Abstract
Most cases of intussusception in adults present with chronic and nonspecifi c symptoms, and can sometimes be challenging to diagnose. We herein report on a patient w ith the rare symptom of colonic intussusceptions presenting with rectal prolapse and review the existing literature of similar case reports to discuss how to reach an accurate diagnosis. A 75-year-old woman with dementia presented with per rectal bleeding, rectal prolapse and lower abdominal pain. An operation was scheduled and a large sigmoid intussusception with a polyp as a leading point was found intraoperatively. She subsequently recovered well and was discharged. As large sigmoid intussusceptions may present as rectal prolapse, intussusception should be considered as a differential diagnosis for immobile patients, especially when the leading point is a lesion.
INTRODUCTION
Symptoms of intussusception in adults are not as typical as those in paediatric cases. Most adult cases present with chronic and nonspecific symptoms such as nausea, vomiting, gastrointestinal bleeding, constipation and abdominal distention.(1) Thus, they can sometimes be challenging to diagnose. We herein present an even rarer presentation of intussusceptions: rectal prolapse. We review the literature of similar case reports in which intussusception presents with rectal prolapse and discuss ways to reach an accurate diagnosis.
CASE REPORT
A 75-year-old Chinese woman was bedridden and uncommunicative due to a previous femoral neck fracture and dementia. She presented with per rectal (PR) bleeding for five days and lower abdominal pain for a day, according to the medical history provided by her family. On admission, the patient was clinically stable (temperature 37.3°C, blood pressure 135/90 mmHg, heart rate 94 bpm). A physical examination revealed that her abdomen was soft and non-distended. There was tenderness at the lower abdomen with no rebound tenderness. A rectal examination revealed a ‘prolapsed rectum’ of about 4 cm, with a 2 cm × 1 cm broad-based polyp at the leading point and bleeding from the polyp (
Fig. 1
Photograph shows rectal prolapse with broad-based polyp at the leading point.

Fig. 2
Abdominal radiograph taken on arrival shows faecal loading but no sign of obstruction.

A sigmoidoscopy was subsequently performed on Day 2 of admission. During the procedure, we inserted the sigmoidoscope to 25 cm and found a large rectal prolapse with a polyp as the lead point, with no obvious intussusception. Biopsies of the polyp were taken. However, the procedure was aborted after insertion to 25 cm due to difficulties with the insertion. Repeated reduction of the prolapsed rectum was attempted without success. The histology report of the rectal biopsy indicated an adenomatous lesion with severe dysplasia.
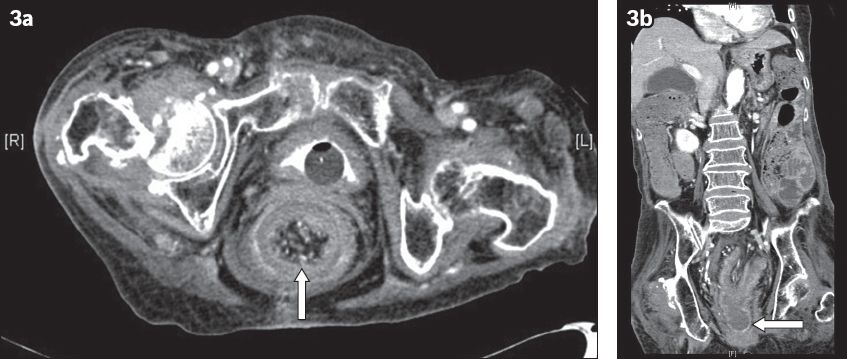
The patient was subsequently prepared for surgical intervention for the rectal prolapse. However, she developed signs of sepsis with tachycardia and a raised white blood cell count five days after admission. Computed tomography (CT) of the abdomen and pelvis was performed on clinical suspicion of an abdominal cause for the sepsis. The result showed a rectosigmoid junction intussusception with a lead point distal to the anal canal. This was associated with proximal bowel dilation suggestive of intestinal obstruction with a distended caecum (
Fig. 3
CT images of the (a) abdomen and (b) pelvis show sigmoid colon intussusception (arrows).
An emergency open laparotomy was performed. Intraoperatively, we found a large long-segment sigmoid intussusception (
Fig. 4
Intraoperative photograph shows sigmoid intussusception.
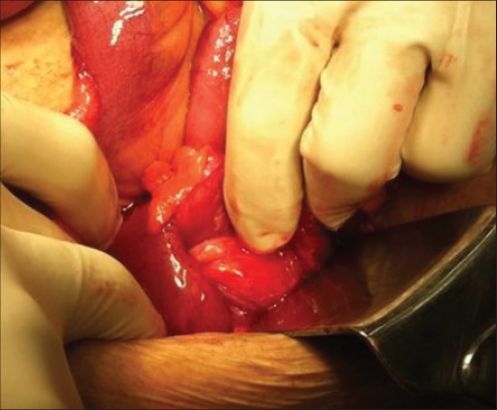
Fig. 5
Photograph shows sample from the sigmoid intussusception (left) and colon with caecum necrosis (right) following total colectomy.

Postoperatively, the patient was managed in a surgical high-dependency unit. She developed postoperative ileus and atrial flutter, which were responsive to medical treatment. Total parenteral nutrition was started and the patient progressed to nasogastric tube feeding on postoperative day (POD) 5. She was transferred to the general ward on POD 6. Due to mild dysphagia secondary to postoperative deconditioning, the patient was discharged with nasogastric tube feeding on POD 17. The final histology of the polyp was that of a partially necrotic polyp, tubulovillous adenoma, with high grade dysplasia. A focus on the base of the polyp raised the suspicion of submucosal invasion.
DISCUSSION
Intussusception in adults is relatively rare and presentations are not typical, compared with the triad of symptoms described in paediatric cases (abdominal pain, mass and PR bleeding). In a retrospective review of 41 intussusception cases, 95.1% (39/41) had abdominal pain, 26.8% (11/41) had bloody stool and 34.1% (14/41) had a palpable abdominal mass. However, the classic triad presentation was only seen in 9.8% (4/41) of the adult patients in the study.(2) Most adult intussusception patients present with chronic, intermittent and nonspecific symptoms, making accurate diagnosis relatively difficult. As a result, the majority of diagnoses are delayed, missed or only made during surgery. In our case, the patient appeared to have rectal prolapse, an even rarer presentation for intussusceptions.
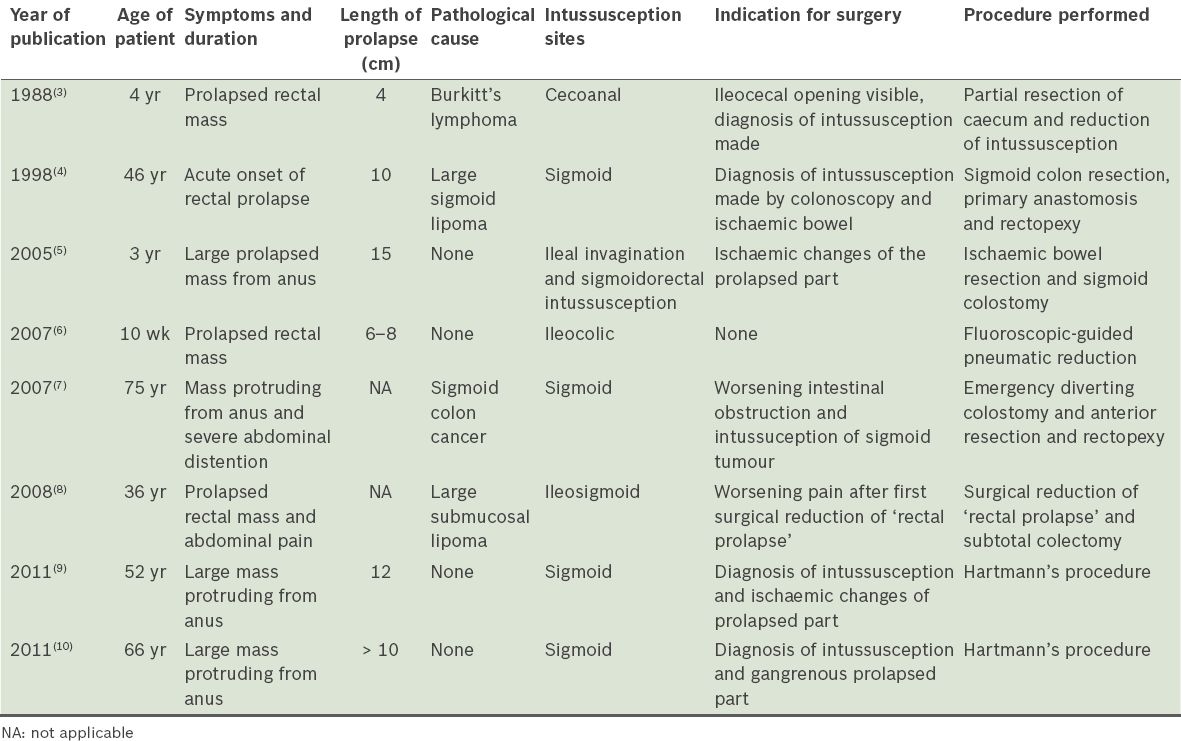
In
Table I
Similar case reports of intussusception presenting as rectal prolapse published in the last 30 years.
When differentiating between intussusceptions and rectal prolapse, physicians need to take note of the following three areas: patient history; physical examination; and further investigations.
Although intussusceptions through the anus and rectal prolapse share some common features in the patient’s medical history (such as chronic constipation), patients with intussusception usually have chronic abdominal pain associated with distension. Some patients can have chronic obstructive symptoms such as nausea or vomiting, and others can develop symptoms of malignancy such as weight loss and abdominal mass. However, some symptoms might be more suggestive of the diagnosis of intussusception. Dvorkin et al compared the symptoms of 377 patients with either rectal intussusception or rectocele with their proctography results. They found that the symptoms of anorectal pain and prolapse were highly predictive of isolated intussusception, as compared with rectocele. The symptom of ‘toilet revisiting’ was also more closely associated with the finding of rectoanal intussusception.(11)
During physical examination, firstly, it is important to note that intussusceptions may have a leading point lesion on the protruding mass (as presented in our case), which does not occur in cases of rectal prolapse. Of the eight cases presented in
Further investigations can help to identify intussusceptions. First, endoscopic investigations such as colonoscopy and sigmoidoscopy play an important role in evaluating the underlying causes (leading point) of intussusceptions and obtaining a histology sample, which will help in planning further treatments.(12) Second, CT of the abdomen and pelvis is one of the most useful and accurate methods to identify intussusceptions.(13,14) It can provide sufficient information about the site of the intussusception, its extent, underlying lesion, dilatation of bowel, signs of obstruction and most importantly, whether it is noninvasive.
For early definitive management, prompt diagnosis and differentiation between a rectal prolapse and a large transanal intussuception is crucial, especially for severely ill patients with a lesion as a leading point. Diagnoses should be built on careful history-taking, physical examination and relevant investigations. An early CT of the abdomen and pelvis may be helpful if intussusception is of diagnostic concern.


