Dear Sir,
May-Thurner syndrome (MTS) is described as venous outflow obstruction resulting from an anatomical variant in which the left common iliac vein is compressed by the right common iliac artery at the point of crossing over. Patients typically present with leg swelling and oedema or acute deep vein thrombosis at first presentation, with a smaller proportion presenting with pulmonary embolism.(1) We herein report an unusual presentation of MTS in which the patient presented with chronic pelvic pain and bilateral intermittent lower limb swelling.
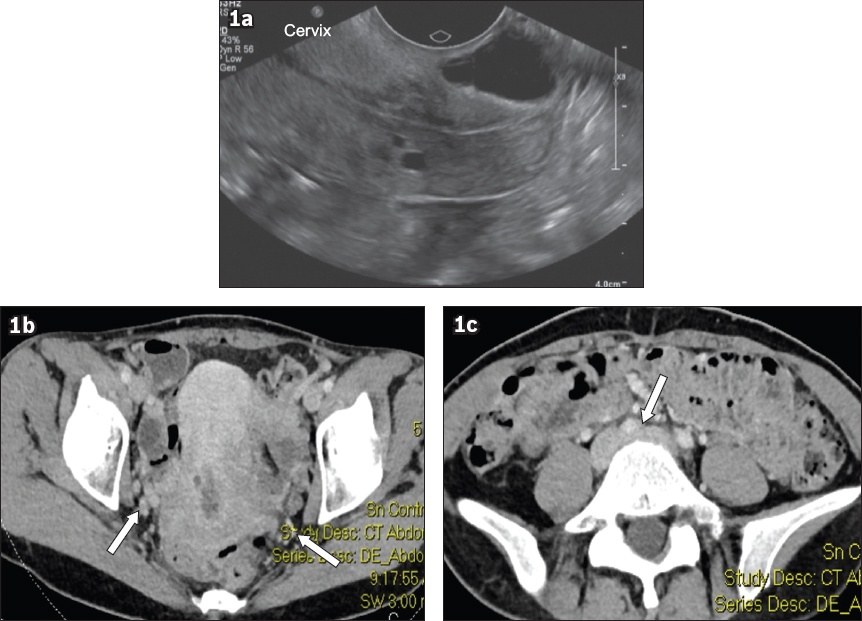
A 49-year-old woman with a known history of rheumatoid arthritis and previous ectopic pregnancy presented to the vascular specialist clinic with a six-month history of lower back and pelvic pain. The pain was aching, non-radiating and episodic in nature, with each episode lasting between hours and days. It was associated with intermittent bilateral lower limb swelling that worsened with prolonged standing and sitting, and was relieved by lying flat. The patient also reported 4 kg of unintentional weight loss and less frequent bowel movements over the same time period. She denied having any lower limb weakness, numbness, urinary symptoms, deep dyspareunia or history of preceding back trauma. Physical examination was unremarkable. Her current medications included hormonal therapy for perimenopausal symptoms. Magnetic resonance imaging of the sacrum demonstrated dilated veins in the right pre-sacral space arising from the right internal iliac vein, suggestive of pelvic congestion syndrome. Pelvic ultrasonography found no cervical lesions except for venous congestion (
Fig. 1
Pelvic US image shows (a) enlarged oedematous cervix with cysts. CT images show (b) bilateral dilated adnexal veins (arrows) and enlarged cervix and (c) compression of the left common iliac vein by the right common iliac artery (arrow).
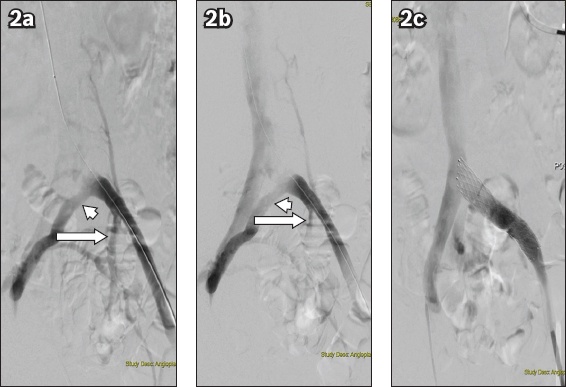
Intraoperatively, left antegrade iliac venography demonstrated a tight stenosis in the proximal left common iliac vein, with a large pre-stenotic collateral and reflux into the left internal iliac vein, in keeping with MTS (Figs.
Fig. 2
Iliac venograms show (a & b) severe left proximal common iliac vein stenosis with large pre-stenotic collateral (arrowheads) draining into the right iliac vein, with reflux into the left internal iliac veins (arrows), and (c) left common iliac vein stent with good flow. No residual stenosis or collaterals are visualised.
Atypical presentations of MTS that have been reported in the literature include severe pelvic pain with absence of lower extremity symptoms(2) and left-sided varicocele.(3) In this case, our patient presented with chronic pelvic pain, bilateral lower limb swelling and systemic symptoms such as change in bowel habits and weight loss. The pelvic pain occurred as a result of pelvic congestion due to downstream obstruction. We suspect that the bilateral lower limb swelling was due to back pressure from cross collaterisation from the left side and diversion of venous drainage to the right. This is supported by the fact that the swelling of the right lower limb also settled after the left common iliac vein stenting. The change in bowel habits and weight loss could have resulted from the abdominal discomfort and bloating. This case illustrates that presenting symptoms of MTS can vary and can sometimes be misleading. MTS is usually suspected based on the clinical presentation of left lower limb pain or swelling with concomitant findings of deep vein thrombosis in the affected lower extremity on duplex ultrasonography. The diagnosis can then be further augmented by non-invasive or invasive modalities such as CT venography, magnetic resonance venography and intravascular ultrasonography (IVUS). CT venography is most commonly used preoperatively to look for iliac vein compression and to rule out any large intra-abdominal masses that are causing extrinsic venous compression. However, it may exaggerate the extent of compression of the iliac vein in a dehydrated patient; the absence of iliac vein compression on CTs does not rule out compression, as the process is dynamic and CT only captures one time point and cannot visualise scarring within the vein. The gold standard for diagnosing MTS is conventional venography with IVUS. The benefits of IVUS include accurate evaluation of the wall of the vessel lumen and its diameter, which is paramount for stent selection and accurate stent placement.
In summary, a diagnosis of MTS should be considered in patients presenting with chronic pelvic pain, as MTS can be proven by on-table interrogation of the common iliac vein and treated by stenting, resulting in significant symptomatic improvement. Unfortunately, knowledge of deep vein pathology and what can be offered to patients for symptomatic venous obstruction, such as in severe chronic venous insufficiency (venous ulcers and leg swelling), remains primitive and immature. As a result, patients tend to be put in compression for an unnecessarily long period of time before presentation. Conventional venography with IVUS remains the gold standard for diagnosing MTS. This case report lends support to the current sparse case reports available in the literature on atypical presentations of MTS.


