INTRODUCTION
Incidental pancreatic lesions are increasingly being detected due to the increasing use of cross-sectional imaging such as computed tomography (CT) and magnetic resonance (MR) imaging. These pancreatic lesions can be broadly categorised into hypervascular and hypovascular lesions by comparing the degree of lesion enhancement to the background pancreatic parenchymal enhancement. For practicality, we define pancreatic lesions as hypervascular when they show enhancement greater or equal to that of the pancreatic parenchyma on either CT or MR imaging vis-a-vis hypovascular lesions, which characteristically enhance less than the background pancreatic parenchyma. Hypovascular lesions have been widely described, including ductal adenocarcinoma and chronic focal pancreatitis.(1) A few prior published reviews related to hypervascular pancreatic masses have focused on the differential entities or their malignant potential.(2,3) To the best of our knowledge, there is a lack of an algorithm-based approach that enables general radiologists to prospectively differentiate the various hypervascular pancreatic lesions, as presented in this pictorial essay. We further discuss the pertinent radiologic-pathologic features of each differential diagnosis and illustrate them using individual case examples.
ALGORITHM-BASED APPROACH
Our proposed algorithm (
Fig. 1
Flowchart shows an algorithm-based approach to hypervascular pancreatic lesions. *Acinar cell carcinoma (ACC) is classically described as a hypovascular lesion. Based on our experience, not all ACCs demonstrate this finding; some show similar enhancement to the pancreatic parenchyma (when the central necrosis is excluded). Other reasons are discussed in the text. CT: computed tomography; EUS: endoscopic ultrasonography; FNA: fine needle aspiration; Ga-68 DOTATATE PET/CT: gallium-68 positron emission tomography/computed tomography; HDRBC: heat-damaged red blood cell; MR: magnetic resonance; pNET: pancreatic neuroendocrine tumour; SCN: serous cystic neoplasm; SI: signal intensity; SPECT: single-photon emission computed tomography; SPEN: solid pseudopapillary neoplasm; Tc-99m: technetium-99m
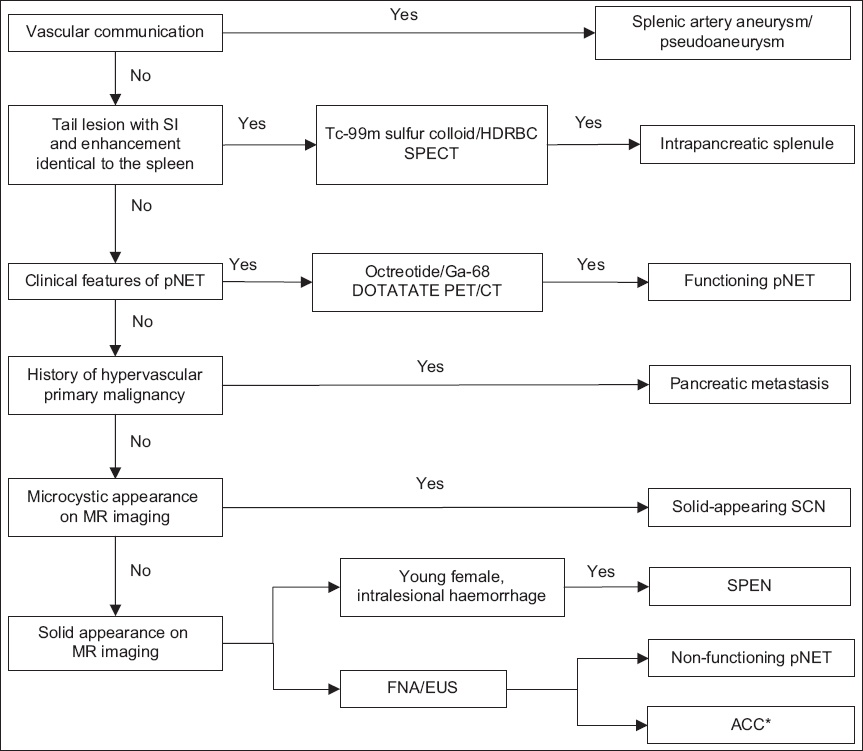
Stepwise, downwards in the algorithm, the diagnoses of pancreatic neuroendocrine tumour (pNET) and hypervascular metastasis are considered, as they are the more common conditions presenting as hypervascular lesions in the pancreas. These are followed by less common differential diagnoses such as solid-appearing serous cystic neoplasm (SCN), solid pseudopapillary epithelial neoplasm (SPEN) and acinar cell carcinoma (ACC). ACC should be the last to be considered, as it is the least common and also lacks the associated clinical characteristics; its diagnosis is often made retrospectively by histology.(4)
SPLENIC ARTERY ANEURYSM OR PSEUDOANEURYSM
Splenic artery aneurysm represents the third most common site of intra-abdominal aneurysms, following abdominal aorta and iliac arteries. A true aneurysm involves all the three walls (intima, media and adventitia) of the splenic artery, while a pseudoaneurysm usually only involves one or more walls of the splenic artery. Splenic artery aneurysms usually measure less than 3 cm (range 2–9 cm).
The exact pathophysiology is not known, but it is believed to be associated with systemic hypertension, portal hypertension, cirrhosis, liver transplant and pregnancy.(5) Patients with this condition are often asymptomatic, and the lesion is usually detected incidentally. The risk of rupture is reported to be around 2%–3%,(6) with the rate of rupture increasing if other risk factors are present, such as size of more than 2 cm, portal hypertension, pregnancy and being a liver transplant recipient.(5) Management of a splenic artery aneurysm is beyond the scope of this pictorial essay. In general, for pregnant women with incidental splenic artery aneurysm, the decision for expected management, embolisation or surgery requires a balance between the risks and benefits of the treatment options, such as gestational age at time of diagnosis, size of aneurysm and the presence of symptoms.(7) In pre-liver transplant patients (i.e. patients on the transplant waiting list), treatment of an asymptomatic aneurysm is usually postponed until the time of transplant, because the aneurysm is often small in size (< 3 cm) and there is fear of adhesion when the splenic artery is needed for vessel anastomosis in the surgery. In post-transplant recipients, the therapeutic procedures are often complex.(8)
Pseudoaneurysms of the splenic artery usually measure more than 3 cm, with a mean size of about 4.8 cm (range 0.3–17.0 cm).(9) They are often iatrogenic and associated with trauma, pancreatitis and, rarely, peptic ulcer disease causing secondary splenic artery injury.(5) Patients can present with abdominal pain (29.5%), haematochezia or melena (26.2%), and haematemesis (14.8%).(5) The risk of rupture of a pseudoaneurysm is higher (37%), with a mortality rate of about 90%; thus, making a correct diagnosis and prompt treatment are important.(5)
On imaging, the diagnosis of a splenic artery aneurysm or pseudoaneurysm is often unequivocal. The lesion shows communication with the splenic artery and has a similar enhancement to that of the aorta (
Fig. 2
Axial contrast-enhanced CT images in (a) arterial and (b) portal venous phases show a homogeneously enhancing ovoid lesion at the tail of the pancreas (arrows) with communication with the distal splenic artery (arrowheads), consistent with a splenic artery aneurysm. (c) Three-dimensional image clearly shows the communication to the splenic artery with the aneurysm (arrow).
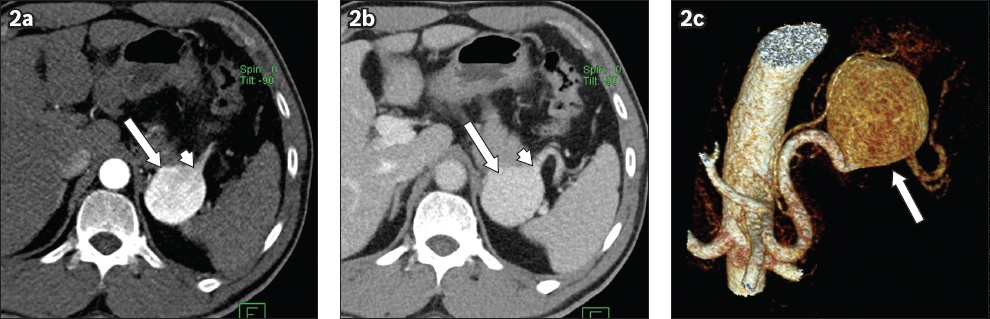
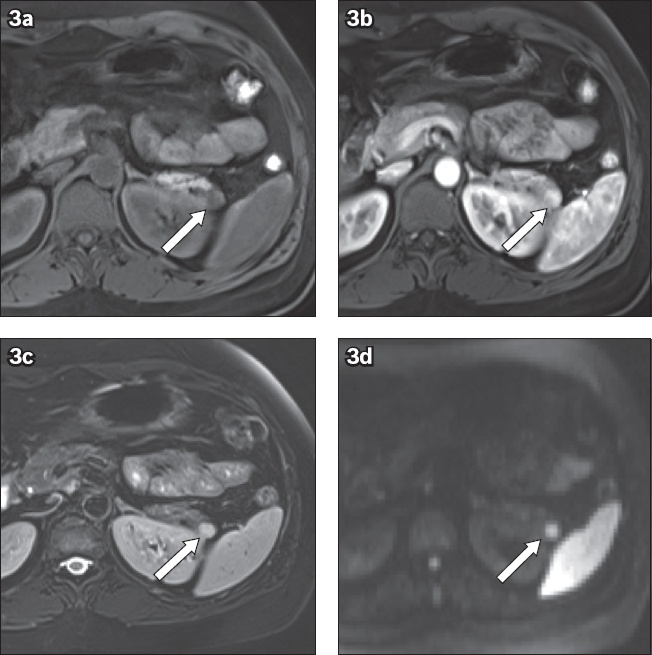
Table I
Differences between a splenic artery aneurysm and pseudoaneurysm.
INTRAPANCREATIC SPLENULE
Accessory spleen is a relatively common congenital condition that is often discovered incidentally on imaging performed for other causes. Previous autopsy reports suggest that it occurs in approximately 17% of the population.(10) When an accessory spleen is found in the pancreas, the condition is called intrapancreatic splenule, which makes up approximately one sixth of all cases of accessory spleens.(11) Familiarity with this condition is essential to avoid misdiagnosing it as a malignancy, such as neuroendocrine tumour or hypervascular metastasis, and prevent unnecessary investigations.
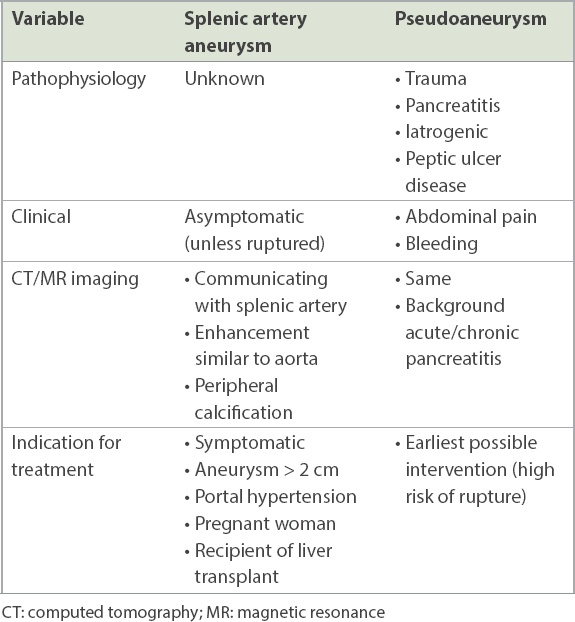
Intrapancreatic splenule commonly presents as a small, well-defined hypervascular lesion in the tail of the pancreas with a size of approximately 1–3 cm.(11) As it comprises the same splenic tissues as the parent spleen, it is not surprising to observe the same MR signal intensity, CT attenuation and pattern of enhancement as the parent spleen. In the arterial phase (on either CT or MR imaging), the lesion demonstrates a characteristic serpiginous appearance, similar to the parent spleen. When this feature is seen, it increases the likelihood of the diagnosis.(11) When CT is not diagnostic, MR imaging can be performed, as it offers superior soft tissue characterisation that aids in making a more specific diagnosis (
Fig. 3
Incidental hypervascular lesion found at the tail of the pancreas (arrows) shows signal intensities and degree of contrast enhancement similar to that of the adjacent spleen on the axial sections of (a) fat-suppressed T1-weighted pre-contrast, (b) arterial phase, (c) portal venous phase and (d) diffusion-weighted images. The findings are consistent with those of an intrapancreatic splenule.
If the diagnosis remains equivocal, radionuclide studies such as technetium-99m heat-damaged red blood cell (Tc-99m HDRBC) or Tc-99m sulfur colloid scintigraphy are extremely useful, as the splenic tissue takes up and accumulates the radiotracers. Between the two nuclear medicine studies, we prefer Tc-99m HDRBC because it offers higher specificity with 90% of HDRBC uptake in the splenic tissue.(3) The downside of Tc-99m HDRBC is the need to handle blood products and the longer scanning time.(3)
PANCREATIC NEUROENDOCRINE TUMOUR
pNETs arise from the endocrine cells of the pancreas(3) and commonly present in individuals aged 50–70 years.(12) pNETs are categorised clinically as functional and non-functional, depending on the presence or absence of symptoms associated with excessive secretion of hormones (e.g. insulin, glucagon, gastrin, vasoactive intestinal peptide and somatostatin). Most of the pNETs detected nowadays are non-functional (~ 60%–80%) due to the increasing use of cross-sectional imaging. Non-functional pNETs have variable malignant potential, ranging from slow growing and indolent to being aggressively metastasising lesions.(3) pNETs can occur sporadically or arise in association with genetic syndromes such as von Hippel-Lindau disease, multiple endocrine syndrome Type 1, tuberous sclerosis and neurofibromatosis.(3)
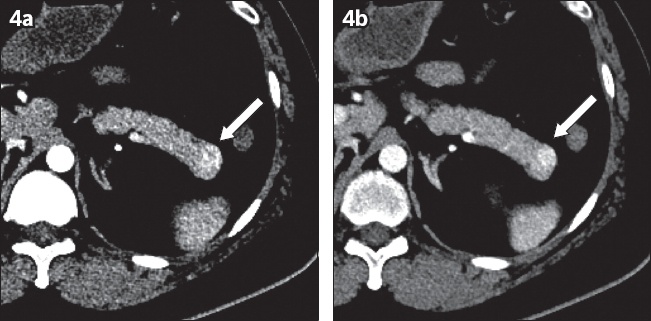
On contrast-enhanced CT or MR imaging, pNETs commonly present as a well-circumscribed hypervascular lesion in the pancreas with a different degree of enhancement compared to the spleen, thus excluding the diagnosis of intrapancreatic splenule (
Fig. 4
A 38-year-old man presented with hypoglycaemia. Axial contrast-enhanced CT images in (a) arterial and (b) portal venous phases show a hyper-enhancing lesion at the tail of the pancreas with a degree of enhancement greater than that of the adjacent spleen (arrows). The lesion was histologically confirmed to be a well-differentiated neuroendocrine tumour (insulinoma).
When the diagnosis is equivocal, radioisotope studies such as Indium-111 octreotide scintigraphy or the currently preferred gallium-68 (Ga-68) DOTATATE positron emission tomography (PET/CT), are useful. Ga-68 DOTATATE PET/CT has a higher diagnostic accuracy with a sensitivity of 93% and specificity of 96%.(13) As making the diagnosis based on imaging alone can sometimes be difficult, tissue sampling may be required in some cases.(3)
Although several non-benign features have been described in the literature (e.g. hypovascularity, cystic morphology, presence of calcification, pancreatic ductal dilatation, adenopathy and size > 3 cm), the aggressive behaviour of pNETs often requires histopathology to assess for mitotic activity and the percentage of nuclear antigen Ki-67.(12) Nevertheless, if locoregional invasion and liver or nodal metastases are seen on imaging, the diagnosis of a malignant pNET should be raised.(12)
HYPERVASCULAR METASTASES
Metastasis to the pancreas is rare, consisting of 2%–5% of all pancreatic malignancies.(14) The most common primary malignancy that metastasises to the pancreas is renal cell carcinoma (RCC), followed by lung, breast and colorectal malignancies, as well as melanoma.(3) Delayed pancreatic metastasis occurring more than ten years after the initial diagnosis of RCC has been reported and can happen in more than 10% of patients. About half of the patients with pancreatic metastases are asymptomatic, while the other half may present with abdominal pain, obstructive jaundice or pancreatitis.(14)
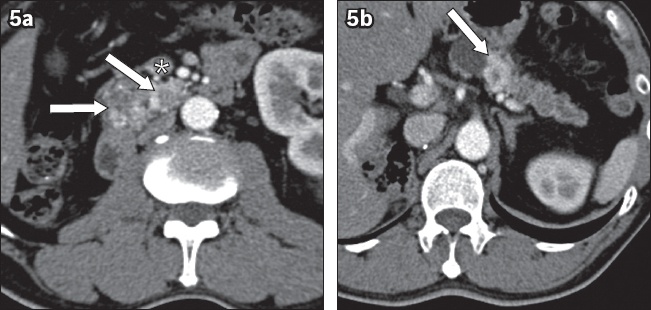
Imaging features of hypervascular pancreatic metastases can closely mimic those of primary pNETs, presenting as a well-defined hypervascular lesion without main pancreatic ductal dilatation.(14) However, metastases to the pancreas often manifest with multiplicity and patients often have a previous history of hypervascular primary malignancies or evidence of nephrectomy, which suggests a prior RCC (
Fig. 5
Hypervascular metastases from renal cell carcinoma. (a & b) Axial contrast-enhanced CT images of a patient with previous right nephrectomy for renal cell carcinoma show multiple hyper-enhancing lesions in the pancreas (arrows), some with necrotic centres, suspicious for hypervascular pancreatic metastases. The superior mesenteric vein (asterisk) is seen. Note the absence of the right kidney.
SOLID-APPEARING SEROUS CYSTIC NEOPLASM
As the name implies, SCN of the pancreas usually presents as a cystic lesion in about 80% of cases.(15) It is referred to as the ‘grandmother’ lesion, classically occurring in women above 60 years of age and typically located in the head of the pancreas, as compared to the mucinous cystic neoplasm, which is more commonly seen in the body and tail of the pancreas in women aged 40–50 years.(15)
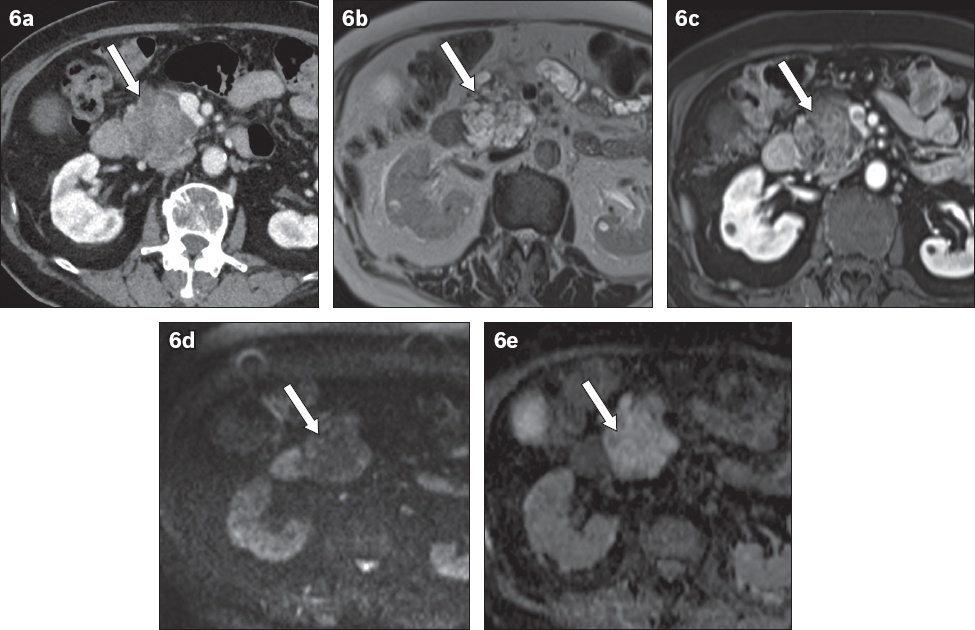
In a minority (about 20%), SCNs can present as solid-appearing lesions due to their closely apposed enhancing septae and walls.(3) In this situation, T2-weighted MR images are extremely helpful in establishing the microcystic nature of the pseudo-solid lesion. SCNs tend to have a lobulated margin along with microcystic morphology, giving rise to their honeycomb appearance. Sometimes, a central scar or calcification may be seen, adding to diagnostic confidence (
Fig. 6
(a) Axial contrast-enhanced CT image shows a solid-appearing heterogeneous mass in the head of the pancreas (arrow). (b) T2-W image shows a lobulated microcystic lesion with central scar (arrow). (c) T1-W post-contrast image shows enhancement of the septae and central component (arrow). (d) Diffusion-weighted and (e) apparent diffusion coefficient images show T2 shine-through without restricted diffusion (arrows). The constellation of findings suggests serous cystic neoplasm of the pancreas.
SOLID PSEUDOPAPILLARY EPITHELIAL NEOPLASM
SPEN occurs almost exclusively in young women aged below 40 years.(16) Patients are often asymptomatic, but if the mass is large, some may present with abdominal distension or vague abdominal pain. SPEN is recognised as an indolent tumour with potential malignant behaviour (harbouring up to approximately 10%–20% malignant potential).(16) In our experience, middle-aged men can sometimes present with this pathology.
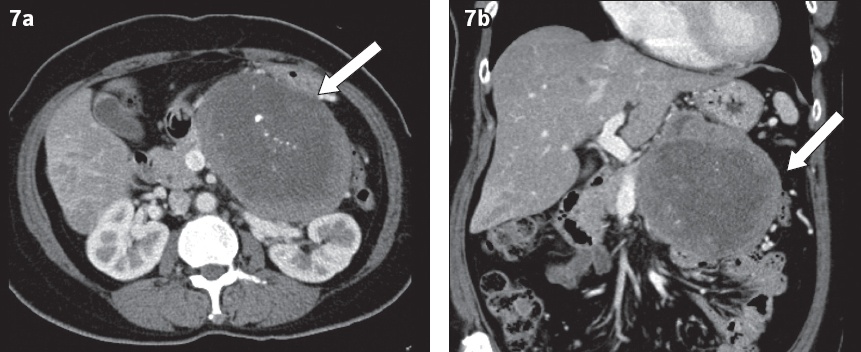
Typically, SPEN presents as a well-defined solid mass in the tail of the pancreas (
Fig. 7
(a) Axial and (b) coronal contrast-enhanced CT images of the abdomen in a 35-year-old woman show a large heterogeneously and peripherally enhancing mass (arrows) at the distal pancreas with a well-defined margin, necrotic centre and internal coarse calcifications. It was histologically diagnosed to be a solid pseudopapillary tumour of the pancreas.
ACINAR CELL CARCINOMA
ACC is a rare epithelial neoplasm of the pancreas with acinar cell differentiation.(4) It is an aggressive tumour with high malignant risk.(3) It typically occurs in elderly male patients (aged 50–70 years). The clinical symptoms are often non-specific, with abdominal pain being the most common presentation (about 55%), followed by nausea/vomiting, loss of weight and loss of appetite. Uncommonly, patients with ACC can present with paraneoplastic syndromes due to hyperlipasaemia, manifesting as painful and erythematous subcutaneous nodules and multiple lytic lesions involving the peripheral joints (e.g. wrists, hands, ankle, feet and knees), and mimicking metastases.(4)
Although ACC is typically described in the literature as a large (> 4 cm) exophytic mass in the pancreas with heterogeneous enhancement and a well-defined margin (
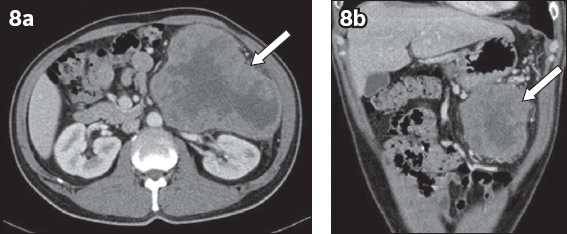
Fig. 8
(a) Axial and (b) coronal CT images of an elderly man show a large exophytic heterogeneously and peripherally enhancing mass at the tail of the pancreas (arrow). The mass has a necrotic centre, and is distinct from and exerts mass effect on the surrounding structures (e.g. left kidney, stomach and bowel loops). It was histologically diagnosed to be acinar cell carcinoma of the pancreas.
CONCLUSION
Hypervascular pancreatic lesions have a range of differential diagnoses from benign to malignant conditions. We have described, with specific examples, an algorithm-based approach that will enable radiologists to make a sensible and appropriate prospective diagnosis in daily clinical practice.
SMJ-62-119.pdf


