Mrs Tan took her daughter Emma, a well-thrived three-year-old girl, to the family clinic for two days of fever, sore throat and rhinorrhoea. Apart from slight decreased appetite, Mrs Tan reported that Emma’s activity level and behaviour were not affected. During the examination, Emma was interactive, her nose was congested with clear rhinorrhoea, and there was pharyngeal injection without exudates. You discovered bilateral non-tender, mobile cervical lymph nodes that were up to 1.5 cm in size. Mrs Tan was uncertain if they were present prior to her current illness. There was no organomegaly or other lymphadenopathy. You treated Emma for viral respiratory tract illness and made plans to review her in two weeks for her cervical lymphadenopathy.
WHAT IS LYMPHADENOPATHY?
Lymphadenopathy is defined as the presence of one or more lymph nodes of more than 1 cm in diameter, with or without an abnormality in character.(1) In children, it represents the majority of causes of neck masses, which are abnormal palpable lumps or swellings.
HOW RELEVANT IS THIS TO MY PRACTICE?
Cervical lymphadenopathy in the paediatric population is common in general medical practice and presents either as a primary complaint of neck mass or as an incidental finding during clinical examination. Park reported that 90% of all children aged 4–8 years have palpable lymphadenopathy.(2) In a systematic review of paediatric cervical lymphadenopathy involving 2,687 patients, two thirds of the cases were due to non-specific benign aetiology with no definitive diagnosis, and 4.7% were secondary to malignancy.(3)
When first reviewing a child with cervical lymphadenopathy, the primary care physician is faced with a conundrum – manage at primary care or refer for specialist review? We propose that the physician’s familiarity with the differential diagnoses of lymphadenopathy and neck masses increases the success rate of managing this in primary care. An evidence-based evaluation framework may reduce unnecessary diagnostic tests and therapies, as well as enable physicians to counsel their patients and caregivers appropriately.
WHAT CAN I DO IN MY PRACTICE?
Clinical approach
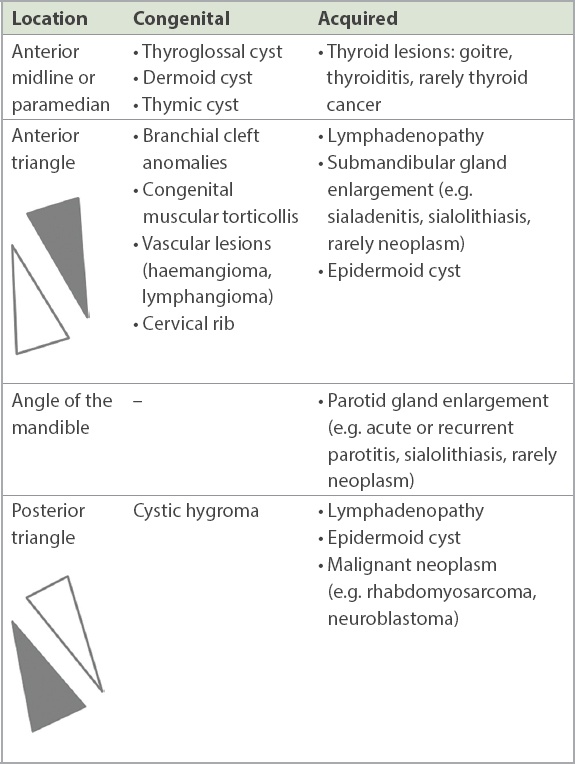
In the initial approach, it is important to first consider the broad differential diagnosis of cervical lymphadenopathy, including other causes of neck masses that may mimic it closely (
Table I
Differential diagnoses of neck masses.
A thorough history and physical examination are fundamental steps in the evaluation of a child with the complaint of a neck mass.
History
The following questions are important in evaluating for the various possible causes of neck masses in children:
Patient’s age
Duration of neck mass: (a) present since birth or recently discovered, and for how long; and (b) recurrence of neck mass
Associated symptoms: (a) focal symptoms (e.g. pain, erythema); (b) infective symptoms (e.g. fever, sore throat, other localising symptoms of infection); (c) rashes, arthralgia and other features of Kawasaki disease (KD), including conjunctival injection, erythema/cracking of lips and tongue, and erythema/swelling of hands and feet; and (d) weight loss, loss of appetite, night sweats, fatigue, easy bruising and pallor
Recent illnesses (e.g. pharyngitis, tonsillitis, dental infections)
History of recurrent infections, recurrent skin abscesses or recurrent lymphadenopathy
Drug history, including any treatment with antibiotics
Exposure to animals (particularly cats), insects, sick persons, persons with tuberculosis or chronic cough
Recent travel history
Immunisation status
Physical examination
A complete physical examination always includes a general inspection of the child’s growth parameters (i.e. growth charts) and general health status. The presence of pallor or jaundice should be determined. In addition to the location of the neck mass, it is important to examine the following:
Size of lesion
Quality of lesion: (a) tenderness, warmth, mobility, fluctuance, consistency and erythema; and (b) other overlying skin changes such as cutaneous sinus tract
A sequential examination of the lymph node chains of the head and neck (
A quick examination of the eyes, ears, nose, mouth and throat should be performed to look for common sources of infection that could cause cervical lymphadenopathy (
To complete the examination, assess for the presence of rashes, KD features, petechiae/purpura and joint swelling, and palpate the abdomen to assess for hepatosplenomegaly or abdominal masses.
Fig. 1
Illustration shows an overview of the lymph node regions of the neck (reproduced with permission from Dr Marc Ong Weijie).
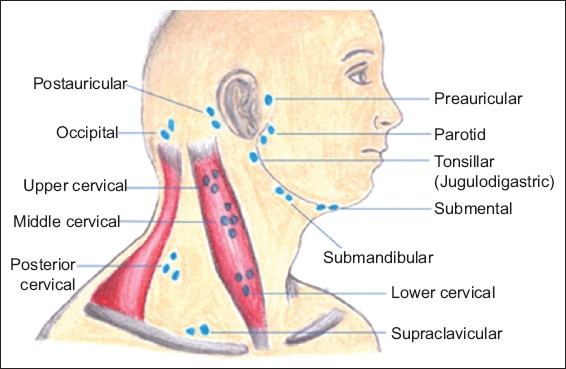
Table II
Summary of drainage areas for cervical lymph node groups.
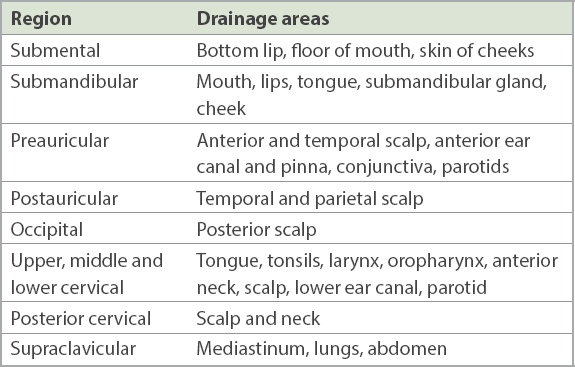
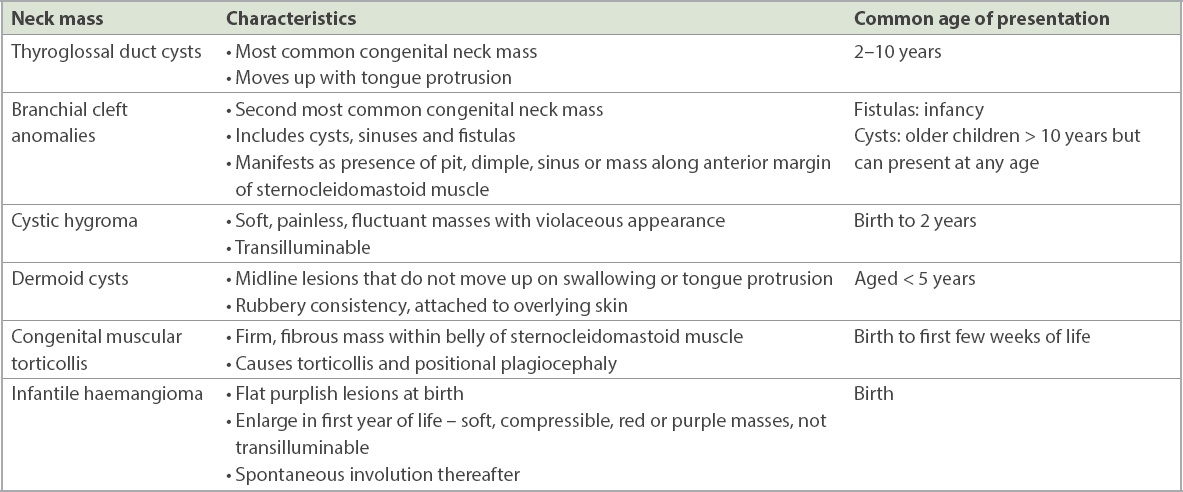
Table III
Common congenital neck masses.
WHAT ARE THE MAIN CAUSES?
In a child with cervical lymphadenopathy, the duration of lymphadenopathy is a key consideration in determining its possible aetiology, which can be categorised into four main groups: infectious, immunologic, malignancy and miscellaneous causes. The causes can then be classified according to the origin and time course of symptoms, as presented in
Table IV
Causes of cervical lymphadenopathy.
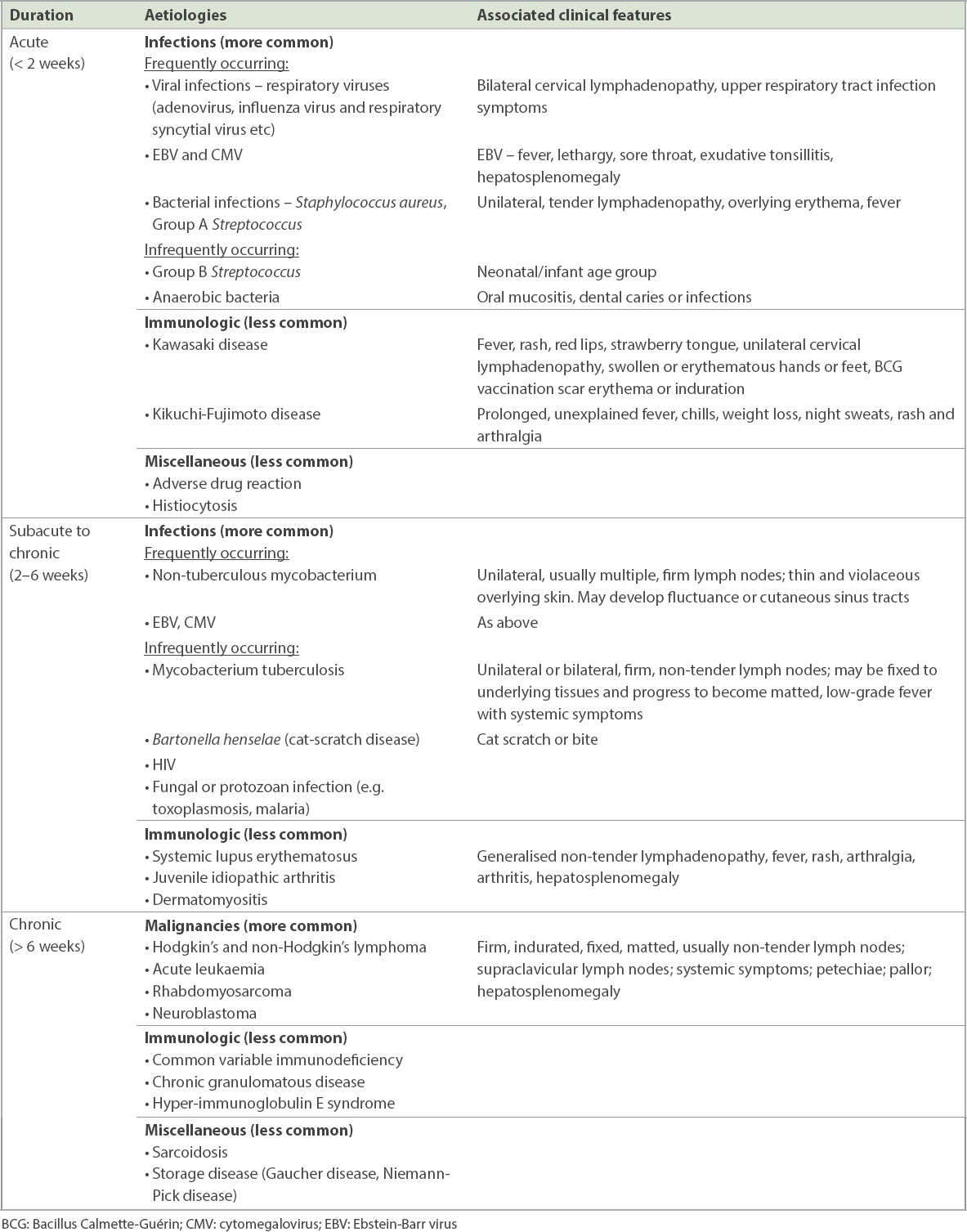
Acute cervical lymphadenopathy
Infective causes
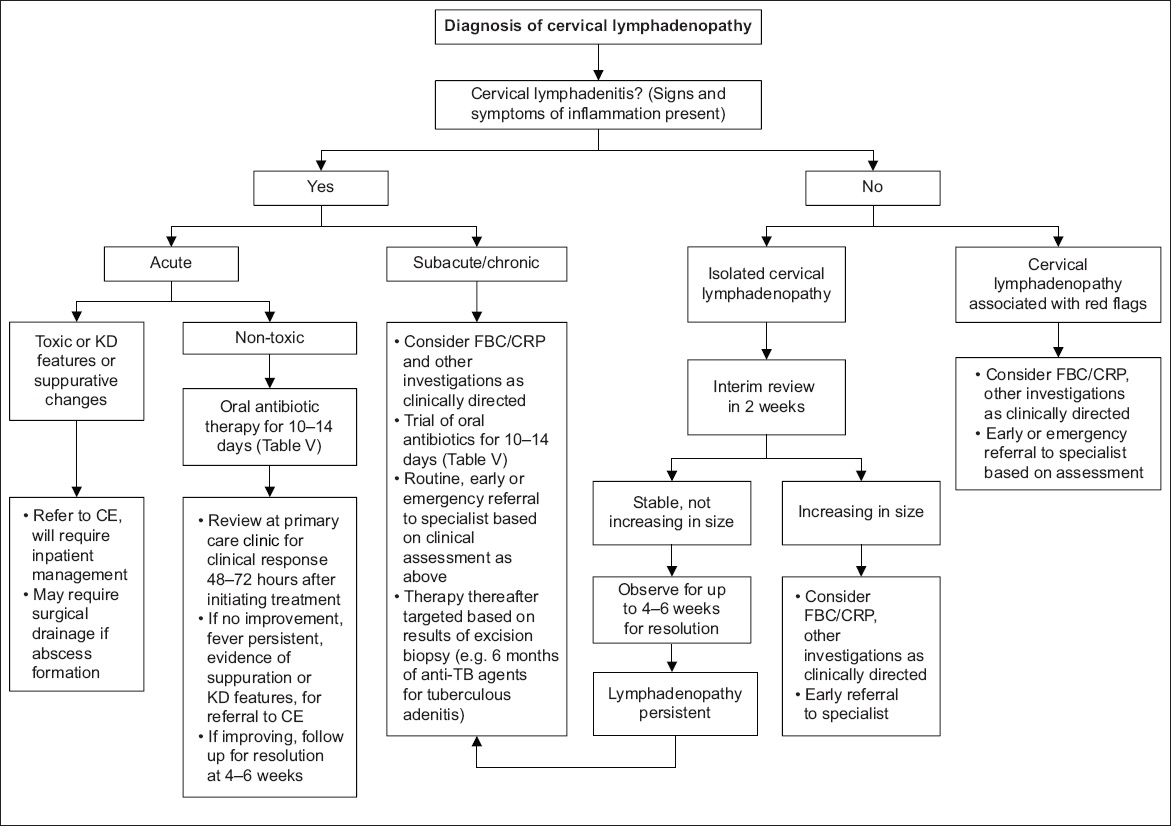
The most common scenario of acute cervical lymphadenopathy is enlargement of bilateral lymph nodes in the correct nodal drainage chain during an acute infection. This represents a self-limiting, transient response of lymphatic tissue hyperplasia to a local infective process that improves with resolution of the viral illness. In the absence of red flags, it can be managed according to
Fig. 2
Flowchart summarises the general principles for the management of cervical lymphadenopathy. CE: children’s emergency department; CRP: C-reactive protein; FBC: full blood count; KD: Kawasaki disease; TB: tuberculosis
Ebstein-Barr virus (EBV) and cytomegalovirus (CMV) infections may be more common in older children of school-going age and adolescents. Children with EBV infection often present with a clinical picture of infectious mononucleosis, characterised by generalised lymphadenopathy, sore throat, fatigue and fever. This may be accompanied by exudative tonsillitis and hepatosplenomegaly.
Children can also present with acute unilateral cervical lymphadenitis, caused by bacterial infection. Lymphadenitis is defined as lymphadenopathies caused by an inflammatory process, resulting in enlarged, tender lymph nodes with or without overlying erythema.(6) The most common causative pathogens are Staphylococcus aureus or Streptococcus pyogenes (Group A Streptococcus).(5) The primary source of infection may or may not be found. Acute unilateral cervical lymphadenitis most often affects children aged 1–4 years. Some may progress to have abscess formation. Less commonly, it may be caused by anaerobic bacteria associated with dental infections and abscesses.
An important distinguishing feature between viral and bacterial lymphadenitis is whether there is self-resolution. Primary bacterial lymphadenitis or a viral lymphadenitis with secondary bacterial infection should be considered if the patient does not improve after 4–7 days.
Immunologic causes
Kawasaki disease
KD is the most common childhood acute vasculitic disease of unclear aetiology and is associated with the development of coronary artery complications. It mainly affects children under five years of age. The diagnosis is clinical, based on the presence of fever lasting five days or more, and a constellation of symptoms, which may not all be present. These include polymorphous exanthem, bilateral non-suppurative conjunctivitis, changes in lips and oral mucosa, changes in extremities, and usually unilateral cervical lymphadenopathy measuring more than 1.5 cm. KD should be considered in a child with persistent fever and cervical lymphadenitis despite the use of antibiotics.
Most reports in the literature describe KD as an uncommon cause of cervical lymphadenopathy, with the highest incidence in Asian countries, in particular Japan, South Korea and Taiwan.(7) However, in the wake of the current coronavirus 2019 (COVID-19) pandemic, there has been increasing interest in KD in European countries with large COVID-19 outbreaks. These countries have reported cases of a paediatric multi-system inflammatory syndrome, where critically ill children present with features of shock and Kawasaki-like disease, which may be temporally associated with COVID-19 infection.(8) Although Singapore has not yet seen such cases among the paediatric population, the Ministry of Health has issued an advisory for medical practitioners to be aware of this condition. This further highlights the importance of early recognition of KD at a primary care level, to facilitate early specialist referral.
Kikuchi-Fujimoto disease
Kikuchi-Fujimoto disease, also known as histiocytic necrotising lymphadenitis, is a lesser known clinical entity but is not as uncommon as previously perceived. It usually presents in older children and adolescents, most commonly aged 7–12 years, with unexplained fever and cervical lymphadenopathy. Accompanying symptoms include weight loss, night sweats, chills, rash and arthralgia. Although generally understood to be a self-limiting, benign condition of unknown aetiology, it can lead to significant complications including aseptic meningitis, with reports of progression to systemic lupus erythematosus.(9) A biopsy of the lymph node is required for histopathological diagnosis.
Miscellaneous
Less commonly, lymphadenopathy can be a result of an adverse drug reaction. Medications that may cause this include phenytoin, isoniazid, pyrimethamine and allopurinol.
Subacute or chronic cervical lymphadenopathy
Chronic infective causes
Atypical mycobacterial, or non-tuberculous mycobacterial (NTM) infection, often affects children aged 1–5 years. It is the most common cause of chronic cervical lymphadenopathy. Children with NTM infection present with progressive lymph node enlargement over weeks to months, although the onset may also be acute and very rapid. They are often afebrile and have unilateral, non-tender lymphadenitis, with thin and violaceous overlying skin. It commonly affects the upper anterior cervical and submandibular lymph nodes.(10) The affected lymph nodes may undergo rapid suppuration or rupture and form sinus tracts.
Mycobacterium tuberculosis infection is less common. It can affect all age groups, but usually older children above five years of age. It can cause unilateral or bilateral, firm, discrete, non-tender lymphadenopathy, often fixed to underlying tissues. There may be associated low-grade fever and systemic symptoms. There is usually a preceding history of exposure to tuberculosis, and 28%–71% of affected patients have abnormal chest radiographs.(10)
Bartonella henselae infection (cat-scratch disease) causes a granulomatous infection that is transmitted by the scratch or bite of a cat.(4) Lymphadenopathy usually occurs after several weeks but can occur acutely as well.
Malignancy
Chronic cervical lymphadenopathy may be a presenting sign of a primary malignancy, or metastatic disease. The most common malignancies associated with cervical lymphadenopathy in the first six years of life are acute leukaemia, neuroblastoma, rhabdomyosarcoma and non-Hodgkin’s lymphoma. Thereafter, after six years of age, Hodgkin’s lymphoma is the most common malignancy, followed by non-Hodgkin’s lymphoma and rhabdomyosarcoma.(11) Worrying features include firm, indurated, fixed and matted lymph nodes that are usually not tender.
Immunologic
Autoimmune diseases, such as systemic lupus erythematosus, juvenile idiopathic arthritis and dermatomyositis, can cause chronic generalised lymphadenopathy. Lymph nodes are often non-tender and discrete, with a range of sizes from very small to a few centimetres in diameter.(6)
WHAT INVESTIGATIONS SHOULD BE UNDERTAKEN?
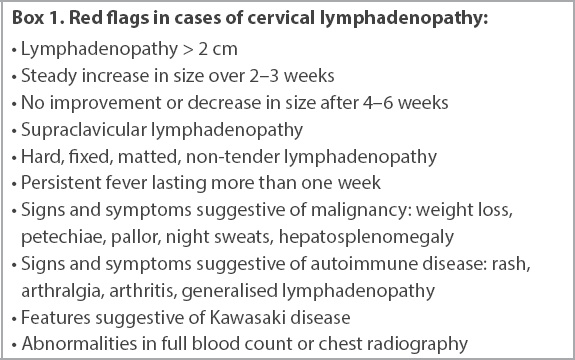
Investigations are necessary when cervical lymphadenopathy is subacute or chronic in presentation, has associated red flag features (
Box. 1
Red flags in cases of cervical lymphadenopathy:
In primary care
The following are preliminary investigations that can be done in the primary care setting to aid in diagnostic and subsequent management decisions. These tests are especially valuable in cases that are routinely referred to tertiary care, and can further assure the patient and their family if their results are deemed normal. Conversely, abnormalities in these investigations would prompt a more urgent referral. In cases where emergency referral is felt to be necessary or investigations are difficult to perform, testing can also be performed by the tertiary paediatric institution.
Blood investigations
Full blood count (FBC) and peripheral blood film (PBF) should be done. Raised total white cell count and neutrophilia are suggestive of a bacterial aetiology, whereas cytopenia can be seen in viral aetiologies, haematological malignancies or autoimmune conditions. Thrombocytosis might be present in cases of reactive cervical lymphadenitis or inflammatory conditions such as KD. It is important to note the differential white cell counts, as lymphopenia can be seen in systemic lupus erythematosus, and a high percentage of atypical lymphocytes or monocytes can be seen in infectious mononucleosis syndrome. The PBF might reveal the presence of blast cells in cases of haematological malignancies.
Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels are inflammatory markers that may be raised in infective (more likely from a bacterial cause) or inflammatory causes of cervical lymphadenopathy. However, for an inflammatory condition, a markedly raised ESR in relation to the CRP level would be more concerning.
Uric acid and lactate dehydrogenase (LDH) levels should also be checked. Raised uric acid and LDH levels are indicative of a high cell turnover state, and significantly raised levels are worrisome for an underlying malignancy. Liver function test (LFT) and renal panel are useful for determining multi-systemic involvement from the underlying condition.
The choice of blood tests is directed largely by clinical suspicion after assessment of the child. For example, if there are some features suggestive of malignancy, appropriate investigations would include FBC, PBF, and LDH and uric acid tests, while if there is a suspicion of autoimmune disease, FBC, CRP, ESR, LFT and renal panel tests would be appropriate. We propose that FBC and CRP tests are appropriate first-line blood investigations that can be performed, with other tests as clinically directed.
Imaging
Chest radiography is a helpful test to assess for evidence of mediastinal widening for cases of chronic lymphadenopathy, especially when malignancy such as lymphoma cannot be ruled out. Mediastinal widening may be suggestive of a mediastinal mass, or hilar adenopathy. This would be an indication for immediate emergency referral. It should also be performed in patients with a clinical suspicion of tuberculosis.
In tertiary institutions
Specific serologic and antibody tests
Specific serologic tests for EBV, CMV, Bartonella henselae and toxoplasmosis might be considered. The blood plasma anti-streptolysin O titre test can be used in the diagnosis of a streptococcal infection.
Imaging
Ultrasonography is advocated as the initial imaging modality for cervical lymphadenopathy, if required. It is useful in determining if complications such as an abscess formation have occurred, and can also be used to guide surgical drainage in such cases. It is also useful to differentiate lymphadenopathy from other causes of congenital or acquired neck masses. Other advantages of ultrasonography include lack of radiation exposure, easy availability, fast interpretation and lower cost compared to cross-sectional imaging. The disadvantage of ultrasonography is that it is operator dependent.
Computed tomography (CT) or magnetic resonance (MR) imaging investigations are particularly useful in evaluating neck masses located within the deep neck. Advantages of CT over MR imaging are that it is more readily available, has lower cost and has faster scan times. MR imaging is the imaging modality of choice to evaluate paediatric neck masses with suspected intracranial or intraspinal extension, and its significant advantage would be the lack of radiation exposure. However, sedation is usually required during MR imaging.
Diagnostic biopsy
The gold standard for tissue diagnosis is an excisional biopsy. There are several indications for which an excisional biopsy may be considered:(5,6,14) (a) persistent or progressive lymphadenopathy after 4–6 weeks; (b) lymph nodes greater than 2 cm; (c) symptoms and signs suggestive of malignancy; (d) supraclavicular lymph node; (e) unexplained, prolonged fever; (f) abnormal FBC (in particular cell line defects) or chest radiography; and (g) concerning features on ultrasonography or CT.
When indicated, the largest and most abnormal lymph node should be excised.(6) The biopsy specimen can be sent for histology, gram stain and bacterial culture, acid-fast bacilli (AFB) smear and culture, AFB polymerase chain reaction test, fungal smear and fungal culture. If there is a suspicion of lymphoma, an excision biopsy should be performed with a pathologist on standby so that a fresh specimen can be sent for appropriate staining.
WHAT ARE THE PRINCIPLES OF MANAGEMENT IN PRIMARY CARE?
Management of cervical lymphadenopathy in children should be targeted at the underlying aetiology. Most cases of reactive cervical lymphadenopathy present with isolated bilateral, mobile, small sub-centimetre lymphadenopathy in response to a self-limiting viral illness, and reassurance by the primary care provider is often sufficient. In cases of isolated cervical lymphadenopathy of 1–2 cm with no other red flag features, patients should be followed up for 4–6 weeks until the swelling of the lymph nodes has resolved,(6,14) with an interim follow-up at two weeks where feasible to ensure that there is no significant increase in size.
For acute non-toxic cervical lymphadenitis, patients can be reviewed 48–72 hours after starting oral antibiotics; lack of improvement, persistence of fever, evidence of suppurative changes or development of KD features should prompt emergency referral.
WHEN SHOULD I REFER TO A SPECIALIST?
Children with red flags based on history and physical examination (Box 1) that suggest more worrisome underlying disease(5,6,10,12) warrant further investigations and referral for specialist assessment. As a general guide, these patients can be referred to paediatric medicine, or to the ear, nose and throat department for cases that may benefit from biopsy or when congenital neck masses are suspected. For children who appear unwell and present with features suggestive of bacterial lymphadenitis, especially in infants and toddlers for whom a thorough clinical assessment might be more challenging, an emergency referral to a tertiary paediatric hospital would be necessary for initiation of early intravenous antibiotics.
The timeliness of referral largely depends on the physician’s discretion, based on clinical assessment. We propose the following timelines as a guide:
Routine referral (seen within 4–6 weeks) for persistent isolated lymphadenopathy < 2 cm not improving after 4–6 weeks with no other red flag features
Early referral (seen within 2–3 weeks) for lymphadenopathy > 2 cm, steady increase in size during observation, signs and symptoms suggestive of autoimmune disease
Emergency referral for toxic cervical lymphadenitis, or acute cervical lymphadenitis with no improvement 48–72 hours after starting oral antibiotic therapy, features of KD, associated persistent fever > 5 days, evidence of suppuration, signs and symptoms strongly suggestive of malignancy, chest radiography changes (e.g. mediastinal widening), or significant laboratory test abnormalities.
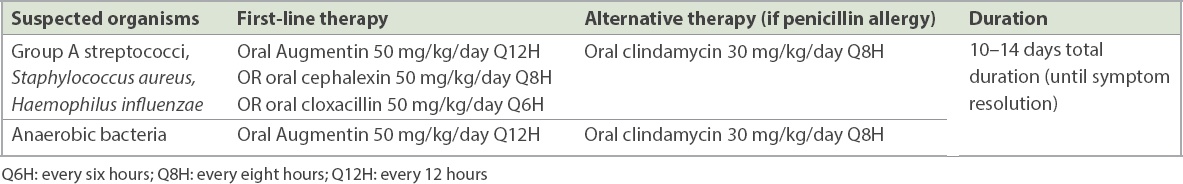
Table V
Recommended antimicrobial therapy for acute cervical lymphadenitis.
TAKE HOME MESSAGES
-
Cervical lymphadenopathy is a common problem in children, with reactive lymphadenopathy from a variety of viral infections being the most common cause. In these instances, systemic antibiotics are not warranted.
-
Features suggestive of cervical lymphadenitis secondary to bacterial infection include an acute presentation, fever, and prominent tenderness in the lymph nodes with or without overlying erythema. The primary source of infection may or may not be found. In these cases, empiric antibiotic therapy should be directed towards treating the most likely causative organisms, Staphylococcus aureus or Streptococcus pyogenes.
-
The primary care practitioner should evaluate for red flags that would prompt early investigations and need for specialist referral. Congenital neck masses, such as branchial cleft anomalies, may mimic lymphadenopathy and must be considered.
-
The choice of investigations is largely directed by clinical suspicion after assessment of the child. Investigations should be performed in cases of subacute or chronic lymphadenopathy, when there are associated red flags or if the child does not respond to first-line treatment. First-line investigations are FBC and CRP tests, with other tests as clinically indicated, to evaluate for more worrisome pathology.
-
An excisional biopsy of the cervical lymph node is the gold standard test for tissue diagnosis.
-
In children with acute cervical lymphadenitis, a timely re-evaluation should always be done to examine their clinical response to appropriate first-line oral antibiotics. Failure of first-line therapy should prompt the primary care provider to consider other differentials, particularly KD, for which early diagnosis is important to facilitate urgent paediatric referral and initiate appropriate, time-sensitive treatment.
-
Early intravenous antibiotics are needed in a child who looks unwell and presents with features suggestive of bacterial lymphadenitis, especially in infants and toddlers, for whom a thorough clinical assessment might be more challenging.
At her follow-up visit two weeks later, Emma had recovered fully from her recent infection and was well. As her cervical lymph nodes were stable, you planned to observe her and follow up in another four weeks. However, at the second follow-up visit, she still had non-tender, mobile cervical lymph nodes that were 2 cm in size. You ordered a full blood count and C-reactive protein test for her, which came back normal. In the absence of additional red flags, you decided to refer Emma to a paediatrician for further evaluation of persistent cervical lymphadenopathy.
SMJ-61-577.pdf


