Dear Sir,
Tracheo-oesophageal fistulae (TOF) occur as a congenital deformity or secondary to pathologic injury from diseases such as carcinoma and are defined as an abnormal connection between the oesophagus and the trachea. Oesophageal malignancy accounts for more than 50% of acquired TOF cases(1) owing to tumour invasion or tumour necrosis after completing radiation and chemotherapy. Benign acquired TOF have rarer aetiologies, such as prolonged intubation, blunt or penetrating trauma, caustic ingestion, local infections (granulomatous mediastinal infections), iatrogenic surgery injury (prior tracheal or oesophageal interventions) and indwelling stents or immunodeficiency.(1) It is crucial to differentiate benign and malignant aetiologies, as their management differs considerably. Management of a malignant TOF is usually palliative in intent owing to its poor prognosis. Stenting is often used to alleviate symptoms and reduce repeated episodes of aspiration pneumonia and sepsis.(2)
We herein report on the case of an 80-year-old Chinese man who presented with dysphagia, odynophagia, cough and left lower zone pneumonia on chest radiography. The patient underwent radiological investigations including videofluoroscopy (
Fig. 1
Videofluoroscopy images show the (a) pharyngeal phase; (b) oesophageal phase; and (c & d) possible tract (arrow) connecting the oesophagus and the trachea.
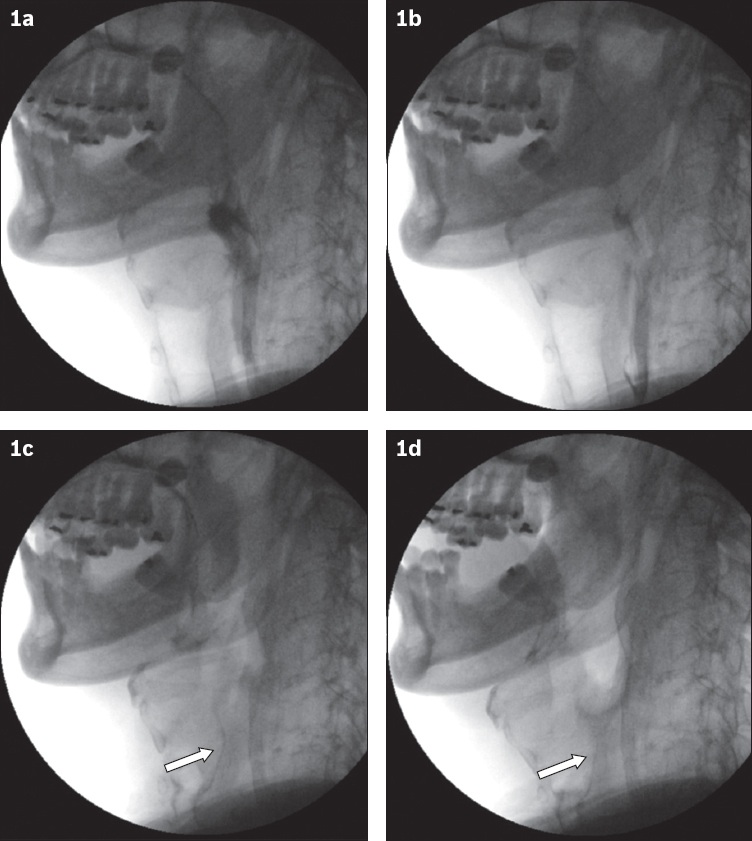
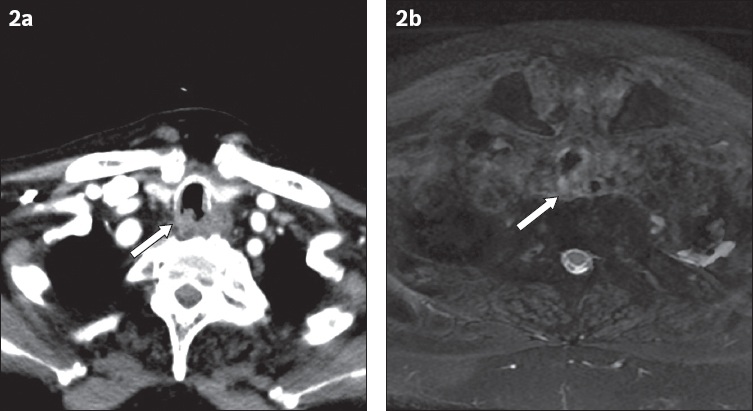
Fig. 2
(a) CT image shows an irregular soft tissue thickening (arrow) of the posterior tracheal wall. (b) MR image of the neck in concordance with the CT image shows tracheal wall thickening (arrow).
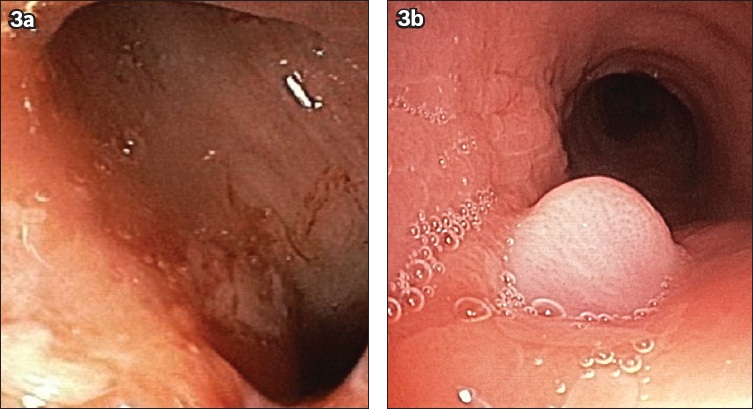
Flexible bronchoscopy and oesophagogastroduodenoscopy showed a tracheo-oesophageal fistula in the proximal trachea, with a sub-centimetre oesophageal defect and grossly normal surrounding mucosa (
Fig. 3
(a) Oesophagogastroduodenoscopy image shows oesophageal opening to the tracheoesophageal fistula. (b) Bronchoscopy image shows an outpouching of the oesophageal mucosa into the trachea.
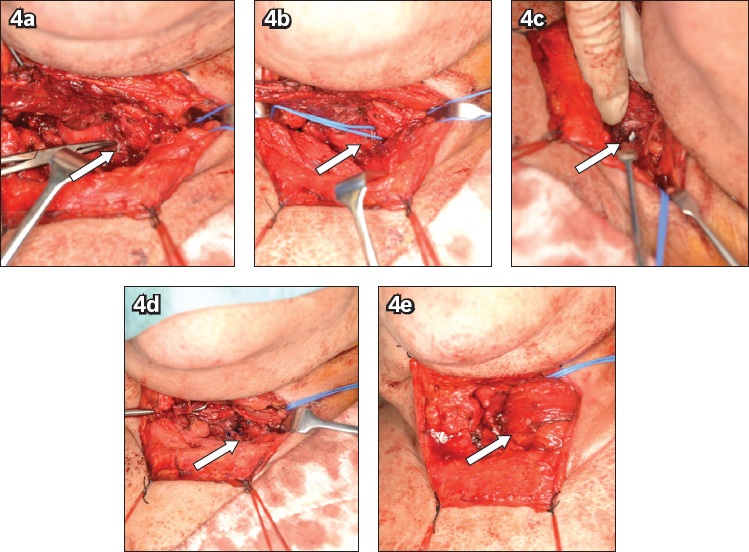
Subsequently, the patient underwent surgical repair of the TOF and a left-pedicled pectoralis major muscle flap reconstruction with buttressing of the tracheo-oesophageal repair. He was positioned supine with the neck hyperextended and intubated using a flexible bronchoscope; the endotracheal tube cuff rested below the fistula and just above the carina. Endoscopy was used to identify the tracheal and oesophageal defects, which were marked with a hypodermic needle for accurate localisation of the fistula. The fistula was ligated, and primary closure of the tracheal defect and oesophageal defect was performed (
Fig. 4
Photographs show the (a) recurrent laryngeal nerve and tracheo-oesophageal fistula (TOF) visualised (arrow); (b) TOF (arrow) isolated and slung; (c) TOF disconnected, visualising the endotracheal tube beneath (arrow); (d) trachea and the oesophagus repaired primarily with interrupted PDS sutures and continuous vicryl sutures (arrow), respectively; and (e) interposition of the pectoralis major flap (arrow) between the trachea and the oesophagus.
The diagnosis of TOF is challenging and requires a high index of suspicion. In the current case, only videofluoroscopy demonstrated the TOF, while other imaging studies did not reveal it. This patient did not have a history of previous intubations, or oesophageal or tracheal instrumentation. Extensive investigations did not show malignancy or infective causes. We postulate that this patient’s TOF might be secondary to trauma from a fishbone perforation in view of its position in the cervical oesophagus at the level of the cricopharyngeus.(3)
Surgical management of patients with acquired non-malignant fistulae between the airway and the oesophagus is challenging. Single-stage direct suture repair of both the tracheal and the oesophageal defect with interposed soft tissue flaps can be performed successfully in the majority of patients with acquired non-malignant TOF.(4,5)


