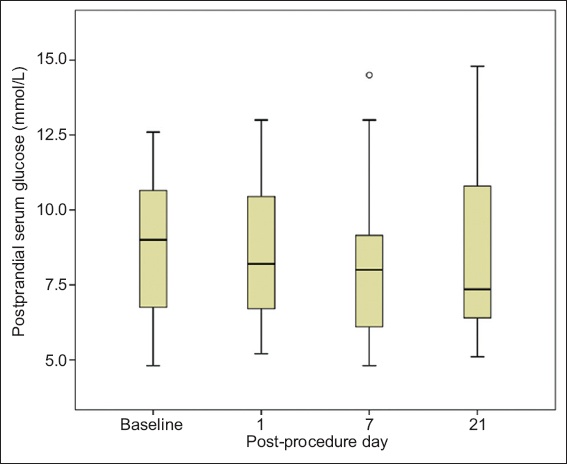
At post-procedure Day 1, the median fasting blood glucose level of 6.3 (interquartile range [IQR] 5.5–7.1) mmol/L was significantly higher than the baseline level of 5.3 (IQR 4.7–5.9) mmol/L (p = 0.026). However, there was no significant change in median two-hour postprandial blood glucose from baseline. At seven and 21 days post procedure, there was no significant difference in fasting or two-hour postprandial glucose levels (
Table II
Serum glucose control in diabetic and non-diabetic patients at various post-procedure time-points.
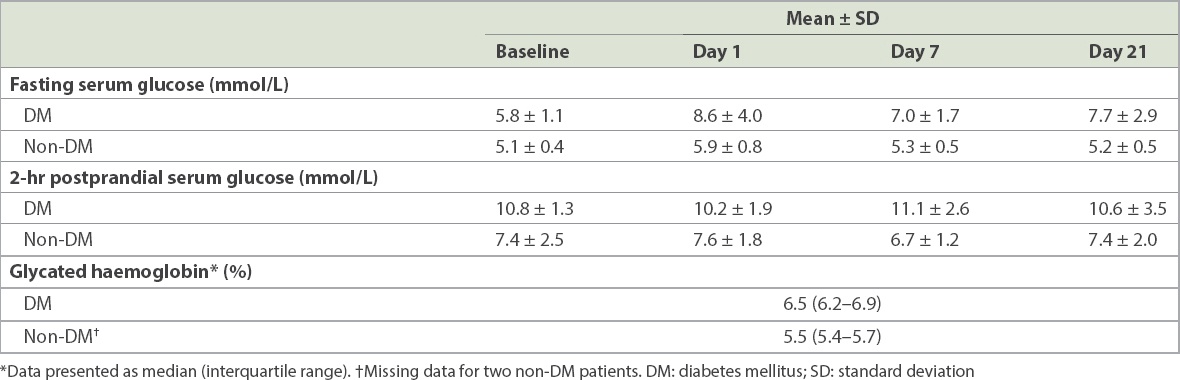
Fig. 1
Chart shows distribution of fasting serum glucose at various time-points, with p = 0.026 at one day post procedure versus baseline. * and ° represent extreme and outlier values, respectively.
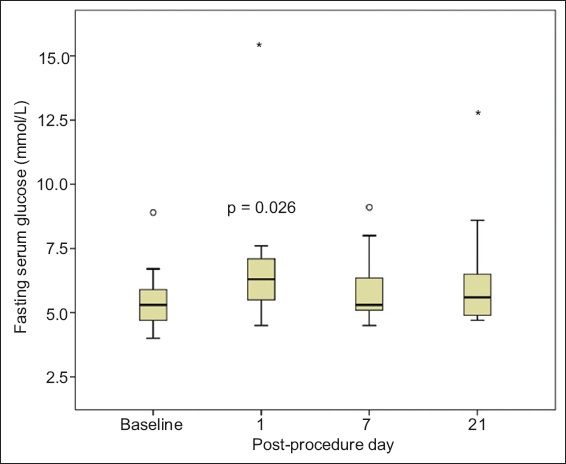
Fig. 2
Chart shows distribution of two-hour postprandial serum glucose at various time-points. ° represents outlier values.
Both ACTH and serum cortisol were significantly reduced at post-procedure Day 1 compared to baseline in all patients (both p < 0.001), decreasing to 7.0% and 7.6% (median) of baseline levels, respectively. At Day 7 and Day 21, there was no significant difference in ACTH and serum cortisol levels from the baseline (
Fig. 3
Charts show (a) distribution of serum adrenocorticotropic hormone (ACTH); and (b) distribution of serum cortisol at various time-points, with p = 0.001 at one day post procedure versus baseline. * and ° represent extreme and outlier values, respectively. One outlier patient with markedly lower baseline serum ACTH and cortisol levels compared to other patients was excluded from
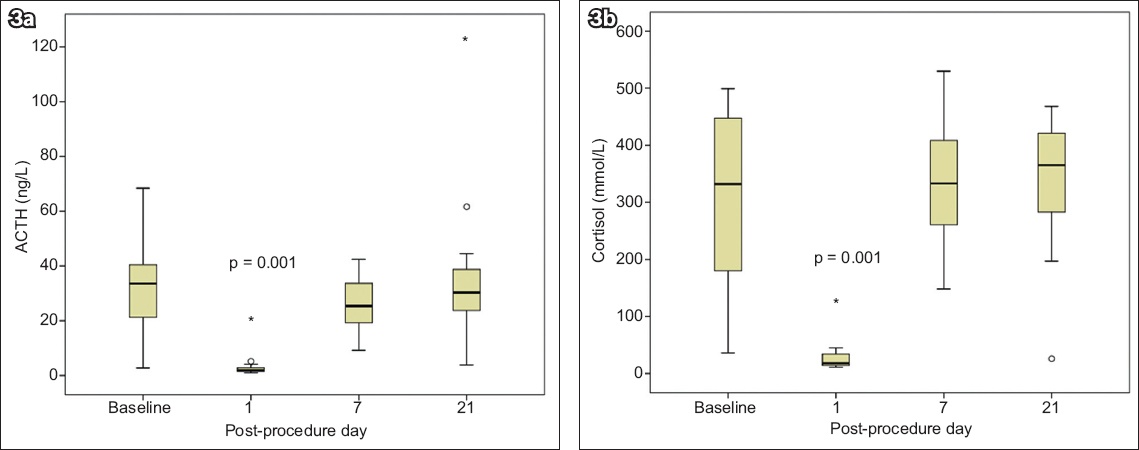
Of note was one patient who had significant adrenal suppression even at three weeks post procedure (ACTH 8.4% of baseline, cortisol 13.7% of baseline). Further investigation revealed that the patient was on mometasone, a steroid nasal spray from an ear, nose and throat specialist from one week post procedure. Another patient with diabetes mellitus had a significantly low ACTH level, which was 16.9% of baseline at three weeks post procedure. Her cortisol level during this time, however, was less significantly reduced at 69.5% of baseline. We also noted that she had severe gastroenteritis one week after the epidural steroids. In both these patients, the possible confounding factors were not present at the blood analysis on post-procedure Day 1.
All patients returned for blood analysis on the first day after the procedure. However, one patient required spine surgery within one week of the epidural procedure, and data was not collected at one and three weeks. Another patient had spine surgery 1–3 weeks post procedure, and his data was not collected at three weeks.
DISCUSSION
Glucocorticoids are used in the treatment of a myriad of diseases because of their anti-inflammatory and immunosuppressive effects.(9) However, the usage of systemic steroids is fraught with many side effects, one of which is suppression of the HPA axis. Abrupt withdrawal of ongoing glucocorticoid therapy can precipitate a life-threatening Addisonian crisis.(10)
Glucocorticoids are injected into joints for the treatment of arthritis, around tendons for tendinitis and via the neuraxial route for pain from spine disorders. The side effects of topical and single injections of steroids at various parts of the body may not be fully appreciated in clinical practice. However, adrenal suppression for variable periods has been reported from a single injection of steroids, as well as from topical applications.(4,5,11,12) Derangement of blood glucose levels has also been reported from topical,(13) intra-articular(14-17) and epidural steroid injections.(8,18)
Many studies on the endocrine side effects of epidural steroids used steroid-equivalent doses that were much higher than the dexamethasone 8 mg used routinely in our practice among Asian patients,(4,5,12) and it is possible that doses as low as dexamethasone 4 mg may offer the same efficacy.(19) Hence, we deemed it necessary to investigate the effect of the lower dose used in our practice on the HPA axis and blood glucose levels.
Non-particulate steroids such as dexamethasone may have a similar efficacy to particulate steroids,(20) with possibly a lower risk of embolic complications.(7) However, this claim is still controversial, as various other studies provide conflicting evidence with respect to their efficacy.(21-24) Nevertheless, various centres, including ours, have seen a change in practice in recent years, from using particulate to non-particulate steroids in the epidural space for treatment of spine-related pain. Hence, we felt the need to investigate the endocrine effects of non-particulate steroids such as dexamethasone.
The patients in this study were all Asians, with a median weight of 69.0 kg and a median BMI of 26.05 kg/m2. Significant adrenal suppression was present at post-procedure Day 1 in all patients. ACTH and cortisol decreased to 7% (median) and 7.6% (median) of the baseline, respectively. The median fasting blood glucose level was significantly higher at one day post procedure than at baseline (6.3 mmol/L vs. 5.3 mmol/L), but not at seven days or 21 days after the procedure. This observation was not reproduced with regard to higher postprandial blood glucose levels over any time period, even when the diabetic status of patients was accounted for in a separate analysis. Although diabetic patients had a trend of greater differences in absolute values of fasting serum glucose from baseline, this did not reach statistical significance. A larger follow-up study on diabetic patients would be useful to supplement our findings.
In a similar study by Ward et al,(5) ten patients with BMI of 26.7 (range 21.1–33.4) kg/m2, were administered 80 mg of triamcinolone (equivalent to dexamethasone 16 mg) via the caudal epidural route. Fasting insulin levels rose significantly from 11.6 mU/uL to 16.2 mU/uL (95% confidence interval [CI] 1.0–1.9; p = 0.03) one day after the epidural, and returned to normal by one week. Fasting glucose showed a similar pattern, rising from 4.7 mmol/L to 5.3 mmol/L (95% CI 1.0–1.2 mmol/L; p = 0.003) on the first day after steroid administration. Two subjects developed fasting hyperglycaemia with blood glucose levels of 6.4 mmol/L and 7.4 mmol/L at this time; with levels normalising by the follow-up visit at Day 7. There was marked adrenal suppression at both visits after the glucocorticoid epidural. Fasting cortisol fell from 352 nmol/uL to 49 nmol/uL (7.2-fold lower; 95% CI 4.0–12.9 nmol/uL; p < 0.001) within 24 hours and was still low on Day 7, at 96 nmol/uL. (3.5-fold lower; 95% CI 1.6–7.8 nmol/uL; p = 0.007).
Jacobs et al used 80 mg of methylprednisolone acetate (Depo-Medrol, equivalent to dexamethasone 16 mg), and reported suppression of the adrenocortical axis for up to three weeks following the injection.(11) In another study, Younes et al(8) showed that administering three epidural or intra-articular injections of 5.625 mg cortivazol at three-day intervals (equivalent to a total dose of 37.5 mg of dexamethasone) led to a suppression of the adrenocortical axis that persisted beyond 21 days. Systolic blood pressure increased transiently, and elevations in postprandial glucose levels lasted longer in diabetic than non-diabetic patients.
Thus, it can be inferred that the higher the dose of steroids and the greater the number of injections, the more prolonged and severe the degree of suppression of the adrenocortical axis as well as the derangement of glucose tolerance. The lowest dose of steroid necessary for pain control should be used. In a prospective study, Kim et al(25) randomised 100 patients with back pain of various aetiologies to receive either 40 mg or 20 mg of triamcinolone, an equivalent of 7.5 mg and 3.75 mg of dexamethasone, respectively, via translaminar, caudal or transforaminal routes. The study found that the group receiving 20 mg of triamcinolone experienced the same pain relief and had a similar rate of return to employment as the group receiving a higher dose of steroid, with lower derangements to glucose homeostasis. Another study by Kang et al(26) that focused on the minimum effective dose in treating radicular pain from herniated lumbar discs found that 10 mg of triamcinolone given transforaminally had the same effectiveness in pain relief when compared to 40 mg of triamcinolone, whereas triamcinolone 5 mg had inferior results. Clearly, there is a place for considering lower doses of steroids for epidural use than is currently practised.
In conclusion, epidural steroid injections are an established treatment modality for the alleviation of pain in patients with degenerative disease of the spine. Ultimately, our desire to relieve the suffering of our patients needs to be weighed against the potential for harm of the treatment. An optimal dose of steroid should be used in well-selected patients so as to maximise benefit while reducing the side effects. Our study shows that epidural steroid injections have a real, albeit limited, side effect on glucose and cortisol homeostasis in an Asian population presenting with lower back pain. To minimise the risks, more studies are required to establish the long-term effects of epidural steroid injections, the optimal dosage of the drug, and the recommended interval between injections.


