Abstract
INTRODUCTION
Perioperative glycaemic control is an important aspect of clinical management in diabetic patients undergoing cataract surgery under local anaesthesia. While poor long-term glycaemic control has significant implications for surgery, perioperative hypoglycaemia or hyperglycaemia may also compromise patient safety and surgical outcomes. We aimed to survey ophthalmologists and anaesthesiologists on their approach and to identify the prevalent practice patterns in Singapore.
METHODS
This was a cross-sectional questionnaire-based survey conducted in four public hospitals in Singapore with established ophthalmology and anaesthesia units. Respondents were approached individually, and the self-administered questionnaires comprised questions related to practice patterns, clinical scenarios and awareness of pre-existing guidelines.
RESULTS
A total of 129 doctors responded to the questionnaire survey. 76 (58.9%) were from ophthalmology departments and 53 (41.1%) were from anaesthesia departments. The majority chose to withhold oral hypoglycaemic agents (82.9%) and/or insulin (69.8%), and keep the patient fasted preoperatively. A blood glucose level ≥ 17 mmol/L prompted 86.0%–93.8% of respondents to adopt a treat-and-defer strategy, while a level ≥ 23 mmol/L prompted 86.0%–96.9% of respondents to cancel the cataract surgery. The respondents were consistently more concerned about perioperative hyperglycaemia (n = 99, 76.7%) than intraoperative hypoglycaemia (n = 83, 64.3%).
CONCLUSION
The current study presented the prevalent practice patterns of ophthalmologists and anaesthesiologists in the perioperative management of diabetic patients undergoing cataract surgery in four public hospitals in Singapore. Further research in this field is required, and may be useful for the future formulation of formal guidelines and protocols.
INTRODUCTION
The association between diabetes mellitus and cataracts is well established.(1) Apart from sight-threatening retinopathy, cataracts are a major cause of visual impairment and blindness in diabetic patients. Surgery is the standard of care and a cost-effective solution(2) for restoring vision and improving the quality of life of diabetic patients with visually significant cataracts. With disease prevalence expected to increase worldwide, the global burden of diabetes mellitus and its complications is likely to rise.(3) Other predictors of a rise in cataract surgery performed on diabetic patients are population ageing, improved healthcare delivery and increased demand for good vision.
There are several surgical considerations for diabetic patients who require cataract operations. Poor long-term glycaemic control not only inherently predisposes the individual to various systemic complications of diabetes mellitus and cardiovascular morbidity, but also increases the risks of anaesthesia and may lead to a poor surgical outcome. Diabetics have also been shown to have a higher risk of infection,(4,5) postoperative inflammation(6,7) and delayed wound healing.(8) In addition, cataract surgery may result in the progression of diabetic retinopathy and macular oedema.(9,10) Lastly, stress response to surgery may result in postoperative hyperglycaemia, particularly during general anaesthesia.(11) For these reasons, as well as others, local anaesthetic techniques are preferred.
While poor long-term glycaemic control has significant implications for surgery, perioperative hypoglycaemia or hyperglycaemia may further compromise patient safety and surgical outcomes. Such issues are frequently encountered in the surgical setting. Yet, in practice, preventive and management strategies vary vastly between clinicians and institutions. To the best of our knowledge, there is currently no internationally accepted guideline or consensus on clinical decision-making pertaining to perioperative glucose control. In this study, we aimed to survey local ophthalmologists and anaesthesiologists on their approach to this common clinical problem and thereby identify prevalent practice patterns that may be useful for the formulation of management algorithms in future.
METHODS
This cross-sectional questionnaire-based survey was conducted in four public hospitals in Singapore that have established ophthalmology and anaesthesia units, namely Alexandra Hospital, National University Hospital, Tan Tock Seng Hospital and Changi General Hospital, over a period of four months. Doctors in the two departments were approached individually during their working hours by the study team and the questionnaires were completed after they gave informed verbal consent. The study was approved by the local ethical review board and complied with its policies.
The questionnaire was self-administered and anonymous. It comprised four sections: baseline information, practice patterns, clinical scenarios and awareness of guidelines. Firstly, baseline information was collected, including the respondents’ speciality (ophthalmology or anaesthesia) and grade of appointment (senior consultant, consultant or associate consultant, registrar, medical officer, etc). Secondly, respondents were asked to indicate their preferred preoperative regimen for diabetic patients on oral hypoglycaemic agents (OHGA) and/or insulin. For patients on OHGA, the options included: (a) withhold the agent and keep the patient fasted; (b) withhold the agent, keep the patient fasted and commence glucose-potassium-insulin (GKI) therapy or its equivalent; and (c) have the patient consume the agent with the usual breakfast. For patients on insulin therapy, the options included: (a) withhold the insulin and keep the patient fasted; (b) withhold insulin, keep the patient fasted and commence GKI therapy or its equivalent; (c) reduce the insulin dose while the patient is fasting; (d) reduce the insulin dose while maintaining the patient’s usual diet; and (e) maintain the usual insulin dose with the usual diet. Respondents were also asked whether the blood glucose level of patients was routinely checked perioperatively.
Thirdly, the respondents were told to indicate the level of blood glucose that would prompt them to institute treatment and delay surgery on the same day (treat and defer) or cancel surgery. They were also asked if they had ever cancelled cataract surgery due to poor diabetic control in patients and to identify their greatest concern (between intraoperative hypoglycaemia and poorly controlled perioperative hyperglycaemia) in this group of patients. The respondents were asked if they had ever cancelled cataract surgery for a diabetic patient. Lastly, respondents were questioned to find out their awareness of guidelines for the management of perioperative glucose levels.
RESULTS
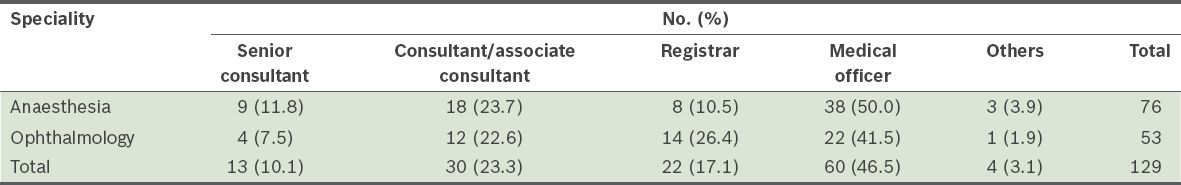
A total of 129 doctors responded to the questionnaire survey (
Table I
Respondents by speciality and grade of appointment (n = 129).
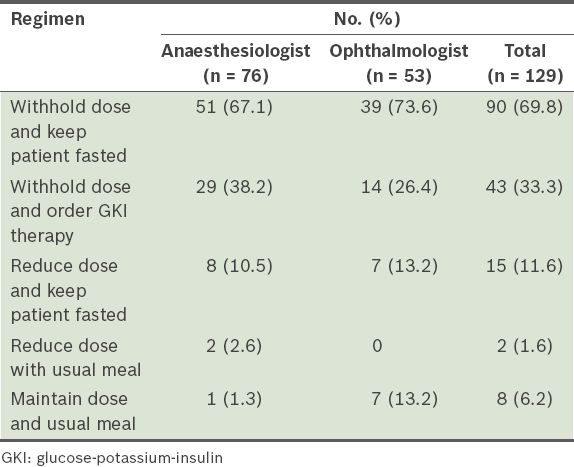
In terms of their preferred practice patterns for the preoperative regimen (Tables
Table II
Preoperative regimens that respondents preferred for patients on oral hypoglycaemic agents.
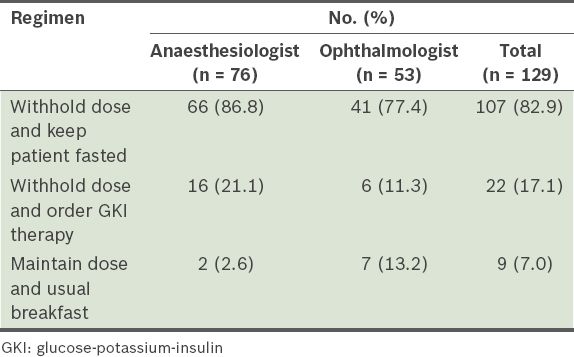
Table III
Preoperative regimens that respondents preferred for patients on insulin.
Most of the respondents (n = 110, 85.3%) routinely performed a preoperative check on the blood glucose levels of patients. Almost half (n = 59, 45.7%) of all the respondents checked blood glucose levels immediately before surgery, while 34.1% (n = 44) performed the test after surgery. Among the 76 anaesthesiologists, 81.6% (n = 62) checked blood glucose levels preoperatively and 34.2% (n = 26) immediately before surgery, while 11.8% (n = 9) and 43.4% (n = 33) performed a check during and after the operation, respectively. Similarly, 90.6% (n = 48) of the 53 ophthalmology doctors checked blood glucose level preoperatively, 49.1% (n = 26) immediately before surgery, while 5.7% (n = 3) and 20.8% (n = 11) performed the test during and after the operation, respectively.
Regarding the blood glucose level that would prompt them to consider a treat-and-defer strategy for diabetic patients undergoing cataract surgery, most respondents (86.0%–93.8%) indicated a level ≥ 17 mmol/L. A total of 48 (37.2%) respondents would institute treatment for patients with a blood glucose level of 2–5 mmol/L, while 40 (31.0%) respondents would do so for a level of 11–16 mmol/L (
Fig. 1
Graph shows the blood glucose levels that would prompt respondents to treat and defer cataract surgery.
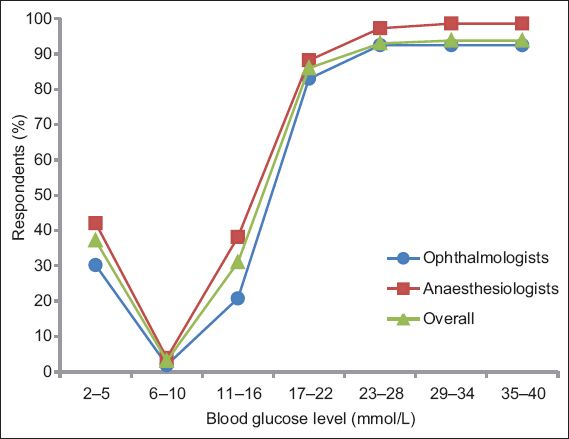
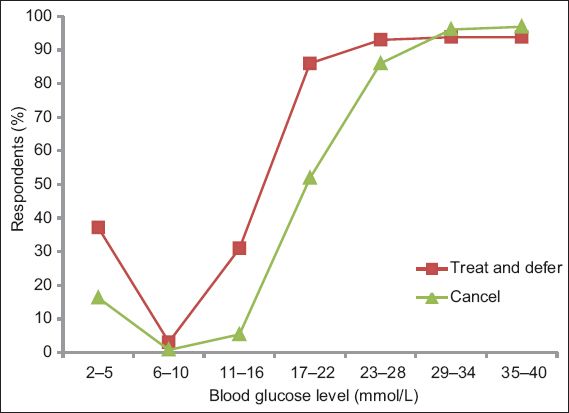
Fig. 2
Graph shows the blood glucose levels that would prompt respondents to cancel cataract surgery.
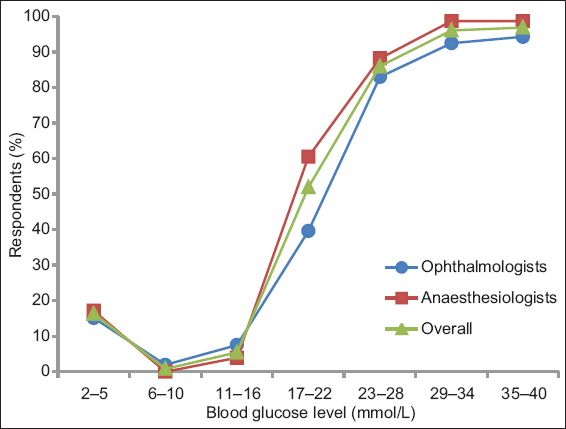
Fig. 3
Graph shows the comparison between respondents who would chose to treat and defer or cancel cataract surgery at different blood glucose levels.
The respondents were consistently more concerned about perioperative hyperglycaemia (n = 99, 76.7%) than intraoperative hypoglycaemia (n = 83, 64.3%). This was also observed among anaesthesiologists (hypoglycaemia: n = 51, 67.1%; hyperglycaemia: n = 60, 78.9%) and ophthalmologists (hypoglycaemia: n = 32, 60.4%; hyperglycaemia: n = 39, 73.6%). Only 55.8% (n = 72) of the respondents had ever cancelled cataract surgery for a diabetic patient (ophthalmologists: n = 43, 81.1%; anaesthesiologists: n = 29, 38.2%). In terms of their awareness of existing guidelines for the management of perioperative blood glucose levels, 83.7% (n = 108) of all respondents were not aware of any existing protocols or guidelines (anaesthesiologists: n = 69, 90.8%; ophthalmologists: n = 39, 73.6%).
DISCUSSION
Currently, there is no internationally accepted guideline specifically for the perioperative management of diabetic patients undergoing cataract surgery. Similarly, the majority of clinicians (n = 108, 83.7%) surveyed in the current study were not aware of any pre-existing protocols or guidelines. Yet, both long-term and acute glycaemic control (in the surgical setting) is multifactorial, and management may be complicated and variable. There is also very limited data specifying optimal treatment goals in the perioperative management of a diabetic patient. As such, a universal ‘one-size-fits-all’ strategy may not be applicable to real-world practice. The prevalent regimens and patterns of perioperative blood glucose control identified in this study can only serve as a guide for clinicians.
Our study revealed that most clinicians preferred to withhold OHGA (82.9%) or insulin (69.8%) and keep the patient fasted prior to surgery. This differs from the recommendations by the Royal College of Anaesthetists and Royal College of Ophthalmologists,(12) which recommend that diabetic patients continue their usual medications with no need to fast before ophthalmic surgery under local anaesthesia. These institutions reported no cases of aspiration during cataract surgery under local anaesthesia. In the context of our study, the standard fasting regimen may have been selected according to local protocols in cataract surgery, during which intravenous sedation is usually administered together with regional anaesthesia. In view of the preoperative fasting, the withholding of diabetic medications serves to mitigate the risks of hypoglycaemia. It is generally recommended that oral agents may be discontinued before surgery.(13) Long-acting sulfonylureas are usually stopped 48–72 hours before surgery, while shorter-acting agents can be withheld the night before or on the day of the surgery. For patients on insulin, the American Academy of Family Physicians recommends frequent monitoring of blood glucose level to facilitate insulin dosage adjustments.(13) In general, long-acting insulin may be stopped 1–2 days before surgery, with the patient on a regimen of intermediate and short-acting insulin to stabilise glucose levels. The use of GKI therapy was found to be uncommon in our survey; one possible reason is the inability to easily titrate glucose and insulin delivery perioperatively.
The majority of our respondents (85.3%) agreed that it is necessary to check blood glucose levels before surgery, while only 34.1% would monitor blood glucose after surgery. Both the United Kingdom’s National Health Service(14) and the Association of Surgeons of Great Britain and Ireland(15) recommend close monitoring of capillary blood glucose on at least a one- to two-hour basis during surgery and in the immediate postoperative period. This may be particularly important when sedation has been administered, as hypoglycaemia may manifest as drowsiness, which can be wrongly attributed to the effects of sedative agents. However, such recommendations may not be applicable in the context of cataract surgery, during which sedation may be minimal or even omitted.
Both the American Diabetes Association and the American Association of Clinical Endocrinologists have recommended an in-hospital intensive care unit glycaemic target of 140–180 mg/dL (7.7–10.0 mmol/L) for general medical care wards and a target of 100–180 mg/dL (5.5–10.0 mmol/L) for surgical wards.(16) This matched our survey results, in which a blood glucose level of 6–10 mmol/L would not prompt respondents to treat the patient or cancel the scheduled surgery. Most of the clinicians surveyed said they would address hypoglycaemia of 2–5 mmol/L, while a blood glucose level of ≥ 17 mmol/L and ≥ 23 mmol/L would prompt them to treat and cancel the surgery, respectively. However, it must be noted that the above values are arbitrarily defined in our study design. Interestingly, most clinicians tend to favour the treat-and-defer approach over cancellation of surgery for the same blood glucose levels, although it appears that the decision to cancel becomes clear-cut at glucose levels ≥ 29 mmol/L. This preference may be due to the respondents’ general awareness of the economic costs and wastage of operating resources associated with cancellation of surgery,(17) for which poor control of diabetes mellitus is an important cause.(18)
The majority of the respondents were more concerned about perioperative hyperglycaemia than intraoperative hypoglycaemia. This could be explained by the increased risk of infection, inflammation and poor wound healing associated with hyperglycaemia, factors that would be of concern to the ophthalmologist. From the anaesthesiologist’s perspective, the risk of hyperglycaemic crises may further complicate perioperative management of the patient, especially as poor baseline glucose control is compounded by a stress response to surgery.
The current study was conducted in only four institutions and, hence, may be limited by the small sample size. Management protocols and guidelines may also vary between institutions in view of differences in staff profile, experience and surgical workload; however, there is limited value in elucidating these differences in the present study. Of note, close to half of the respondents were doctors in training (i.e. medical officers and others). However, this did not skew the survey responses, as the prevalent mode of practice in Singapore mandates supervision of junior doctors by a specialist ophthalmologist or anaesthesiologist.
In conclusion, the current study has presented the prevalent practice patterns of ophthalmologists and anaesthesiologists in the perioperative management of diabetic patients undergoing cataract surgery in four health institutions in Singapore. It is clear that further research in this field is required and may be useful for the formulation of formal guidelines and protocols in the future.


