Abstract
INTRODUCTION
The pattern of venous reflux in Thai patients with chronic venous insufficiency (CVI) was studied in correlation with clinical manifestations.
METHODS
Ultrasonography findings and clinical data were prospectively collected and retrospectively reviewed.
RESULTS
CVI was found in 104 legs of 79 patients (mean age 59.8 ± 12.5 years; C4: 24.1%, C5: 8.9%, C6: 67.1%). 6.7% of the legs had a history of deep vein thrombosis (DVT). The prevalence of superficial vein reflux (SVR), deep vein reflux (DVR), and combined SVR and DVR in 90 legs without previous venous surgery was 82.2%, 63.3% and 57.8%, respectively. In legs with SVR, the prevalence of great saphenous vein reflux (GSVR), small saphenous vein reflux (SSVR), and combined GSVR and SSVR was 91.9%, 33.8% and 25.7%, respectively. 77.0% of SVR involved the calf segment. For medial ulceration, 79.6% had GSVR and 35.2% had SSVR. For lateral ulceration, 46.7% had SSVR and 33.3% had isolated GSVR. Pulsatile venous signal was found in 3.3% of legs. In 17 legs with ulceration after previous surgical treatment, calf vein reflux (residual calf great saphenous vein or small saphenous vein) was found in 13 (76.5%) legs.
CONCLUSION
Calf vein reflux plays an important role in CVI and in patients with recurrent ulceration after previous superficial venous surgery. Although GSVR was present in most patients with CVI in the legs, SSVR may present in one-third of patients, especially those with lateral ulceration. The high prevalence of DVR in the absence of DVT and the presence of a pulsatile venous signal in some patients highlight the incomplete understanding of CVI aetiology.
INTRODUCTION
Chronic venous insufficiency (CVI) is an advanced form of chronic venous disease characterised by skin pigmentation, eczema, atrophie blanche, dermal sclerosis and venous ulceration. Previous studies on the Asian subpopulation from Western countries(1-4) and our own limited earlier study(5) suggest that the characteristics of CVI in Asian patients may differ from those found in the West. The present study aimed to analyse the pattern of venous reflux, as evaluated by ultrasonography, in Thai patients with CVI, correlating findings with clinical manifestations and recurrences.
METHODS
Data of patients with CVI (i.e. Comprehensive Classification System for Chronic Venous Disorders, clinical severity [C] 4–6) who attended the vascular clinic at Vajira Hospital, Bangkok, Thailand, from 1 October 2006 to 30 September 2013 was prospectively collected and retrospectively reviewed. For patients with bilateral CVI, clinical severity was classified according to the higher-scoring leg. All patients underwent history-taking and physical examination according to standard protocols.
All ultrasonography examinations were performed by a vascular surgeon. Patients were placed in the upright position while supporting their weight on the contralateral leg. Venous reflux was elicited by distal manual compression and rapid release. Reflux time of more than 500 milliseconds was defined as venous reflux. The examined venous segments included the proximal and distal common femoral vein, proximal and distal femoral vein, proximal and distal popliteal vein, and saphenofemoral junction, mid-thigh, knee and mid-leg great saphenous veins (GSVs) as well as the small-saphenopopliteal junction and mid-leg small saphenous veins (SSVs). For deep veins, axial reflux was defined as reflux in more than three of six segments examined. For GSVs, axial reflux was defined as reflux in the combined thigh and calf segments of GSVs. Arterial pulsatile signals were defined as high-frequency pulsatile waveforms in the veins consistent with the cardiac cycle during a graphic Doppler examination.
The study was approved by the ethics committee at Faculty of Medicine Vajira Hospital and the project was funded by the Faculty of Medicine Vajira Hospital Research Committee. Descriptive statistics were used and p < 0.05 was considered to be statistically significant.
RESULTS
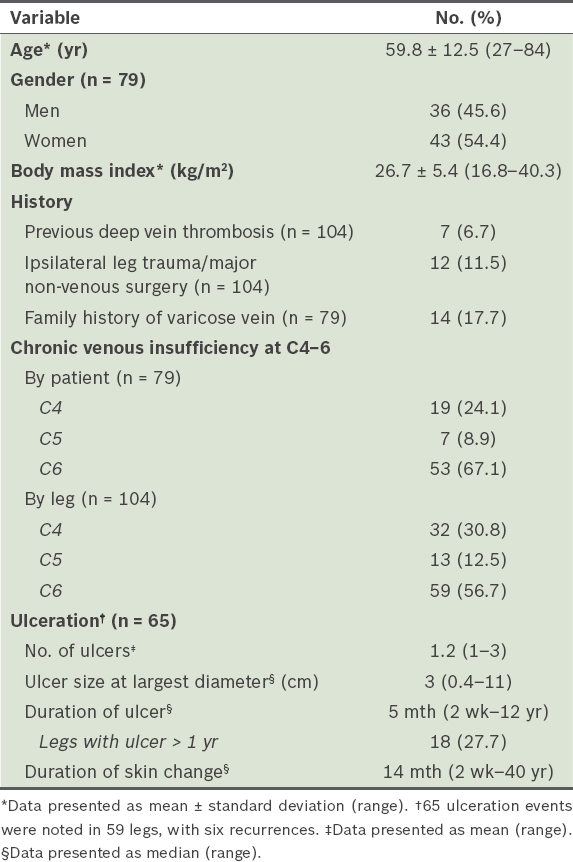
Among 79 patients who completed the examination, there were 104 legs with CVI (C4–6). Patients’ demographic data is presented in
Table I
Demographics of 79 patients with chronic venous insufficiency in 104 legs.
Among 104 legs with CVI, 90 legs of 71 patients had no previous surgery related to the venous system. The ultrasonography findings of these intact legs are presented in
Table II
Ultrasonography findings for 90 intact legs of 71 patients with chronic venous insufficiency who had no previous venous surgery.
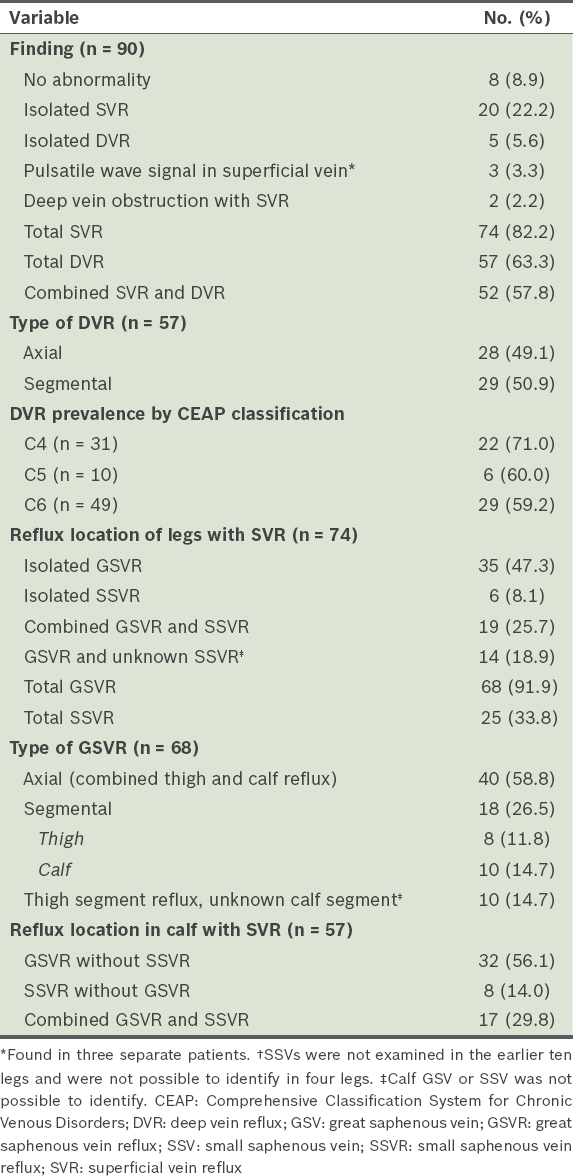
Among 74 legs with SVR, 91.9% (n = 68) had great saphenous vein reflux (GSVR) and 33.8% (n = 25) had small saphenous vein reflux (SSVR), while 25.7% (n = 19) of legs had combined GSVR and SSVR. Among 68 legs with GSVR, 58.8% (n = 40) had axial (combined thigh and calf GSVR) reflux and 26.5% (n = 18) had segmental reflux. Among the 74 legs with SVR, 77.0% (n = 57) had superficial reflux involving the calf venous segment, of which 56.1% (n = 32) had calf GSVR without SSVR, 14.0% (n = 8) had SSVR without calf GSVR, and 29.8% (n = 17) had combined calf GSVR and SSVR. In legs with GSVR, thigh GSVR without calf GSVR was present in 11.8% (n = 8).
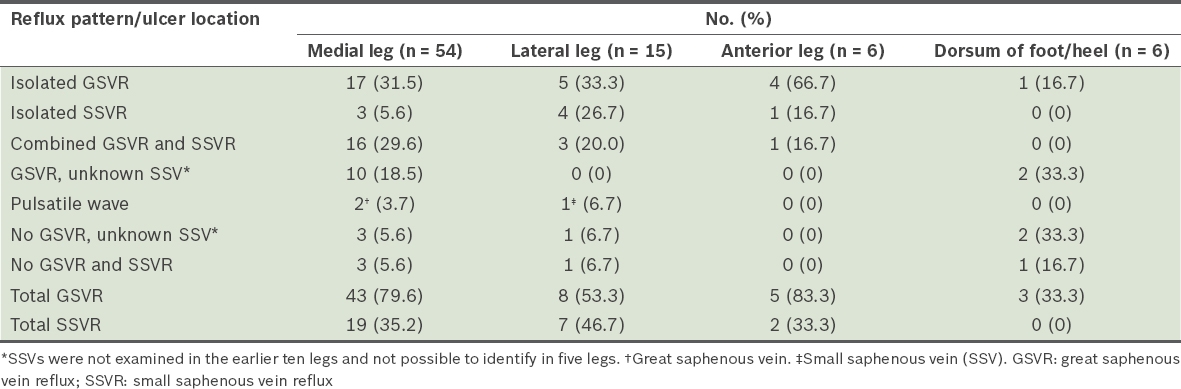
Among the 59 C6 legs, six had recurrences during the data-gathering period, totalling a sum of 65 ulceration events with 81 ulcers. The most common ulcer location was the medial aspect of the leg or ankle. Among the 54 (66.7%) medial ulcers, GSVR was found in 43 (79.6%) ulcers and SSVR was present in 19 (35.2%) ulcers. Among the 15 (18.5%) lateral ulcers, SSVR was found in 7 (46.7%) ulcers and isolated GSVR was present in 5 (33.3%) ulcers. Other locations included the anterior leg (n = 6) and dorsum of the foot or heel (n = 6). The relationship between the location of the ulcers and superficial venous reflux is summarised in
Table III
Relationship between location of ulcer and superficial venous reflux in 81 ulcers.
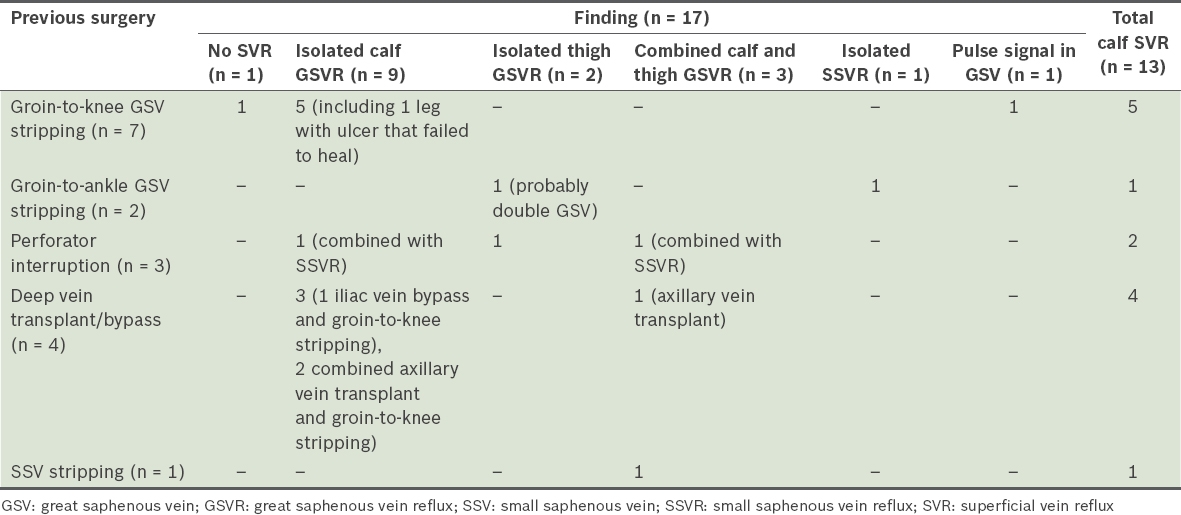
17 legs of 15 patients had non-healed (n = 1) or recurrent (n = 16) ulceration after previous venous surgery for the treatment of CVI. Among the 16 recurrences, the most common operation was groin-to-knee GSV stripping (n = 10, 62.5%), either alone (n = 7, 43.8%) or in combination with axial vein valve transplantation (n = 2, 12.5%) and venous bypass (n = 1, 6.3%). Three legs had perforator interruption, two legs had groin-to-ankle GSV stripping, one leg had axillary vein valve transplantation and one leg had SSV stripping. Calf SVR (calf GSVR or SSVR, or combined) was found in 13 (76.5%) out of 17 legs (
Table IV
Ultrasonography findings for 17 legs of 15 patients with previous venous surgery who presented with non-healed (n = 1) or recurrent (n = 16) ulcers.
DISCUSSION
This study shows a high prevalence of SVR in Thai patients (more than 80%). Many other Asian studies had similar observations, such as those from Hong Kong (93%)(6) and Japan (90%).(7) The history of deep vein thrombosis (DVT) among our patients with CVI was unusual, at 6.7%. Paradoxically, the prevalence of DVR in our study was relatively high (63.3%) and consistent with reports from Hong Kong (73.3%)(6) and Japan (51.7%).(7) Ting et al made similar observations in a review of CVI among Asian patients from Hong Kong.(8) Meanwhile, a study from San Diego, California, United States, found the prevalence of history of DVT to be 2% and DVR in the range of 70%–80% among its Asian subpopulation.(1) The nature and cause of DVR is unknown and probably multi-origin. It has been postulated that DVR may be secondary to SVR volume load, and this is supported by studies that have reported that DVR resolves with superficial vein surgery.(9,10) However, SVR alone is unlikely to be the only cause of DVR; in our study, DVR presented with prior SVR eradication in many patients.
In patients with GSVR, the most common pattern was axial (combined thigh and calf GSVR) reflux, which was present in 58.8% of legs, while a small proportion of legs had reflux confined exclusively to the thigh segment (11.8%). A majority (77.0%) of SVR was located in the calf segment, which could have been associated with the main GSV, its tributary or SSV. This suggests that venous reflux located in the calf adjacent to the ulceration or skin change has a role in the pathogenesis of CVI and should be targeted for removal during CVI treatment. Failure to identify this may result in non-healing of ulcers or their recurrence, given that calf GSV or SSV reflux was the most common finding among patients with recurrent or non-healed ulcerations in our study.
Medially located ulcers were generally associated with GSVR (79.6%). However, SSVR was present in approximately one-third (35.2%) of the medial ulcers and isolated SSVR presented in 5.6% of them. For laterally located ulcers, 46.7% and 33.3% of ulcers were associated with SSVR and isolated GSVR, respectively. Our overall proportions of SVR and of SVR in laterally located ulcers were similar to those of other studies.(7,11,12) This underscores the significance of SSV in the pathogenesis of CVI as well as the indispensability of ultrasonography as a diagnostic tool, given that the location of SVR cannot otherwise be determined based merely on ulcer location or physical findings.
The most widely accepted theory of the causes of venous ulcer is high venous pressure-induced inflammatory response and ulceration;(13-15) a notable cause is venous valve incompetence or obstruction. However, the exact nature of CVI is not completely understood.(13,15) We encountered three patients with venous ulcers who had arterial pulsation waves in the veins. When arteriovenous pathology was investigated using radionucleotide venous scan and angiography, periulcer soft-tissue hypervascularisation was found (
Fig. 1
Angiograph shows periulcer soft-tissue hypervascularisation.

In conclusion, our study indicates the importance of periulcer SVR – either calf GSV and its tributary, or SSV – in Asian patients with CVI. Ultrasonography findings of recurrent or non-healed leg ulcers suggested that surgical treatment should be targeted at these veins. Although GSVR was present in a majority of patients, SSVR was also found to coexist or be present in isolation in a significant number of patients, especially among those with ulcers in a lateral location. Variations in reflux location underscore the importance of ultrasonography. The unknown cause of DVR, which coexists with SVR in a majority of patients with CVI, the absence of abnormal ultrasonography findings and the presence of a pulsatile venous signal in some patients highlight the fact that the aetiology of CVI is not completely understood and may vary among patients of different ethnic groups.


