CLINICAL PRESENTATION
A 12-year-old boy presented to the Children’s Emergency Department with sudden-onset palpitations that began while he was watching television. He had experienced similar symptoms before, and had been instructed to take his medication as a ‘pill-in-the-pocket’ should they occur. He did not report any chest pain or shortness of breath. His father brought him to the hospital as his symptoms had persisted despite two doses of medications. Clinical examination revealed a well-appearing child with normal heart sounds and a mildly elevated heart rate of 128 beats per minute (bpm). No cardiac murmurs or adventitious lung sounds were heard. His blood pressure and oxygen saturation were within normal limits.
A 12-lead electrocardiogram (ECG) was obtained. What does the ECG (
Fig. 1
12-lead ECG on arrival.
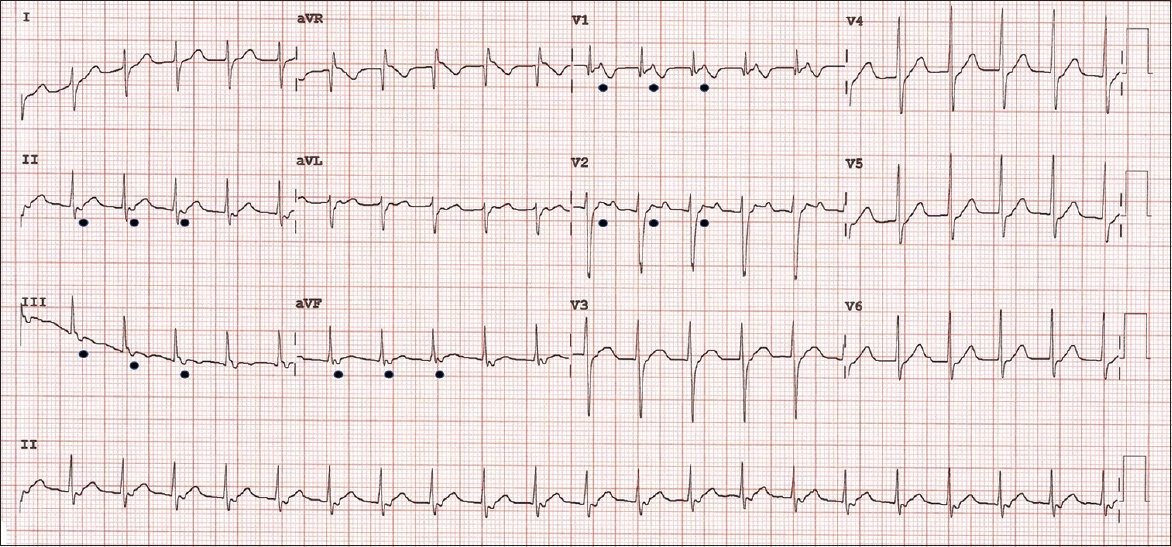
ECG INTERPRETATION
The ECG shows tachycardia at a rate of 128 bpm. P waves are not visualised preceding each QRS complex in this ECG; instead, retrograde P waves are seen in leads V1 and V2, and in leads II, III and aVF (
CLINICAL COURSE
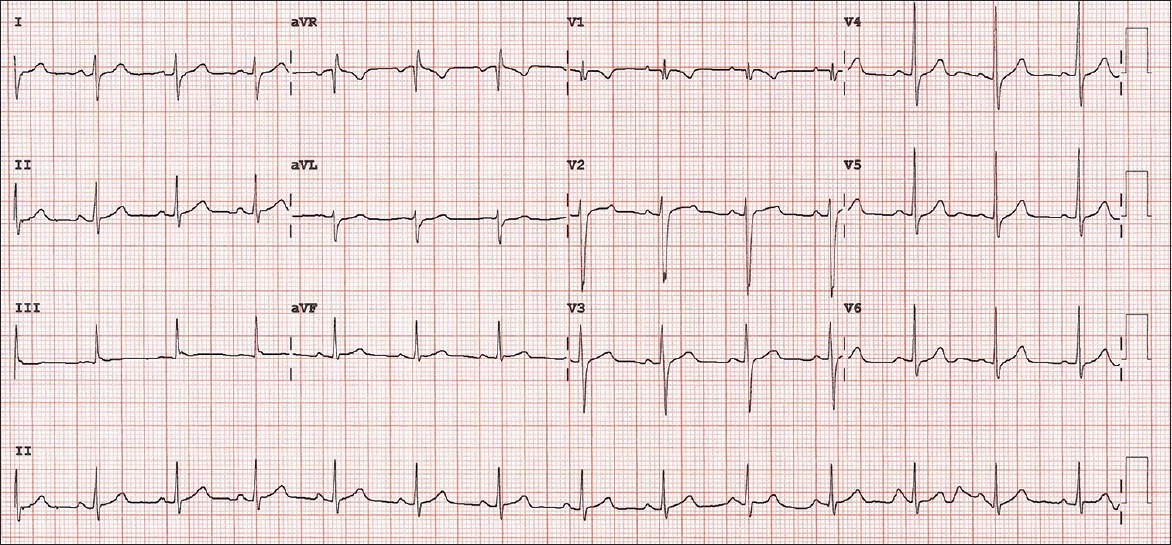
Further questioning revealed that the patient had taken a total of 15 mg of propranolol within two hours prior to presentation. He had a known history of recurrent SVT and was on follow-up at the outpatient cardiology clinic. His last transthoracic echocardiogram showed a structurally and functionally normal heart. He had been advised to take propranolol 10 mg on an ‘as-needed’ basis should initial vagal manoeuvres be unsuccessful. As he was haemodynamically stable at the Children’s Emergency, vagal manoeuvres were re-attempted. After they were unsuccessful, intravenous adenosine of 0.1 mg/kg was administered with a rapid saline flush and the rhythm was converted to sinus rhythm. A repeat ECG was obtained (
Fig. 2
12-lead ECG after first dose of adenosine shows normal sinus rhythm with no evidence of pre-excitation.
He subsequently returned to the Children’s Emergency eight days later owing to another episode of SVT, which required two doses of intravenous adenosine this time, with a second dose at 0.2 mg/kg, for successful rhythm conversion. Following this second presentation, he was discharged with a regular dose of oral atenolol.
DISCUSSION
SVT describes a collection of arrhythmias originating from the atria or atrioventricular node and is the most common arrhythmia in the paediatric population, presenting as a narrow complex regular tachycardia with an extremely rapid ventricular rate (usually 160–300 bpm).(1-3) As per the 2020 Singapore Advanced Paediatric Life Support Guidelines, the heart rate in SVT is usually above 180 bpm in children and above 220 bpm in infants.(4) The child is typically otherwise well, with a structurally normal heart. Children with recurrent SVT are frequently managed with rhythm control agents, either with regular or as-needed dosing.(5,6) In patients who have been pre-treated with beta-blockers, special consideration should be taken during ECG interpretation, as the presenting heart rate may be only mildly elevated and the absence of marked tachycardia may prevent physicians from arriving at the correct diagnosis of SVT. Attention should be paid to the presence or absence of P waves preceding each QRS complex. The clue to the diagnosis of SVT in this case would be the presence of retrograde P waves in leads V1, V2, II, III and aVF. In our approach, we would also look for typical ECG features of specific types of SVT such as the pseudo r’ waves and the pseudo S waves of AVNRT. Another clue would be a fixed monotonous heart rate at presentation.
In re-entrant tachycardia, electrical impulses from activated myocardial regions re-excite areas with recovered excitability and travel around in a re-entrant circuit to cause rapid ventricular depolarisation in an anterograde manner.(1,2) The atria are depolarised in a retrograde manner by the returning electrical impulses, resulting in the appearance of retrograde P waves on the ECG. These are commonly seen as inverted P waves in the inferior leads of II, III and aVF and are usually embedded within or after the QRS complex. Rarely, they may even appear before the QRS complex in atypical forms of re-entrant tachycardia.(2,7) The re-entrant circuit is most commonly established via an anatomical accessory pathway in infants, leading to AVRT, and may manifest features of pre-excitation on ECG (e.g. Wolff-Parkinson-White syndrome).(5) In older children, AVNRT is more common and involves a functionally distinct pathway within the atrioventricular node with varying conduction velocities, creating the re-entrant circuit.(1,2) In AVNRT, retrograde P waves may also be seen, appearing as pseudo r’ waves in leads V1 and V2 and pseudo S waves in leads II, III and aVF. More commonly, P waves may be absent on the ECG strip, as they are hidden within the QRS complex.(1,2) In some situations, as in this case, it may be difficult to differentiate between AVRT and AVNRT on surface ECG, and an electrophysiological study may be required if the episodes of SVT are recurrent. In both cases, the SVT may be aborted pharmacologically with adenosine if vagal manoeuvres fail.
Chronic management of SVT is dependent on the frequency of recurrences and severity of symptoms. The evidence for management of recurrent cases with pharmacological agents is not as robust in the paediatric population compared to the adult population. Beta-blockers are generally recommended as a first-line option for control of recurrent SVT, with instruction to caregivers to monitor for bradycardia and hypotension presenting as dizziness and lethargy.(6,7) Beta-blockers slow the conduction velocity through the atrioventricular node and block impulses from re-circulating while the other re-entrant pathway remains in refractory period.(6) Daily prophylactic therapy is more efficacious than a single-dose ‘as-needed’ regime; however, it suffers from poorer compliance and higher risk of adverse effects.(7) Almost all anti-arrhythmic agents, including calcium channel blockers, digoxin, flecainide, amiodarone and sotalol, have been used in the treatment of SVT, although most have a less favourable side-effect profile and are less commonly used, particularly in the presence of structural heart disease or Wolff-Parkinson-White syndrome.(5,6,8) We recommend that calcium channel blockers be avoided in infants in view of the risk of cardiac decompensation.(9)
Catheter ablation is an effective option to consider as it has high success rates, especially in older children, and is recommended in major treatment guidelines for recurrent SVT. It is, however, avoided in infants below one year of age in view of an increased risk of complications with a higher chance of spontaneous resolution.(5,8,10)
Supplementary Material
SMJ-63-13.pdf


