Abstract
INTRODUCTION
Disease outbreaks such as the COVID-19 pandemic significantly heighten the psychological stress of healthcare workers (HCWs). The objective of this study was to understand the factors contributing to the perceived stress levels of HCWs in a public primary care setting during the COVID-19 pandemic, including their training, protection and support (TPS), job stress (JS), and perceived stigma and interpersonal avoidance.
METHODS
This cross-sectional study using an electronic self-administered questionnaire was conducted at the National Healthcare Group Polyclinics in March 2020. Data was collected anonymously. Analysis was performed using regression modelling.
RESULTS
The response rate was 69.7% (n = 1,040). The mean perceived stress level of HCWs in various departments ranged from 17.2 to 20.3. Respondents who reported higher perceived stress were those who made alternative living arrangements, were more affected by the current pandemic, reported higher JS and were Muslims. Respondents who reported lower perceived stress were those who had been through the severe acute respiratory syndrome epidemic in 2003 and H1N1 pandemic in 2009 as HCWs, and those who had higher confidence in the organisation’s TPS.
CONCLUSION
All HCWs, regardless of their scope of work, were similarly stressed by the current pandemic compared to the general population. Improving the confidence of HCWs in their training, protection and the support of personal protective equipment, and retaining experienced HCWs who can provide advice and emotional support to younger colleagues are important. Adequate psychological support for HCWs in the pandemic can be transformed into reserves of psychological resilience for future disease outbreaks.
INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes COVID-19, is a novel virus that was reported in December 2019. With the subsequent global impact of the virus, COVID-19 was declared a pandemic by the World Health Organization on 11 March 2020.(1) Unlike the severe acute respiratory syndrome (SARS), which infected 20% of healthcare workers (HCWs) worldwide with minimal community transmission as most carriers were symptomatic,(2) COVID-19 has wider community transmission owing to its capability to be transmitted even when carriers are asymptomatic.(3) Hence, COVID-19 has resulted in a higher death count globally than SARS. The pandemic has overwhelmed healthcare systems in many countries owing to the sudden surge in demand for intensive care unit beds and ventilators.
Disease outbreaks significantly heighten the psychological stress level of medical staff.(4-8) Many factors can contribute to the distress experienced by HCWs during COVID-19, including rapidly changing medical information and procedures; overwhelming infection control procedures; increasing JS; reduced contact and interaction between colleagues, friends and family; and stigma.(9) The stress level of an individual depends on his appraisal of the significance of the stressor and his coping abilities within a person-environmental transaction.(10) When stress levels exceed an individual’s ability to cope over a prolonged period, burnout and a wide spectrum of health-related concerns can ensue.(11,12) In a commentary, Sim and Chua(13) reiterated that the psychological well-being of HCWs dealing with disease outbreaks is a priority area for research, and enhancing the psychological well-being of HCWs is a crucial tool in the continuing vigilance and fight against emerging infectious diseases.
Hospital-based medical staff such as doctors and nurses are directly involved in the diagnosis, treatment and care of patients with COVID-19. Community-based medical staff function as gatekeepers to screen a high volume of unknown cases based on careful history-taking and physical examination. High-risk cases are then referred to the hospital for further investigation. Many studies have explored the psychological impact, mainly on doctors and nurses in the hospital setting, during and after major novel communicable disease outbreaks.(4-8) Fewer studies looked at HCWs in the primary care setting.
Medical staff in the primary care setting are supported by a wide range of other HCWs who deliver care and services to the sick indirectly as aides, helpers, laboratory technicians and even medical waste handlers.(14) They toil for long hours and are at risk of developing occupational stress and burnout as well. During an infectious disease outbreak, they may be stigmatised by the public and their perceived stress level may be higher than before the outbreak as they still have to deal with the usual stressors of daily life and family. During the SARS epidemic, the prevalence of psychiatric morbidities in medical staff within a primary healthcare setting was found to be about 20.6% in Singapore.(15) However, limited studies have explored non-medical HCWs in the primary care setting.
This study aims to examine the perceived stress levels of HCWs in a public primary care setting during the pandemic, taking into account their demographics; training, protection and support (TPS); job stress (JS); and perceived stigma and interpersonal avoidance (PSIA). Understanding the extent and magnitude of such psychological impact and associated factors can help healthcare organisations and policymakers to review and improve psychological support for our HCWs working in the primary healthcare setting in current and future outbreaks.
METHODS
The study was conducted in the National Healthcare Group Polyclinics (NHGP), which has six polyclinics in the central and northern parts of Singapore. NHGP is one of the three public primary healthcare delivery networks providing comprehensive primary care in the country.
Singapore announced the change in the Disease Outbreak Response System Condition (DORSCON) for COVID-19 from Yellow to Orange on 7 February 2020. The survey was conducted from 13 March to 24 March 2020, approximately one month after the announcement of DORSCON Orange.(16) DORSCON Orange indicates that the disease is severe and spreads easily from person to person but that it has not spread widely in Singapore and is being contained. During the period that the survey was conducted, the number of COVID-19 cases in Singapore rose from 187 to 509 with two deaths reported.(17) There were also several new infection clusters identified at places of worships and a gym. Subsequently, the Singapore government implemented tighter measures that included tighter border controls, stay-home notices, quarantine orders and social distancing measures.(18) All companies and organisations were advised to introduce working from home as much as possible.(19) Across the border, the Malaysian government implemented a lockdown from 18 March to 31 March 2020, which affected about 300,000 Malaysian workers who usually commute daily to work in Singapore, and many of them had to make urgent alternative living arrangements in Singapore.(20,21)
Prior to 13 March 2020, many members of the public expressed concern about the steady double-digit daily increase in COVID-19 cases and the healthcare system’s capacity to manage them.(22) Businesses were hit by social distancing measures, and many individuals had their jobs affected. The government sought to address these concerns by rolling out an SGD 6-billion economic support package.(23) When the survey was conducted in March 2020, point-of-care testing for COVID-19 had not yet been implemented at the polyclinics. All suspected cases were referred to the National Centre for Infectious Diseases.
The PROTECT (Psychological Readiness and Occupational Training Enhancement during COVID-19 Time) study was conducted using a cross-sectional survey design, using a self-administered anonymous online questionnaire. Ethics approval was obtained from the National Healthcare Group (NHG) Domain Specific Review Board (ethics reference no. 2020/00218).
Total population sampling was carried out. Invitation emails were sent to all NHGP employees based in the six polyclinics. Participation in the survey was voluntary. Staff with no email accounts were invited by their supervisors to access the online questionnaire via the organisation’s intranet homepage. Both the email and the intranet homepage provided a link to the electronic questionnaire on the NHG Research Electronic Data Capture (REDCap) platform. This is a secure Web-based platform that can only be accessed within the corporate enterprise environment to capture data for clinical research. A total of 1,492 employees in the six polyclinics were invited to participate in this survey. Reminders were sent to all participants and supervisors during the survey period. The questionnaire took about five minutes to complete.
The outcome variable was the score on the Perceived Stress Scale (PSS).(24) The PSS, developed by Cohen, Kamarck and Mermelstein,(24) is a well-established self-reported survey based on the psychological conceptualisation of stress and measures perceived as personal stress. It is a ten-item scale that measures the degree to which situations in one’s life are viewed as demanding and stressful. Items are rated on a five-point scale, ranging from 0 (never) to 4 (very often) (Appendix 1). The scale has been validated in several countries in Asia(25-29) and was previously described in another local study on healthcare professionals, where the reported Cronbach’s alpha was 0.84.(30)
Independent variables were (a) TPS, (b) JS and (c) PSIA.(31) We adopted the 18-item questionnaire consisting of these three scales with a Cronbach’s alpha of 0.89, 0.76 and 0.77, respectively. Ten employees were invited to complete the questionnaire as a pilot to test its face and content validity, and the questionnaire was modified according to their feedback. Items were scored on a five-point scale from 1 (very confident that this is false) to 5 (very confident that this is true) for TPS (Appendix 2) and from 1 (strongly disagree) to 5 (strongly agree) for JS and PSIA (Appendix 3). The survey also collected data on respondents’ demographics (e.g. age, gender, marital status, religion) and profiles, including (a) changes to living arrangement due to the COVID-19 outbreak, (b) whether they were in direct contact with patients, (c) how they were affected by the current and previous disease outbreaks in Singapore (SARS in 2003, H1N1 in 2009 and COVID-19) and (d) how long they had worked in the healthcare setting, subcategorised into: < 2 years, 2–10 years, 11–17 years and > 17 years to reflect their experience as HCWs during H1N1 and SARS 11 years and 17 years ago, respectively.
Data analysis was performed using IBM SPSS Statistics version 24.0 (IBM Corp, Armonk, NY, USA). Preliminary data checking was performed to test for normality for PSS using the Kolmogorov-Smirnov test. Descriptive statistics were calculated for all variables and presented as mean ± standard deviation or median with interquartile range. Regression modelling was conducted with perceived stress level as the dependent variable and respondents’ demographic characteristics and profiles, TPS, JS and PSIA as independent variables, where unadjusted, adjusted means, medians and beta coefficients for each variable were provided. A p-value < 0.05 was considered statistically significant. A multicollinearity test was performed to remove independent variables that were correlated to each other where necessary.
RESULTS
Out of the 1,492 eligible participants, a total of 1,040 clinic employees responded to our survey, giving a response rate of 69.7%.
Table I
Demographics and profile of clinic staff (n = 1,040).
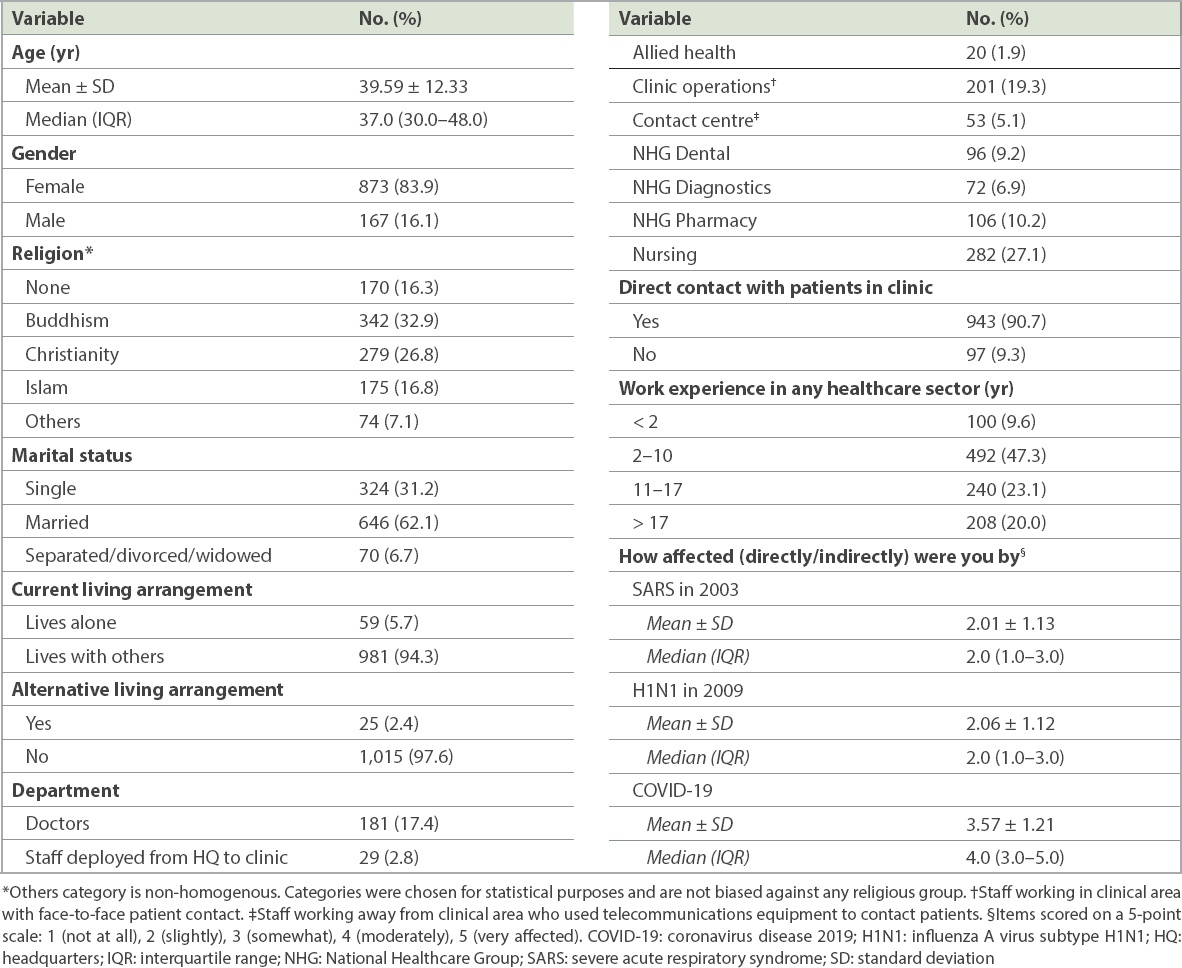
Table II
Training, protection and support, job stress, and perceived stigma and interpersonal avoidance for clinic staff (n = 1,040).
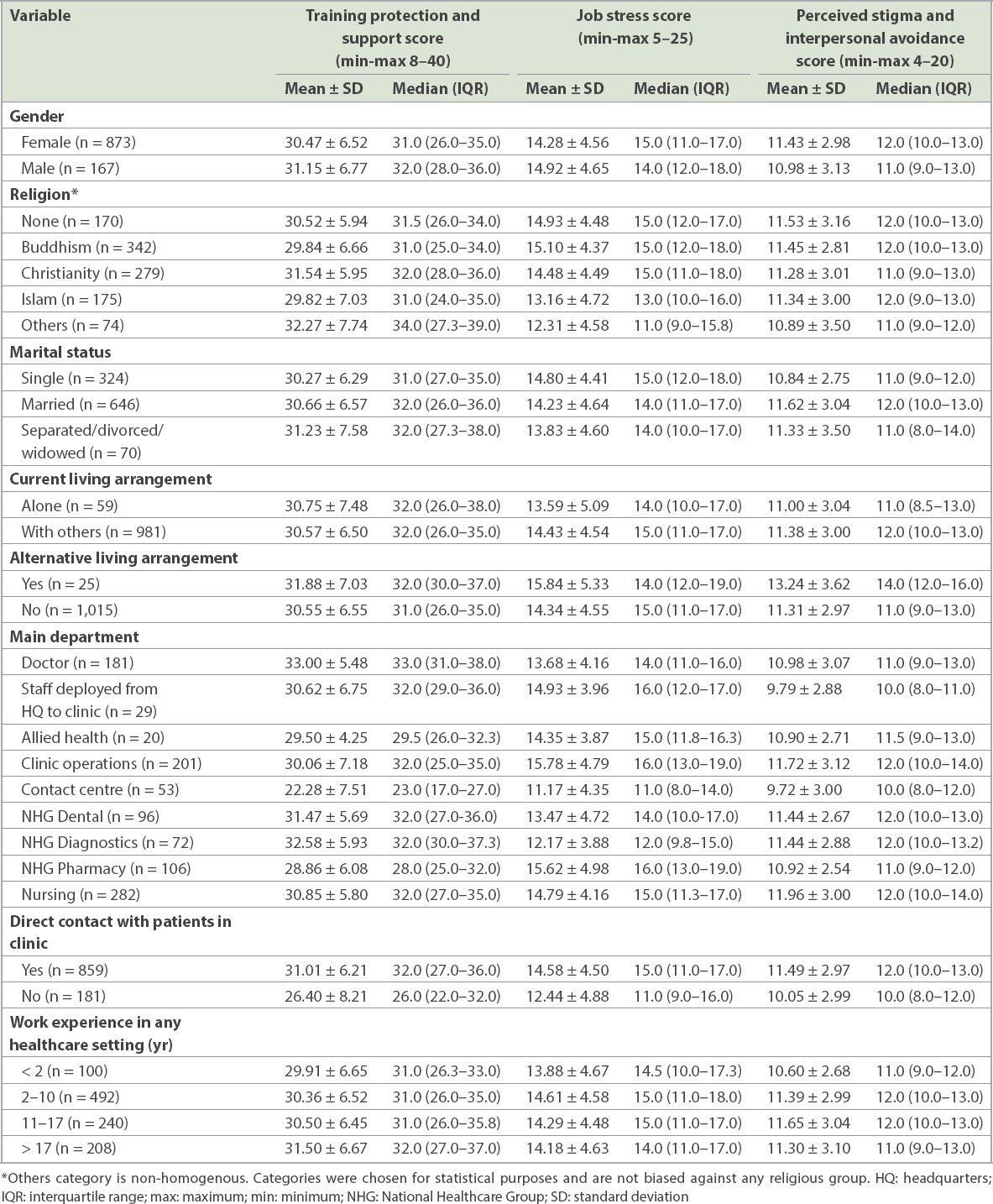
Doctors had the highest (mean 33.00 ± 5.48) and contact centre staff had the lowest (mean 22.28 ± 7.51) TPS scores. Staff with direct patient contact reported higher mean TPS scores (31.01 ± 6.21) compared to those who did not have direct patient contact (26.40 ± 8.21). Staff who worked for more than 17 years reported the highest mean TPS scores (31.50 ± 6.67) and staff who worked less than two years reported the lowest mean TPS scores (29.91 ± 6.65).
Staff who stayed alone reported lower mean JS (13.59 ± 5.09) compared to those who lived with others (14.43 ± 4.54). Staff who made alternative living arrangements reported higher mean JS (15.84 ± 5.33) compared to staff who did not do so (14.34 ± 4.55). Clinic operations staff reported the highest score for JS (15.78 ± 4.79), while contact centre staff reported the lowest (11.17 ± 4.35). Staff with direct patient contact reported higher mean JS scores (14.58 ± 4.50) compared to those who did not have direct patient contact (12.44 ± 4.88). Staff who worked for 2–10 years reported the highest mean JS scores (14.61 ± 4.58), while staff who worked for less than two years reported the lowest (13.88 ± 4.67).
Staff who made alternative living arrangements reported higher mean PSIA scores (13.24 ± 3.62) compared to staff who did not do so (11.31 ± 2.97). Nurses reported the highest score for PSIA (11.96 ± 3.00) while staff from the contact centre reported the lowest score (9.72 ± 3.00). Staff with direct patient contact reported higher mean PSIA score (11.49 ± 2.97) compared to those who do not have direct patient contact (10.05 ± 2.99). Staff with less than two years of experience in healthcare reported the lowest mean PSIA score (10.60 ± 2.68).
Table III
Effect of different factors on the perceived stress of healthcare workers in a public healthcare setting (n = 1,040).
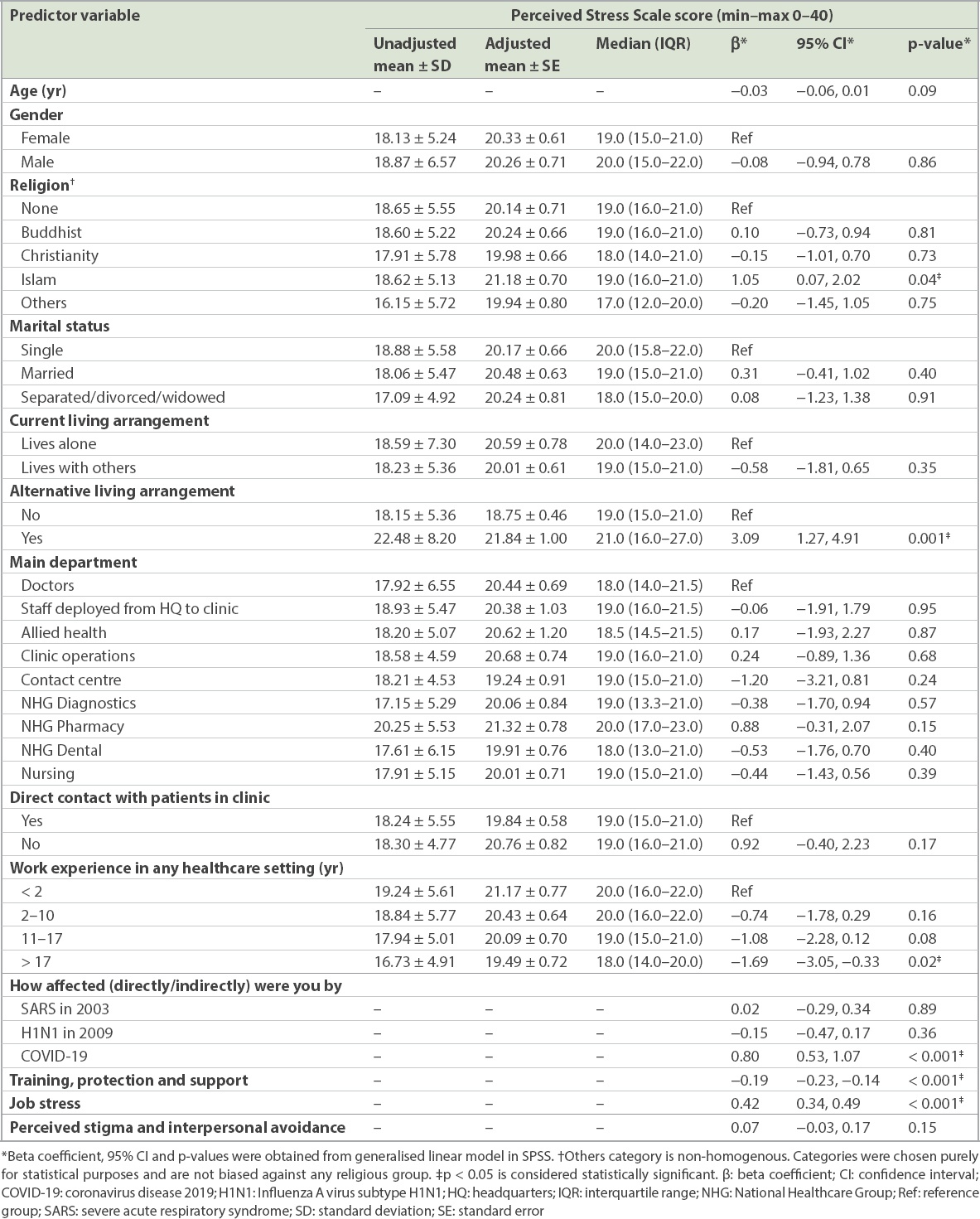
Six independent variables were significantly associated with perceived stress level. Respondents of Islamic faith reported higher perceived stress levels as compared to those with no religious faith (p = 0.04). Those who made alternative living arrangement during the pandemic reported higher perceived stress levels as compared to those who did not (p = 0.001). Respondents who had more than 17 years of healthcare experience (i.e. had been through the SARS and H1N1 epidemic and pandemic) reported lower perceived stress levels as compared to those who had less than two years of work experience in healthcare (p = 0.02). Those who reported being more affected by the current pandemic reported higher perceived stress levels (p < 0.001). Respondents who reported higher confidence in TPS by the organisation reported lower perceived stress levels (p < 0.001). Lastly, those who reported higher JS during the pandemic also reported higher perceived stress levels (p < 0.001).
DISCUSSION
This study found that there was no statistically significant difference in the perceived stress level among respondents from the different departments within the National Healthcare Group Polyclinics. Perceived stress level was reported to be statistically significantly higher for HCWs who: (a) were Muslims compared to those who were atheists; (b) made alternative living arrangements compared to those who did not make such arrangements; (c) were more affected (directly or indirectly) by the current pandemic; and (d) reported higher JS. Conversely, perceived stress level was reported to be lower for HCWs who (a) had more than 17 years of healthcare working experience compared to those who had less than two years of experience and (b) reported higher perceived occupational TPS from the organisation.
Based on a previous study, the baseline PSS level of the general Singapore population prior to the COVID-19 pandemic was estimated to be between 16.0 and 17.0.(32) Our study showed that the perceived stress level of HCWs in the various departments ranged from 17.2 to 20.3. This suggests that the COVID-19 pandemic had a considerable impact on the psychological stress level of HCWs in the primary care setting. This increase in stress level may have been contributed by the demands on HCWs during the COVID-19 pandemic. In addition to ensuring adequate infection control for patients during face-to-face consults at the polyclinics, new workflows to manage patients remotely were also introduced during this time. These included teleconsultations and medication extensions for patients with chronic illnesses who were clinically stable and without any signs or symptoms of COVID-19. Other possible contributors to increased psychological stress for the HCWs were the frequent changes in workflows in response to the growing spread of COVID-19 internationally and, locally, the requirements for rapid data submission, dealing with logistic challenges and working in split teams.
In contrast with another study conducted in several tertiary settings in Singapore between 19 February and 13 March 2020, which showed that the prevalence of anxiety and stress was higher among non-medical HCWs than medical personnel,(8) our study found that the perceived stress level was similar across the different job scopes in the primary care setting. This result was also supported by our finding that there was no statistical difference in perceived stress level between HCWs who had direct and those who had no direct contact with patients. These findings suggest that during a pandemic, demands on primary care services result in increased psychological stress for all HCWs in primary care, including operations support staff.
There may be several reasons for the higher perceived stress reported by Muslim HCWs in this survey. Firstly, it is common practice for Singaporean Muslims to go on a minor religious pilgrimage during the March school holidays. However, Muslim HCWs had to cancel all their overseas leave during this period. Secondly, on 15 March, the Islamic Religious Council of Singapore reported that five Singaporeans who tested positive for COVID-19 had visited ten different local mosques during their infectious period. These occurrences may have contributed to increased stress among some Muslim HCWs.
Several HCWs in our study made alternative living arrangements on their own accord to reduce the chances of passing the infection to their family members if they contracted the virus. A small number of HCWs who commute daily between Singapore and Malaysia were also affected by Malaysia’s announcement of a two-week lockdown on 18 March. They were forced to look for an alternative living arrangement in Singapore or risked not being able to work during the whole lockdown period. Even though the organisation worked quickly with all HCWs affected to find and provide alternative living arrangements as soon as possible, it would not be surprising for these HCWs to report a higher perceived stress level, as they would not be able to see their family members and had to adapt to new living arrangements.
HCWs who had 17 years of work experience in healthcare would have experienced SARS in 2003 and H1N1 in 2009. Interestingly, these more experienced HCWs were more psychologically prepared to cope with the new pandemic compared to those who were relatively new to the healthcare industry. Age was not a confounding factor, as it was accounted for in the regression analysis. Having previous work experience as a healthcare worker when SARS and H1N1 outbreaks occurred, and not just the H1N1 pandemic, may reduce rather than worsen stress.
Shanafelt et al(33) described that in dealing with a pandemic such as COVID-19, HCWs wanted to be heard, protected, supported, cared for and well-prepared through infection control training by the organisation, as they are putting themselves at risk of being infected when they work at the front line. In our study, HCWs who were confident in the TPS provided by the organisation reported lower perceived stress levels as compared to those who were less confident. In general, HCWs who were in direct contact with patients tended to report higher TPS scores compared to HCWs with no patient contact. A contributing factor to this finding may be that during the survey period, HCWs who had no direct contact with patients were not provided face masks in order to conserve the supply of face masks for HCWs who were in direct contact with patients. This practice was in accordance with the Ministry of Health’s recommendations when there was no evidence of community spread of COVID-19 in Singapore. The recommendation then was to only wear a mask when one was sick or had active symptoms. This recommendation has since been reversed by the ministry as of 4 April 2020.(34) All HCWs are now provided with appropriate face masks based on their risk of exposure.
PSIA was not associated with perceived stress level. This may have been a result of the efforts by the Ministry of Health, the Singapore media and the organisations that encouraged widespread community support to HCWs during the pandemic. Within NHGP, morale boosters for HCWs included regular distribution to HCWs of care packs that contained fruit cups, sanitisers and handwritten thank-you cards by community members thanking and encouraging HCWs in their ongoing frontline work.
This study had some limitations. As the survey was administered via the organisation’s intranet, the survey link worked only if an electronic device was connected to the organisation’s Wi-Fi or wired network. The study team chose this method to ensure that all respondents were genuine employees of the organisation. However, staff without an organisation email or easy access to the intranet might not have participated in this survey. Despite this, an overall response rate of about 70% was achieved, with good representation of all the departments at the polyclinics. Moreover, the proportion of women who participated in the survey was 83.9%, similar to the proportion of the female gender in our organisation’s workforce. These results supported the validity of our finding.
The perceived TPS, JS and PSIA scales had not previously been validated in Singapore. However, the research team piloted these scales, found good face and content validity, and made some modifications before proceeding with their utilisation. In terms of reliability, both the TPS scale (0.94) and the JS scale (0.82) had a better Cronbach’s alpha compared to Maunder et al’s 0.89 and 0.76, respectively.(31) The Cronbach’s alpha for PSIA was 0.58, indicating that it had poor internal consistency, unlike Maunder et al’s 0.77.(31) After careful scrutiny, we postulate that the two perceived stigma questions and the two perceived interpersonal avoidance questions seemed to belong to two different constructs and may not be a suitable scale in our local context for future use.
We did not measure other domains of psychological distress such as depression, anxiety and post-traumatic disorder. We decided that it was inappropriate to measure known psychiatric disorders for an anonymous survey and also may not have been able to reach out to the respondents who were severely distressed. Contact information for in-house psychological support was provided for respondents on the last page of our survey.
In conclusion, our study showed that regardless of the scope of work involved, all HCWs were similarly stressed by the recent COVID-19 pandemic. Despite the measures put in place by the organisation to mitigate the negative psychological impact of COVID-19, some HCWs may be at a higher risk of developing more stress. The study results suggest that it is important to provide adequate infection control training for our HCWs, and to retain experienced HCWs who can provide helpful advice and be positive role models for their younger colleagues during such a trying time. It also underpins the importance of providing adequate psychological support for the workforce so that the current stressful experience can be transformed into reserves of psychological resilience for future disease outbreaks.
As the COVID-19 pandemic is likely going to last for some time, with the number of infected cases rising to more than 9,000 as of 21 April 2020, the study team will continue to study how the perceived stress level may change over time as the government implements further measures to curb the spread of COVID-19. The results of this and future studies could help to improve the current system to sustain a healthy and resilient work environment.
ACKNOWLEDGEMENTS
The authors would like to thank the following colleagues from National Healthcare Group Polyclinics: Mr Eugene Lim Guo Shun for his help in setting up the questionnaire and keeping track of the participation rate; Mr Jeremy Lew Kaiwei for assisting with the statistical analysis; Dr Simon Lee Biing Ming, Dr Karen Ng Ming Yann, Dr Christopher Chong Wern Siew, Dr Jonathan Ting Sing Shing, Dr Liu Changwei, Dr Kong Jing Wen, Dr Tan Khai Wei, Dr Evan Sim Chin Sing, Dr Lim Ziliang, Dr Kenneth Low Meng Tze, Ms Tracy Gan Seok Bee, Ms Chen Yee Chui, Ms Lim Voon Hooi, Ms Chew Geok Lan, Ms Chan Soo Chung, Ms Lim Li Ching and Ms Lim Soh Har for helping us to plan the study and/or garner support in their respective departments to do the survey; Ms Jayalakshmy Aarthi Anathanarayanan for providing us with the information on peer support; Mr Chow Zi Siong for providing up-to-date information about the COVID-19 situation in Singapore during the survey period; and finally, Dr Gowri Doraisamy and Ms Noraizah Binte Zainal Abidin for their valuable comments on the study findings. This study would not have been possible without their help. This research was supported by the Singapore Ministry of Health’s National Medical Research Council under the Centre Grant Programme (reference no. NMRC/CG/C019/2017).
SMJ-63-149-Appendix.pdf


