Abstract
Intra-articular ganglion cysts of the anterior cruciate ligament (ACL) are rare, and bilateral ganglion cysts are even rarer. These cysts may cause intermittent or chronic nonspecific knee discomfort. Although three cases of bilateral ganglion cysts have been reported in the literature, the knees were not simultaneously affected in those cases. Herein, we report the case of a 56-year-old woman who presented with simultaneous bilateral ganglion cysts of the ACL that were symptomatic. She was successfully treated with arthroscopic resection and debridement. We also present a brief review of the literature, highlighting the aetiology, diagnosis and management of ganglion cysts of the ACL. To the best of our knowledge, this is the first report of simultaneous bilateral intra-articular ganglion cysts of the ACL.
INTRODUCTION
Intra-articular ganglion cysts may originate from the cruciate ligaments, menisci, popliteus tendon or alar fold.(1) Anterior cruciate ligament (ACL) ganglion cysts were first described by Caan in 1924.(1,2) Although the widespread use of magnetic resonance (MR) imaging and arthroscopy has resulted in an increased number of reports on ganglion cysts, these published case reports mainly presented cases of intra-articular soft tissue masses; ganglion cysts of the ACL are still rarely reported.(3,4) The overall incidences of ACL ganglion cysts are 0.6%–2.0% in arthroscopic studies and 1.0%–1.3% in MR imaging studies;(1,3-5) symptomatic ganglion cysts account for only about 10% of these cases.(1) In several studies, the incidence of intra-articular ganglion cysts of the knee joint has been reported to be more frequent in males in the fourth or fifth decade of life.(1,5,6)
Herein, we report a rare case of symptomatic bilateral ganglion cysts of the ACL occurring simultaneously. We also review the literature and discuss the aetiology, diagnosis and management of ganglion cysts of the ACL. To the best of our knowledge, this is the first case report on such an occurrence.
CASE REPORT
A 56-year-old woman presented with pain, reduced range of motion and mild swelling in both knees. She reported no locking or instability, and no history of recent trauma or sports activity. She had no relevant past medical history and no history of morning stiffness or other joint involvement. The patient was working as a manager in an office setting and had a sedentary lifestyle. Evaluation for rheumatologic disease was negative and blood assessment was unremarkable. Right knee complaints had been ongoing for a year, while reduced flexion range was exacerbated for about seven months. The pain in her left knee had been ongoing for at least six months, while loss of flexion increased in the past month.
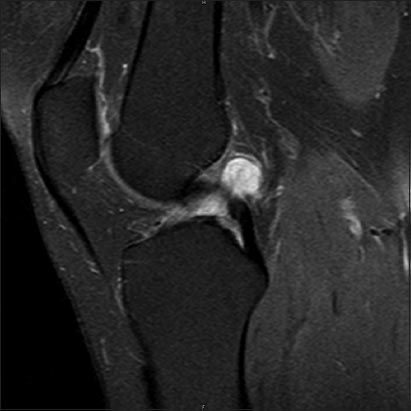
Physical examination of her right knee revealed mild effusion with no locking. Anterior and posterior drawer tests, Lachman test, and varus and valgus stress tests demonstrated no instability. There was no tenderness or swelling along the joint lines. The right knee had a flexion of 90° with pain and full extension. MR imaging of the right knee demonstrated a 21 mm × 13 mm well-circumscribed cystic structure, with low signal intensity in T1-weighted images and high signal intensity in T2-weighted images. The lesion was found next to the femoral attachment of the ACL (
Fig. 1
Sagittal T2-W MR image shows a high signal intensity ganglion cyst located posterior to the anterior cruciate ligament.
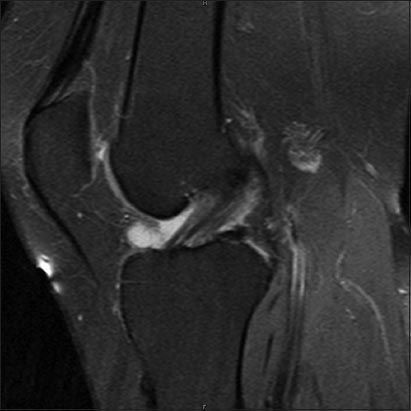
There was also mild effusion in the left knee with no locking. Anterior and posterior drawer tests, Lachman test, and varus and valgus stress tests likewise demonstrated no instability. As was the case with the right knee, there was no tenderness or swelling along the joint lines. The left knee had a flexion of 105° and full extension, with pain experienced in forced extension. MR imaging demonstrated an 11 mm × 6 mm well-circumscribed cystic lesion anterior to the tibial insertion of the ACL. The lesion was homogenous, with low signal intensity in T1-weighted images and high signal intensity in T2-weighted images (
Fig. 2
Sagittal T2-W MR image shows a high signal intensity ganglion cyst located anterior to the tibial insertion point of the anterior cruciate ligament.
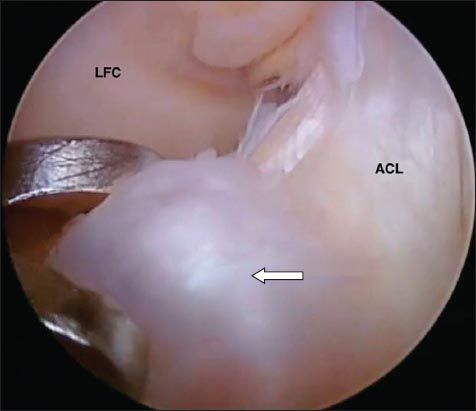
Arthroscopy was performed on both knees using a standard two-portal anterolateral and anteromedial technique. A cystic mass lying between the proximal end of the ACL and the posterior cruciate ligament (PCL) in the right knee was identified (
Fig. 3
Arthroscopic image of the right knee in flexion shows the cyst (arrow) located behind the anterior cruciate ligament (ACL). MFC: medial femoral condyle
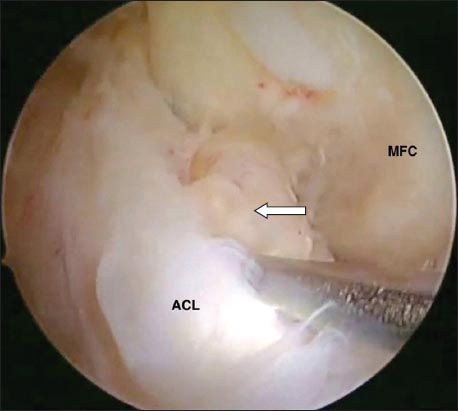
Fig. 4
Arthroscopic image of the left knee in flexion shows the cyst (arrow) next to the tibial insertion of the anterior cruciate ligament (ACL). LFC: lateral femoral condyle
Thorough inspection and probing of the joints revealed no other accompanying pathology. The integrity of the cruciate ligaments was confirmed via examination with a probe. Histological examination of the tissue samples from both knees revealed synovial cells consistent with ganglia. After the operation, the patient was allowed to weight-bear as tolerated; she did not require bracing. A home exercise programme for quadriceps femoris setting and hamstring strengthening was prescribed. At follow-up four months after the operation, the patient was symptom-free.
DISCUSSION
Ganglion cysts of the ACL are very rarely seen and only 10% of patients have symptoms.(1) The aetiology of isolated ganglion cysts of the ACL remains unknown, although there have been several postulated theories. Some authors have suggested that they arise due to synovial tissue herniation, connective tissue degeneration after trauma, mucin deterioration of connective tissue, ectopia of synovial tissue and proliferation of pluripotent mesenchymal stem cells.(1,5)
Intra-articular ganglion cysts may be symptomatic, causing chronic or intermittent knee discomfort and limited knee movement.(1,6) Depending on their intra-articular location and size, ganglion cysts may be responsible for mechanical blocking symptoms, limitation of motion, and discomfort in flexion and extension. Cysts that are located anterior to the cruciate ligament are more likely to restrict extension, while cysts that are located posterior to the cruciate ligament tend to limit flexion.(1) These cysts do not present with a clear inciting event and a majority of them occur without concomitant intra-articular lesions. Asymptomatic intra-articular knee ganglions may be detected incidentally, usually during assessment for other intra-articular pathologies.(1,3)
In the present case, the patient had chronic pain and reduced range of movement in both knees without a traumatic event. Flexion was limited in both knees. Her left knee, which had a smaller ganglion cyst anterior to the ACL, was painful in forced extension. MR imaging and arthroscopy did not detect any other concomitant intra-articular lesions in both of the patient’s knees. MR imaging is the most sensitive and specific noninvasive method for diagnosing ganglion cysts of the ACL and other intra-articular pathologies.(3) Ganglion cysts are usually ovoid, well-circumscribed and have homogeneous low signal intensity on T1-weighted images; however, on T2-weighted images, these cysts show high signal intensity.(1,5) The MR images obtained from the present patient had similar characteristics and did not reveal any accompanying lesions. The differential diagnoses for ganglion cysts of the ACL include pigmented villonodular synovitis, haemangioma, synovial sarcoma, synovial proliferation, myxoma, fibroma, synovial chondromatosis, meniscal cyst and aneurysm.(7-10) While these disorders usually have characteristic features on MR imaging, a tissue sample for histologic examination would be helpful in confirming any diagnosis made.
Arthroscopic resection is the preferred treatment, as it is associated with a low rate of recurrence.(1,5,11) While arthroscopic aspiration and radiology-guided aspiration have also been used for treatment, these methods are reported to have a higher rate of recurrence.(12,13)
In conclusion, ACL ganglion cysts are an uncommon cause of knee pain, and although rare, these cysts can occur simultaneously in both knees. Bilateral ganglion cysts of the cruciate ligaments have been reported by Noda et al, Willis-Owen et al and Andrikoula et al; however, in these reports, the knees were affected ten years, six years and one year apart, respectively.(11,14,15) To the best of our knowledge, the present case is the first report of symptomatic bilateral intra-articular ganglion cysts of the ACL occurring simultaneously in both knees. The patient was successfully treated with arthroscopic resection and debridement. She recovered to full function at follow-up four months after the operation and was symptom-free.


