Abstract
COVID-19 significantly impacted the teaching-learning-assessment activities in many medical schools. In this article, we discuss the impact of COVID-19 on the Yong Loo Lin School of Medicine, National University of Singapore, focusing on paediatric training and the adaptations of the system and the people. The school developed strategies to promptly disseminate information and safety measures to protect all its staff and students. By leveraging on the school’s infrastructure for technology-enabled learning, good-quality medical training and reliable assessments were able to be carried out swiftly. The paediatric curriculum was crafted based on these principles, and it provided distance-based learning with live and interactive sessions to teach core clinical skills. The faculty also tapped on standardised patients to provide consistent and life-like scenarios. Measures were implemented to minimise challenges with technology-enabled learning. Collectively, efforts from the staff, support from the leadership and students’ adaptations tremendously helped to ease the transition.
INTRODUCTION
It has been more than a year since COVID-19 was first reported in Wuhan, Hubei Province, China.(1) This contagious viral illness has spread wildly within a short period of time, affecting many countries. As of 28 March 2021, there have been 126,359,540 confirmed cases of COVID-19 and 2,769,473 deaths reported to the World Health Organization (WHO).(2) Within a few weeks of identifying the first COVID-19 case in Singapore, the Disease Outbreak Response System Condition (DORSCON) level was raised from Yellow to Orange.(3) This had a major impact on the teaching-learning-assessment activities in the medical school. Student activities in clinical settings had to be limited, and clinical assessment formats had to adopt different platforms. In this article, we discuss the impact of the COVID-19 pandemic on the Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine), with a special focus on paediatric training. In addition, we share how the medical school adapted to this change, the challenges faced and the strategies used to mitigate the effects of the pandemic.
IMPACT OF COVID-19 PANDEMIC ON NUS MEDICINE
The COVID-19 pandemic had led to changes in the following six broad areas of the school.
1. A centralised system of management
The Education Team Contingency Workgroup was set up to develop strategies based on the new policies issued from the school or government bodies. The aim was to ensure business continuity while maintaining the safety of the staff. These strategies and their implementation had to be disseminated to all staff appropriately, accurately, transparently, consistently and in a timely manner.
Prioritising safety for all stakeholders
New measures were put in place to safeguard the school from COVID-19. These measures focused on early detection and reduction of the risk of widespread transmission. All staff and students were expected to take ownership of monitoring their health via documenting their temperatures, reporting to the central administration when ill, taking medical leave when necessary, etc. Split team work arrangements were implemented for the staff. There were restrictions on crossing to other healthcare institutions. NUS Medicine also had to exercise additional measures to achieve a high level of cleanliness so as to prevent the spread of the virus.
Transparency and consistency in information dissemination
Considerable effort was made by NUS Medicine to ensure that information dissemination was prompt, transparent, consistent and accurate. Apart from the strategies mentioned above, the information also included guidelines from government bodies, frequently asked questions and the number of infected cases on campus. One way of disseminating information was through an initiative by the school – the COVID-19 chronicles.(4) The chronicles were short educational cartoon strips, whereby key information on COVID-19 was disseminated to all NUS staff and students.
Leveraging on technology to deliver good-quality training
Prior to the outbreak, NUS Medicine had maintained the necessary infrastructure for technology-enabled teaching. This was particularly valuable when the size of gathering allowed decreased and during the circuit-breaker period, when no one was allowed on campus. We were able to swiftly move large-group non-clinical teaching online. As the COVID-19 restrictions eased, small-group teachings (involving fewer than 50 participants) were held face-to-face, while adhering to strict safety measures and regulations.
As the pandemic spread, clinical rotations were halted in February 2020. This mainly affected the Phase III students, who had completed only three out of their four clinical rotations (Phase IV students were on their elective period, and the final-year Phase V students had completed all their clinical rotations). The Phase III students were given a two-week break so that the faculty could replace the clinical teaching in their final clinical rotation with other forms of teaching. The availability of technology, standardised patients as well as a simulation centre enabled us to create this entirely new curriculum within two weeks. This new curriculum included elements such as pre-recorded online lectures, online live lectures, online live tutorials conducted via Zoom or Microsoft Teams, online live case-based learning, online self-directed learning using programmes such as Aquifer and simulation-based teachings. As COVID-19 improved over time, for the academic year beginning in June 2020, clinical postings were resumed, but only at 50% of their usual duration and with rigorous movement restriction and other safety measures. The other half of the time remained as campus-based learning, as described above.
Maintaining the rigour and quality of assessments and examinations
Conduction of continuous assessments was facilitated by the fact that we had gone online for all our clinical posting assessment forms. This meant that admin staff could work from home as they did not have to collect and process hard copy forms. Use of the online e-assessment forms also meant that we reduced the risk of the hard copy forms being fomites.
Conducting exams during the COVID-19 outbreak was a huge challenge, especially the graduating class’ final MBBS exams in March 2020. The school was committed to conducting this exam, as it had the responsibility of providing 300 new graduates for the healthcare service, which was anticipated to come under duress in the event of a large COVID-19 outbreak. Fortunately for us, all our theory exams were already conducted on an e-exam system for several years. It was not too difficult for us to de-centralise and simultaneously conduct the theory exams at multiple sites, with each hosting up to only 50 persons while maintaining physical distancing, social distancing and many more safety measures.
The final-year clinical exams were held in NUS, as it was a non-clinical institution. Real patients were replaced with standardised patients (SPs), simulators and task trainers. We were able to do this as we had built these resources over the years. Student briefings, examiner briefings and exam team briefings were conducted online. Students, examiners, SPs and the exam team were assembled into small groups with minimal cross movement. Many other safety measures were put in place. The final-year exams were conducted without sacrificing the number of exam stations and without incurring a single COVID-19 infection. It probably did cause the exam team members to grow more white hairs. We did cancel the Phase II and Phase III clinical exams. However, the Phase III clinical exam would be replaced with a formative exam at the end of the Phase IV school term.
Adaptations of the school admission exercise
The 2020 admissions exercise was also affected. Under strict regulations, with no cross-campus movement of healthcare workers during this period of time, the number of assessors to invigilate the admission exercise was adversely affected. Therefore, the number of stations during admission exercise was reduced from five to two to accommodate this change. The admission process also moved online, leveraging on the technology that was available to us.
ADAPTATIONS OF UNDERGRADUATE PAEDIATRIC MEDICAL EDUCATION
The academic year 2020 (starting in June 2020) was meant to be the launch of the new Phase IV paediatric curriculum for NUS Medicine. The paediatric education team of NUS, NUH and KKH had spent many months planning and implementing this new curriculum. With the institution of the 50% reduction in clinical training and no cross-institution movement, all this preparation work was gone with the wind. Over a two-month period, we had to build yet another new curriculum for the paediatric posting in Phase III, Phase IV and Phase V. We had to figure out how to teach about 900 in-flight students while complying with the strict restrictions and lack of clinical patients.
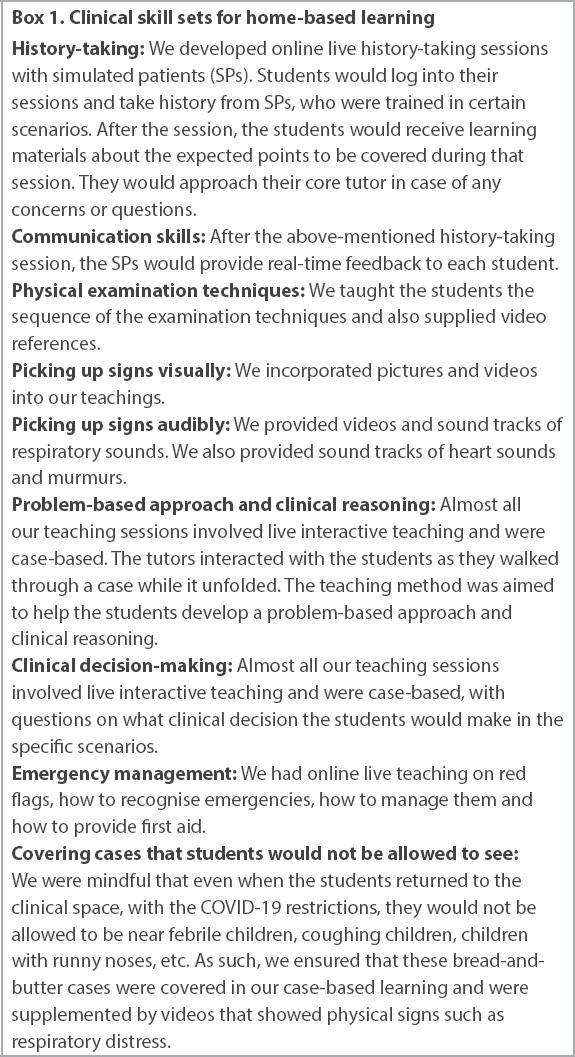
With the clinical exposure halved, we needed to figure out how to use the home-based learning time to make up for the loss of clinical learning. We distilled the clinical skill sets that we thought we could still try to teach while the students were doing home-based learning. This has been summarised in
Box 1
Clinical skill sets for home-based learning
We recognised that home-based learning meant that we could not help the students develop their tactile skills, e.g. experiencing how an enlarged liver feels like. Hence, we emphasised to the students that during their clinical weeks, they had to make all effort to touch and examine patients. We also ensured that they had clinical tutors during their clinical posting. The physical distancing and social distancing measures meant that we could not send the students to the usual places, as it would result in overcrowding. Thus, we used resources that we traditionally did not use for medical students, e.g. patients were seen in the clean areas of the paediatric emergencies.
We also recognised that COVID-19 and the consequent changes to the medical education can add to the academic as well as psychological stress of the students. We were also cognisant that this situation could make the weaker students more vulnerable to failure. Hence, we instituted the role of the core tutor. This is elaborated in the next section.
ADOPTION AND CHALLENGES OF DIGITAL MEDICAL EDUCATION
Responding to the changes in the curriculum and social distancing measures, a new teaching role that utilised distance-based learning (DL) was created. Faculty members were invited to be core tutors and they were to journey alongside the students for the entirety of their paediatric posting (two weeks for Phase III, six weeks for Phase IV and three weeks for Phase V) by meeting with the students every week but via an online platform, usually Zoom or Microsoft Teams. For Phase IV and Phase V, each clinical group was assigned two core tutors. The core tutor was to be a mentor and counsellor for the students in case any of them were facing academic difficulty or psychological stress because of the modified curriculum. The online meetings were also used to assess and cover learning gaps. The meetings tended to be longer when the students were learning from home and shorter during their clinical weeks, and they were sometimes conducted during the students’ lunch hour.
The core tutors found that the consistent contact with the students was useful in obtaining a more holistic view of the students’ strengths and weaknesses. The general feedback from the students on the core tutor sessions was good, and they wished that some sessions could have been face-to-face. They liked the informal nature of the sessions and that they were given the chance to clarify their doubts and ask questions.
DL is a form of technology-enabled learning that has been progressively incorporated into undergraduate medical education over the years.(5,6) However, this pivot towards DL was sudden and huge; it posed some challenges to both tutors and students, as follows. The foundation of DL was dependent on the adoption of digital skills such as online content creation or video conferencing and the provision of technological equipment, including laptops and webcams.(7) Many tutors were required, at short notice, to learn these digital skills, be adept in them and to apply them during their online teaching sessions. Some of the impediments faced were the lack of resources to learn the digital skills or the lack of guidance on how to conduct DL.(8) This was probably more difficult for the senior tutors who conducted only traditional face-to-face teaching or those who were less familiar with digital learning.(9) Fortunately, most doctors were quick learners and could adapt, albeit with a steep learning curve.
A major limitation of DL vis-a-vis face-to-face teaching was the lack of bedside patient interactions.(10) The art of medicine revolves around doctor-patient interactions, and many core skills, such as history-taking and physical examination, require the student to physically interact with the patient. Therefore, DL could not totally replace all critical bedside skills.(11) The downstream impact would likely be the greatest for the Phase III students, as their opportunities to accrue these clinical skills in their first major clinical year were significantly curtailed. To minimise these limitations, many measures were introduced, such as online live history-taking sessions and incorporation of SPs in assessments and exams.
When conducting face-to-face teachings, the tutor often used various sensory modalities to engage with the students, such as body language and intonation. However, not all of these modalities can be created successfully, in partial or in full, during DL sessions, when one is facing a screen. A student might feel socially isolated if there is little or no interaction during DL.(12) With this in mind, the school strongly encouraged online teaching to be interactive. Almost every paediatric home-based learning session was interactive, with questions built into the cases. There were sufficient questions for the tutor to ask at least one question to every student during each session. Owing to the lack of physical presence, tutors also needed to be more aware of the students’ mood by attempting to hear between the lines and read the students’ body language through the screens.(13) It was difficult for tutors to identify a struggling student in a large group teaching. Hence, the core tutor concept was implemented to mitigate this.
CONCLUSIONS
NUS Medicine is much more prepared today than it was during the SARS outbreak. The implementation of technology-based teaching and learning, standardised patients, simulators and task trainers had been in place for several years before COVID-19 struck. This allowed the school to adapt quickly and reduce the impact on student learning during the outbreak. While there were some constraints in the initial implementation of these adaptations, many measures were adopted to minimise the impact and many tutors quickly caught on to technology-enabled learning. We were also very fortunate to have a large database of SPs that the school managed to mobilise quickly to assist in teaching as well as in examinations. Most importantly, the collective effort from the staff, strong support from the leadership and students’ adaptation to the situation tremendously helped to ease the transition.


