Abstract
INTRODUCTION
Paediatric epidurals can present technical challenges due to wide variations in age and weight among children, ranging from neonates to teenagers. This study evaluated the skin-to-epidural distance in the thoracic and lumbar regions to determine the relationship between age, weight and ethnicity and depth to the epidural space in our Singapore paediatric population.
METHODS
Data from the Acute Pain Service was prospectively collected over 16 years. Details included patient demographics, level of epidural performed and distance from skin to epidural space. Multivariable regression analysis was performed to determine the association of weight, age, ethnicity and gender with the depths to the thoracic and lumbar epidural spaces. A simple linear regression was calculated to predict the depth to both thoracic and lumbar epidural spaces based on body weight. Equations were formulated to describe the relationship between weight and depth of epidural space.
RESULTS
A total of 616 midline epidurals were studied. Regression analysis was performed for 225 thoracic epidurals and 363 lumbar epidurals. Our study revealed a clear correlation between skin-to-lumbar epidural distance and weight in children. The best correlation was demonstrated between skin-to-lumbar epidural distance and body weight (R2 = 0.729). This relationship was described by the formula: depth (mm) = (0.63 × weight [kg]) + 9.2.
CONCLUSION
Skin-to-lumbar epidural distance correlated with weight in children. Our results highlighted the clinical significance of differences between Southeast Asian paediatric populations when compared to other populations.
INTRODUCTION
Paediatric central neuraxial blocks represent a challenge to the anaesthetist, not least because they are commonly performed in the anaesthetised child, thus losing the safety of routine ‘awake placement′ employed in adults. With its lower safety track record, when compared to peripheral regional blocks,(1) it has seen a diminishing trend in its popularity, but nevertheless remains an invaluable tool for optimising perioperative pain relief.
The wide variation in age, weight, size and body characteristics of a cohort comprising neonates to teenagers has implications for accurate placement as well as precise prescription in order to ensure safety and efficacy. Problem-free execution, particularly in neonates and infants, requires both experience and skill, and an awareness of the variability of depth to epidural space.
Previous studies have attempted to determine the relationship between age and weight and the skin-to-epidural distance in children.(2-4) Though the skin-to-epidural distance has been investigated in the Caucasian, South African and East Asian populations,(2-6) to the best of our knowledge, it has not previously been investigated in a multiracial Southeast Asian population.
This study aimed to document and evaluate the skin-to-epidural distance in both the thoracic and lumbar regions in order to determine the relationship between age, weight, ethnicity and gender and depth to the epidural space in our Singapore paediatric population. In addition, we aimed to propose formulae relevant to estimating depth to the epidural space based on our practice.
METHODS
Since 1997, the Department of Paediatric Anaesthesia, KK Women′s and Children′s Hospital, Singapore, has prospectively collected data on every epidural performed and documented the information on Acute Pain Service forms. Data captured comprised specialist′s grade (experience), number of attempts, patient demographics, level of epidural performed, skin-to-epidural distance as well as any complications or problems encountered. In all cases, the procedure was performed in the lateral position and the epidural space was identified by a loss of resistance to saline.
After institutional review board approval, all children below 21 years of age who had received thoracic and lumbar epidurals from 1 June 1997 to 31 May 2013 were identified. Epidurals that were performed via the paramedian approach were excluded. For the epidurals performed via the midline approach, age and weight of patients, level of epidural performed and skin-to-epidural distance were studied.
Data was analysed using IBM SPSS Statistics version 20 (IBM Corp, Armonk, NY, USA). Analysis was performed separately for thoracic and lumbar epidurals. Furthermore, logistic regression analysis was performed on an age range defined by mean age ± two standard deviations. Multivariable regression analysis was initially performed for independent factors of weight, age, ethnicity and gender. A simple linear regression was subsequently calculated with weight alone to determine the linear association between body weight and the depth of thoracic and lumbar epidurals. Equations for each were obtained.
RESULTS
A total of 645 epidurals were reviewed, of which 616 (95.5%) epidurals were performed via the midline approach (
Table I
Demographics of study population (n = 616).
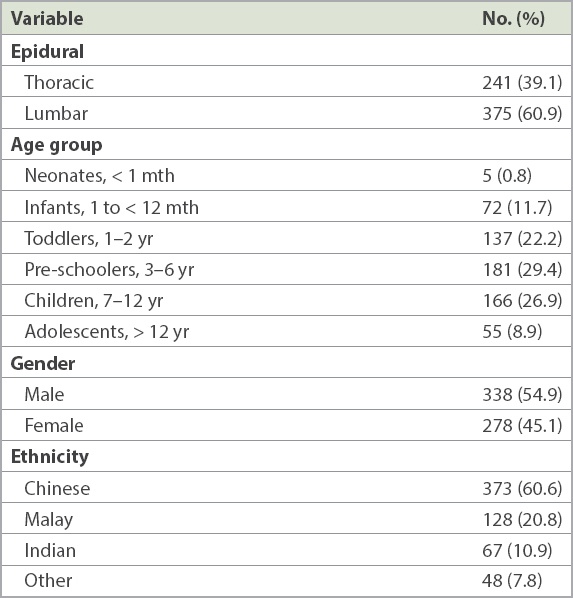
Table II
Study findings according to age group.
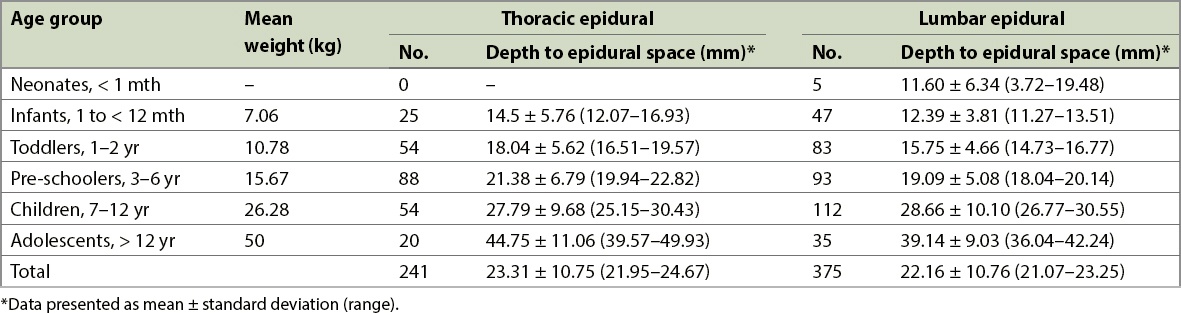
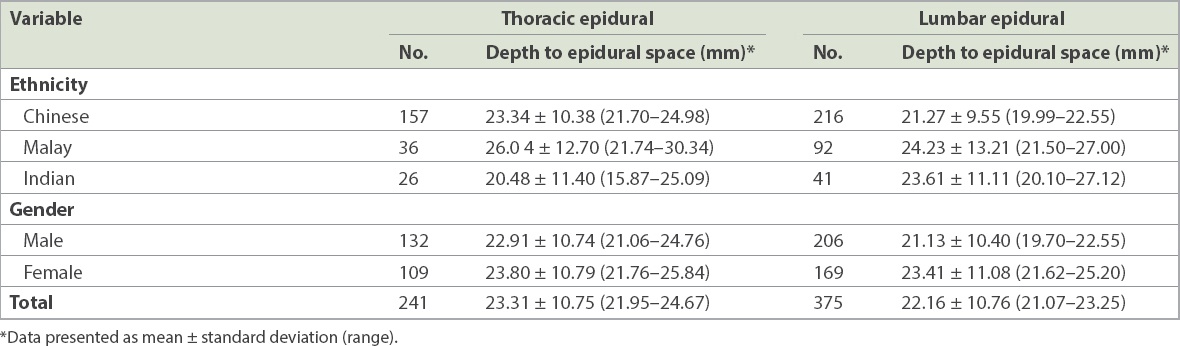
Table III
Study findings according to ethnicity and gender.
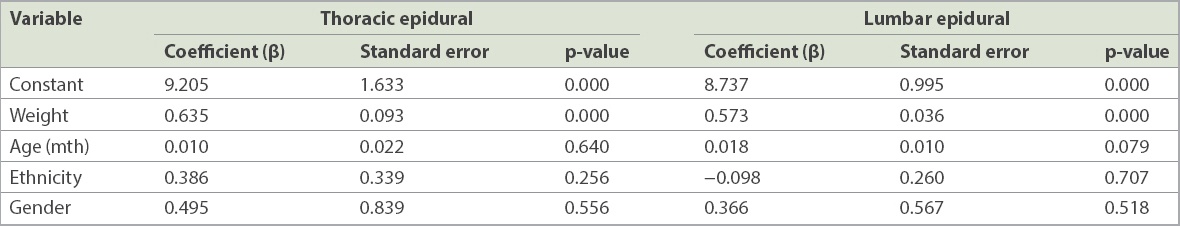
After defining an age range of mean ± two standard deviations, regression analysis was ultimately performed for 225 thoracic epidurals in children aged 0–13 years and 363 lumbar epidurals in children aged 0–14 years. Multivariable regression analysis within the defined age range showed that weight was the only significant predictor for depth to the thoracic and lumbar epidural spaces (
Table IV
Findings of multivariable regression analysis.
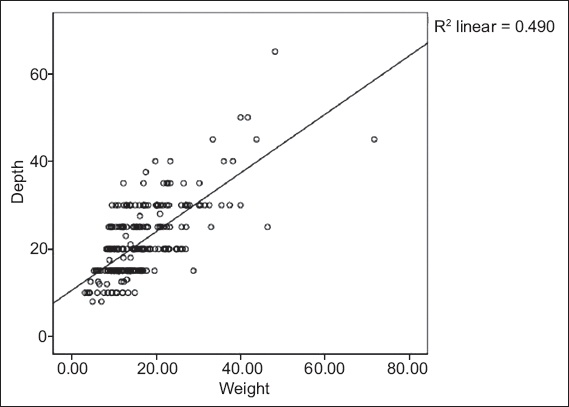
The mean depth of thoracic epidurals was 21.7 (range 8.0–65.0) mm (
Fig. 1
Scatterplot shows the association between weight (kg) and depth of thoracic epidurals (mm) in children aged 0–13 years. The equation for the best fit line is: depth (mm) = 0.67 × weight (kg) + 10.6 (p < 0.01; R2 = 0.490).
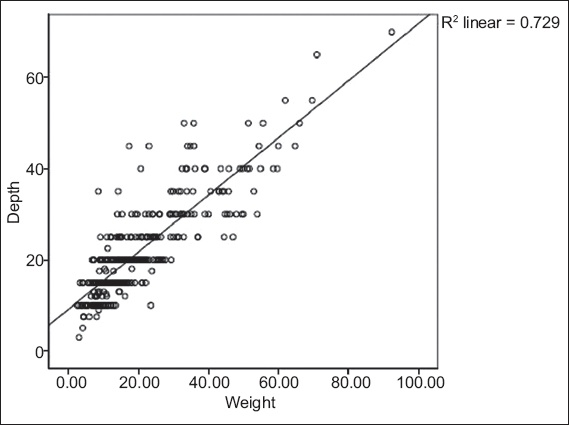
The mean depth of lumbar epidurals was 21.5 (range 3.0–70.0) mm (
Fig. 2
Scatterplot shows the association between weight (kg) and depth of lumbar epidurals (mm) in children aged 0–14 years. The equation for the best fit line is: depth (mm) = 0.63 × weight (kg) + 9.2 (p < 0.01; R2 = 0.729).
DISCUSSION
The skin-to-epidural distance can vary considerably between individuals, depending on a multitude of factors, such as age, weight and body habitus. Anatomical factors, in turn, can be significantly different between populations of different ethnicities. Differences in the depth to epidural space can have profound implications on the patient, particularly in complications related to epidural insertion, such as inadvertent dural punctures and neurological injury.
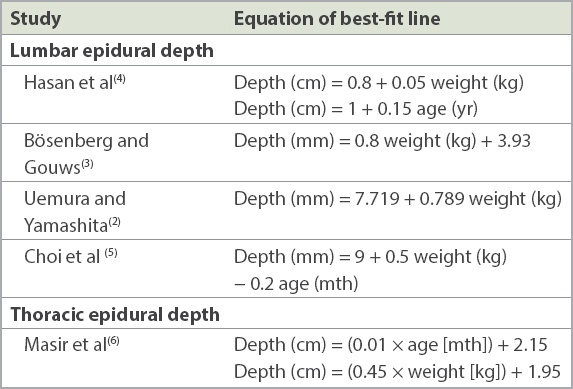
Bösenberg and Gouws showed that a guideline of 1 mm/kg body weight was useful for estimating skin-to-lumbar epidural distance in children aged between six months and ten years.(3) In addition, formulae have previously been derived to estimate the distance from the skin-to-lumbar epidural space based on age and weight in UK(4) and Japanese(2) populations (
Table V
Formulae previously described in the literature for calculation of epidural distances.
Our study revealed a clear correlation between weight and skin-to-epidural distance in children. This correlation has been noted in several studies in the past.(2-4,6) However, significant differences were also found between our population and others previously studied. This may be attributable to population differences.
In our study, the best correlation was demonstrated between the skin-to-lumbar epidural distance and body weight (R2 = 0.729). For any given age, there is a large variation in the body size and characteristics of children, accounting for the decreased correlation of skin-to-epidural distance with age when compared to weight.
This is in keeping with the findings of other studies performed internationally.(2-4) Practically, weight is the most useful predictor of skin-to-epidural distance, as it has the best correlation and is readily available to anaesthetists.
Masir′s formula, depth (cm) = 1.95 + (0.45 × weight [kg]),(6) was derived in a Belgian population and is markedly different from the equation derived by our study. Assuming a 10-kg child, the Belgian equation derives a depth of 2.4 cm compared to a depth of 1.7 cm for Singapore patients – a difference of 7 mm, which has definite clinical implications, including the potential for dural punctures.
In our study, a perpendicular approach was taken in advancing the Tuohy needle in the thoracic intervertebral space. Hence, aside from anatomical differences, it is possible that cephalad angulation of the epidural needle may have accounted for the greater depth to epidural space seen in the Belgian population.
Contrary to the regression equation found for thoracic epidurals, the application of our equation would yield a skin-to-epidural distance deeper than that found in a South African population (
While other studies had previously demonstrated correlation between age and the skin-to-epidural distance,(1,4,5) this association was not found in our analysis. To our knowledge, relationships of gender and ethnicity with skin-to-epidural distance has not previously been investigated or documented in any study. Our study found no relationship between ethnicity or gender and depth to epidural distance. However, this study involved largely Asian ethnicity groups and is unlikely to be representative of a global population.
This study was not without limitations. The study reviewed a total of 616 epidurals performed at a single centre. This represented the largest set of data in the local population. However, over a period of 16 years, these procedures were performed by different anaesthetists within the same department and anaesthetists may have changed their practices with experience. Variations in technique may have given rise to differences in the results studied. Next, it is likely that there may exist other variables affecting depth to epidural space that have not been identified or captured in the proposed formulae. This is particularly so for thoracic epidurals. As such, while the formulae presented by our study may offer some guidance to anaesthetists, it remains important to rely on clinical assessment of the depth of epidural space.
In conclusion, our results highlight the importance of understanding differences between Southeast Asian populations when compared to other populations. Our population was unique in its heterogeneous, multiracial distribution, which may give rise to subtle differences between patients and make our paediatric epidurals more challenging to perform. The differences in the skin-to-epidural distance have clinical significance and implications for complications, such as dural punctures. The application of the derived formulae may increase the success rate and decrease the rate of immediate complications from epidural analgesia.


