Abstract
INTRODUCTION
This study aimed to assess understanding of the potential risks associated with medical imaging among caregivers and adolescent patients in a paediatric emergency department (PED) in Singapore.
METHODS
A prospective convenience sample survey was performed involving adolescents and caregivers presenting to our PED from December 2015 to May 2016. The questionnaire examined demographic data, knowledge of imaging procedures and radiation risks, and expectations regarding information provided about medical radiation.
RESULTS
A total of 349 questionnaires were returned (caregivers 82.5%, adolescents 17.5%). A mean of 6.2 ± 2.4 (out of 11) questions were correctly answered. Those who had tertiary education fared better than those who did not (36.4% vs. 17.2% scoring above the mean, p = 0.001). Age, gender, history of previous imaging and imaging performed during the visit did not affect the score. Two-thirds of the participants did not associate medical radiation with any negative lifetime risk of cancers or know that different scans entailed differing amounts of radiation. Most were unaware that the radiation dose in medical imaging is adjusted to a child’s size. Among patients who underwent imaging, 90.1% received explanations on the need for scans, and 26.5% were informed of the risks involved. Almost all participants wished to be informed of imaging indications and risks. More preferred to learn this from physicians (75.6%) or technicians (51.6%) rather than through educational pamphlets (34.4%) or Internet resources (22.9%).
CONCLUSION
Awareness regarding medical radiation needs to be improved in our patient population. A mismatch exists between caregiver expectations and the actual procedure of disclosure of the risk associated with radiation.
INTRODUCTION
Diagnostic imaging, particularly computed tomography (CT) and radiography, is increasingly utilised in paediatric emergency departments (PEDs) for the diagnosis and management of patients. In emergency departments (EDs), where CT is frequently utilised for the evaluation of head injury, abdominal pain and patients with polytrauma, a fivefold increase in the use of CT has been reported over the last decade.(1-3) This is of special concern, because CT involves much higher radiation doses than other diagnostic modalities, and children are more radiosensitive than adults. Hence, the potential malignancy risk associated with exposure to ionising radiation may be greater among children.
Despite the media interest in potential radiation risks from medical imaging in recent years, previous studies have shown that patients underestimate this risk.(4-6) While the majority of the studies were conducted on adult patients in a non-urgent setting in the radiology department, two of the studies were carried out in PEDs. Both studies highlighted that more than 50% of the surveyed caregivers lacked awareness regarding the long-term negative effects of medical imaging.(7,8)
In our own PED experience, we have encountered patients and caregivers who seek scans when they are not medically indicated. Meanwhile, some patients have radiation phobia and hesitate or decline diagnostic imaging owing to the perceived health risks. Hence, we sought to assess the understanding of the potential risks associated with medical imaging among caregivers and adolescent patients presenting to our PED. We also examined whether current physician practice adequately addresses the concerns of our patients and their caregivers regarding medical imaging.
To the best of our knowledge, no local study has quantified the understanding of potential malignancy risk associated with medical radiation among caregivers whose children present to the PED. Also, no previous studies have assessed the perceptions of adolescent patients (aged 12–18 years). As it is important for physicians to accurately and adequately communicate the risks and benefits of medical imaging to patients and their caregivers, knowledge of the current practice of physicians would be useful in determining whether any improvements are needed.
METHODS
This prospective cross-sectional study was performed from December 2015 to May 2016 at the PED of a tertiary university hospital in Singapore. The PED sees patients who are up to 18 years of age, with approximately 45,000 visits per year in total. This study was approved by our local institutional review board and did not receive specific grants from funding agencies in the public, commercial or not-for-profit sectors.
A convenience sample of parents/caregivers of non-critically ill children or adolescent patients (aged 12–18 years) who presented to our PED was approached for enrolment into the study. We enrolled one parent/caregiver per child. Informed consent was then obtained from those who agreed to participate. They were enrolled after completing their consultation with the treating physician. Adolescents and caregivers/parents of patients whose Patient Acuity Category Scale score was 1 were excluded. Participants who were unable to complete the questionnaire were also excluded.
The questionnaire was developed by one of the authors of this study and was based on information from the relevant literature and previously conducted studies.(4,6,8) The survey was pilot-tested on a convenience sample of 25 parents/caregivers and adolescents of varied educational and socioeconomic backgrounds to determine their comprehension level and time required to complete the survey. The questionnaire was modified in accordance with the feedback received during the pilot phase.
The final questionnaire (Appendix) comprised three sections examining (a) patient/caregiver demographic data; (b) their knowledge of radiography/CT and their associated radiation risks; and (c) their expectations of being informed about the indications of the required medical imaging and the potential radiation risks involved. In addition, they were also asked whether they had ever undergone prior medical imaging. A total of 11 questions assessed the participants’ knowledge of medical radiation and effects of ionising radiation. They could answer ‘Yes’, ‘No’ or ‘Don’t know’ to each of these questions. One mark was awarded for the correct answer and zero for the incorrect answer or if the participant did not know the answer. The maximum possible score was 11.
The questionnaire was administered by trained interviewers in English and required about 10–15 minutes to complete. When translation to Mandarin, Malay or Tamil was required, translators were used, and efforts were made to ensure that the translated version was semantically close to the original form.
Data was analysed using IBM SPSS Statistics version 23.0 (IBM Corp, Armonk, NY, USA). Descriptive statistics were used to describe patient demographics, knowledge scores and patients’/caregivers’ perception of adequate communication regarding radiation risk. Percentages were used for categorical variables, while mean and standard deviation were calculated for continuous variables. Statistical analyses were performed using chi-square tests. When the sample size requirement for the chi-square test was not met, Fisher’s exact test was used. The level of significance was set at p < 0.05.
RESULTS
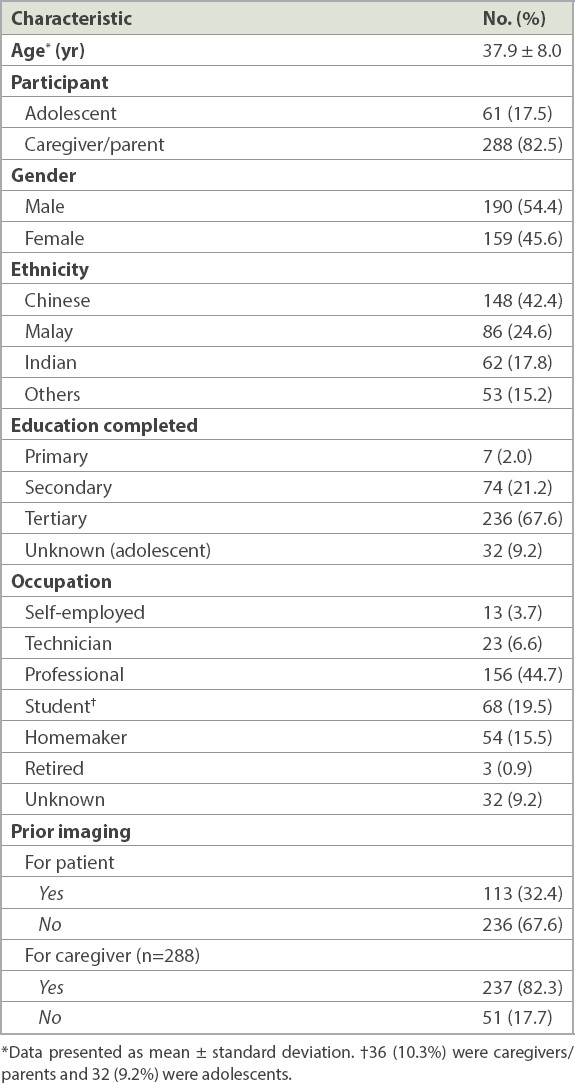
A total of 349 participants, including 288 (82.5%) parents/caregivers and 61 (17.5%) adolescents, were surveyed. A parent/caregiver was defined as an adult who accompanied the child and was the child’s parent or primary guardian. Adolescent patients referred to those between 12 and 18 years of age. The parents/caregivers had an age range of 22–67 years and a mean age of 37.9 ± 8.0 years. The mean and median age of the adolescent participants was 14.8 ± 1.5 years. 54.4% of the participants were male. 42.4% of the participants were Chinese, and the rest were Malay (24.6%), Indian (17.8%) and of other ethnicities (15.2%). The majority of the participants had completed tertiary education (67.6%), while 21.2% and 2.0% had completed secondary and primary education, respectively. 82.3% of the parents/caregivers and 32.4% of the patients reported having previously undergone imaging.
Table I
Demographic characteristics of the participants (n = 349).
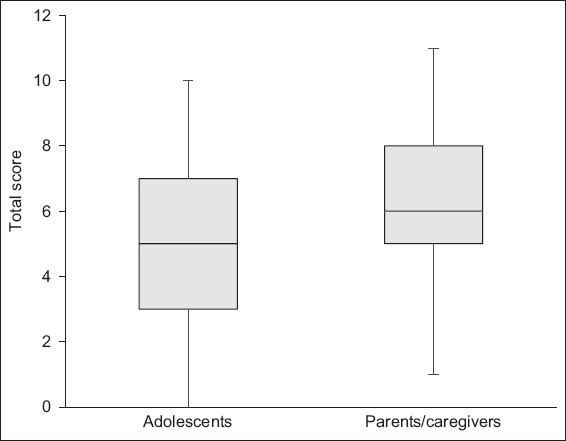
Participants were scored on their knowledge of potential malignancy risks associated with radiation exposure. The overall mean and median scores of the 349 survey respondents were 6.2 and 6.0, respectively, with a standard deviation of 2.4. The scores ranged from 0 to 11, with only 6 (1.7%) participants achieving a maximum score of 11. When the scores were analysed according to whether the participants were parents/caregivers or adolescents, the results showed that the parent/caregiver group scored better than the adolescents (6.4 ± 2.3 vs. 5.2 ± 2.6), although the difference between the groups was not statistically significant (
Fig. 1
Box and whisker plot shows the questionnaire scores of the parents/caregivers and adolescent patients.
Overall, 32.1% (95% confidence interval [CI] 27.2%–37.0%) of the participants were aware that radiography and CT could increase a child’s lifetime risk of developing malignancies (parents/caregivers 30.6% [CI 25.3%–35.9%] vs. adolescents 39.3% [CI 27.0%–51.6%], p = 0.182). Correspondingly, 40.3% (CI 34.6%–46.0%) of the parent/caregiver group was worried about the long-term negative effects of radiation exposure. By contrast, only 9.8% (CI 2.3%–17.3%) of the adolescents expressed concern (p = 0.000).
More parents/caregivers than adolescents were able to report that children were more radiosensitive than adults when exposed to medical radiation (69.8% [CI 64.5%–75.1%] vs. 32.8% [CI 21.0%–44.6%], p = 0.000). Survey scores and the proportion of participants who had knowledge of potential malignancy risks associated with medical radiation exposure were not significantly associated with age, gender, ethnicity and history of previous imaging.
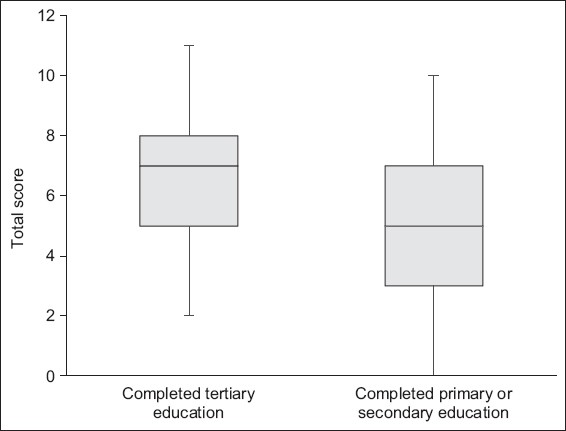
However, a positive association was observed between the education level of the participants and the scores as well as the awareness of potential malignancy risks associated with medical radiation exposure (
Fig. 2
Box and whisker plot shows the questionnaire scores based on level of formal education.
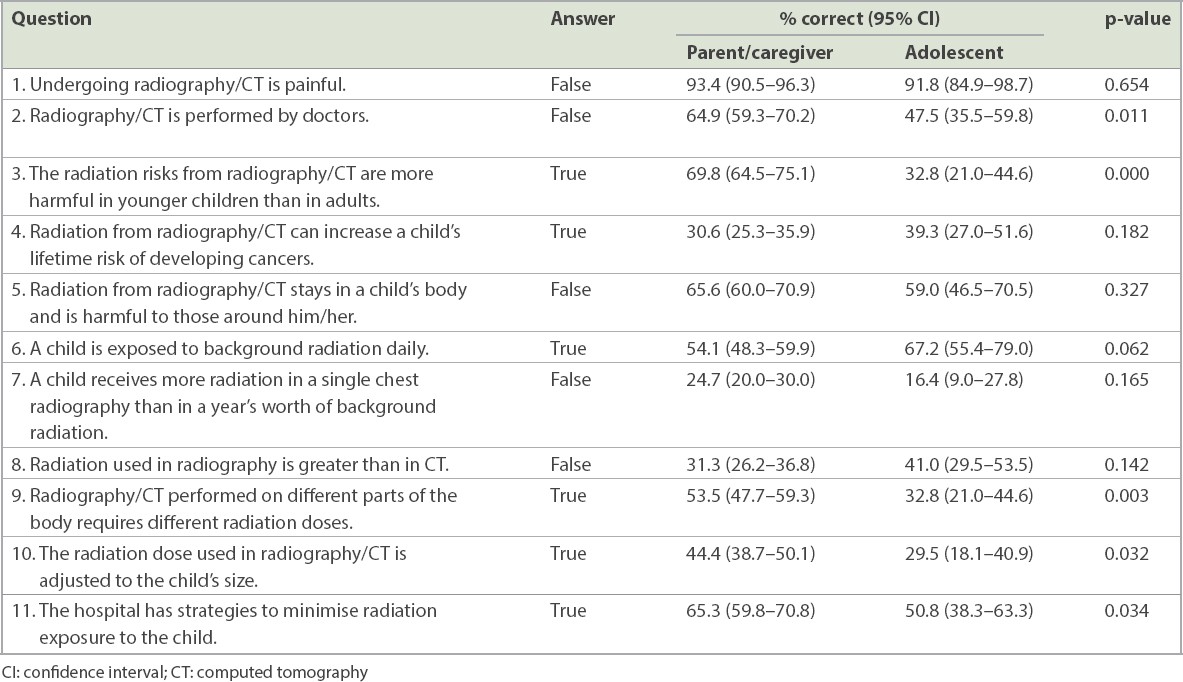
Some of the questions in the survey were directed at the participants’ understanding of radiography/CT performed in the ED. Over 90% of them correctly stated that these were not painful procedures. In the parent/caregiver group, 64.9% (CI 59.3%–70.2%) were aware that these procedures were performed by the radiographer, as compared to 47.5% (CI 35.5%–59.8%) of the adolescent patients (p = 0.011). More than half of the participants were aware that a child is exposed to background radiation daily, but less than a quarter could correctly estimate the radiation in a single paediatric chest radiograph as compared to background radiation. In addition, the majority of the participants did not know that CT involved greater radiation than radiography did. More parents/caregivers than adolescents were aware that scans performed on different parts of the body required different radiation doses (parents/caregivers 53.5% [CI 47.7%–59.3%] vs. adolescents 32.8% [CI 21.0%–44.6%], p = 0.003). While most were unaware that the radiation dose used in scans is adjusted to the child’s size, more than half of the respondents believed that the hospital had strategies in place to minimise radiation exposure to the child. More in the parent/caregiver group (65.3% [CI 59.8%–70.8%]) felt that such strategies existed, compared to 50.8% (CI 38.3%–63.3%) in the adolescent group (p = 0.034). The correct answers to the 11 true/false questions in the questionnaire and how participants performed are shown in
Table II
Performance of parents/caregivers and adolescent patients on questionnaire.
Based on the results of the questionnaire, we examined whether the treating physicians had provided adequate information regarding the indication for medical imaging and its potential radiation risks to the patients. Of the 121 patients who required imaging with radiography/CT, 90.1% stated that they were informed of the indication for the procedure, but only 26.5% were told of the risks. 99.4% and 95.7% of the participants indicated their desire to be informed about the indications and risks of the scans, respectively. In terms of expecting information about indication for the scans, there was no difference between the parent/caregiver and adolescent groups. However, 97.5% of the parents/caregivers preferred to be informed of the risks of the scans, as compared to 86.9% of the adolescents (p = 0.01). Participants’ expectations of being informed of the indications and risks of medical imaging were not affected by race, gender, ethnicity, education level or history of previous imaging.
The participants were also asked where they would like to receive information on medical imaging and its radiation risks from. They could give multiple answers. Most participants (75.6%) indicated a preference for their treating physicians to explain the information. More respondents preferred to learn it from the radiographer (51.6%) rather than the nurse (28.7%). Some preferred to learn it from educational pamphlets (34.4%) or reliable Internet resources (22.9%).
DISCUSSION
The potential association between exposure to medical radiation and cancer risk should be a topic of concern for both the patient and the physician. Two recent population studies suggested that a single CT scan increased the risk of cancer in patients.(9,10) At the same time, there is an increase in the utilisation of medical imaging in the ED, in particular CT, which is the largest contributor to diagnostic medical radiation exposure in paediatric emergency medicine.
Our findings revealed that only 30.6% of the parents/caregivers and 39.3% of the adolescent patients in our study were aware of the potential malignancy risk associated with medical radiation. This lack of awareness was more pronounced among respondents with less formal education. The majority was also unaware that CT involved greater radiation exposure than radiography.
Boutis et al(11) observed a substantial interval increase in public awareness of the potential risk associated with ionising imaging modalities over the past ten years. This was attributed to the increased media coverage and greater communication from healthcare professionals. The two studies performed in the PED setting by Boutis et al(7) and Hartwig et al(8) showed that 50% and 40%, respectively, of parents whose children presented to a tertiary care PED were aware of the long-term negative effects associated with medical imaging. Comparatively, our respondents displayed greater lack of awareness and knowledge. Only 37.1% of the respondents who needed imaging were aware of the associated risks. This is of concern, as the survey was carried out after the physician consultation, and it is assumed that the physician would have discussed the effects of imaging, giving the patient/caregiver a greater understanding of the risks involved. The physician disclosure rate was 26.5% in our study.
Our study also showed that imaging was prevalent in our study population. 82.3% of the parents/caregivers and 32.4% of the patients (mean age 7.8 ± 5.6 years) had reported having undergone previous imaging. Despite the prevalence of previous imaging, the radiation risk remains generally underestimated. A possible reason for this lack of awareness is the lack of routine discussion of imaging risks by healthcare professionals. The factors that contribute to this lack of discussion are physicians’ concern about possibly excessive parental anxiety regarding potential cancer risk and that a required scan might be denied; unnecessary delays when dealing with a critically ill child; time constraints; litigation; and the lack of easily accessible guidance on how to communicate these risks.(11) Additional barriers may be patient literacy and the fact that radiation risk is not immediately apparent.
Patients and their parents/caregivers may also underestimate the risks associated with ionising imaging, because they incorrectly assume that an investigation that is performed so frequently should not have any safety concerns. Baumann et al(4) reported that ED patients were more confident in their medical care when more testing is performed, specifically when a CT is performed. Such perceptions may result in patients and their caregivers being less receptive to information on the negative effects of ionising imaging.
Compared to the adult respondents in our study, fewer adolescents were worried about the negative effects of medical radiation. Fewer of them also wanted to be informed of the risks of medical radiation. These statistically significant findings are perhaps in keeping with the typical behaviour of adolescents, who may not fully appreciate the long-term and unseen consequences.
Our study also found that the rate of risk disclosure by our physicians did not meet the expectations of our patients and their parents/caregivers. While 95.7% of all the respondents were eager for information on radiation risks, only 26.5% of patients who needed imaging in the PED reported receiving this information. Previously published data reported that the physician disclosure rate was 24%–37% among general emergency physicians(12,13) and over 60% among paediatric emergency physicians.(14) While self-reporting surveys among physicians may inflate the results and patients’ perceptions may not always parallel those of physicians, our study shows that physicians fall short when it comes to counselling our patients regarding the potential long-term risks of radiation. In the current era of medicine, in which patient autonomy and shared decision-making are emphasised, physicians have a responsibility to discuss with their patients the benefits of acute diagnostic imaging and the potential long-term risks associated with it. By doing so, we can ensure that patients’ values and preferences are considered and patient-centred care is delivered.
As in previous studies, our respondents generally favoured obtaining radiation information from their healthcare provider rather than through written resources such as educational pamphlets and hospital-endorsed Internet sites.(6,15) Their preference is understandable, as a face-to-face dialogue allows for a more personalised discussion on individual risks instead of population risks. The majority of the respondents preferred to discuss it with their physicians, followed by radiographers. This finding supports a collaborative approach between emergency physicians and radiographers in improving patient-centred communication about imaging.
Multiple studies have consistently reported that patients and their families are eager to be informed of possible radiation risks,(13,15,16) and physicians concur that such discussions are needed.(13) However, there is also evidence that physicians have insufficient knowledge in this area, particularly non-radiology physicians.(14,17,18) To raise patients’ awareness and understanding of radiation risks, a two-pronged approach aimed at both the healthcare providers and patients is required. Equipping healthcare providers with both the necessary knowledge and skills to carry out such dialogues would be useful. Physicians may also be reassured that communicating relevant information to parents/caregivers actually increases their comfort and acceptance of radiation imaging, as seen in the study by Zavras et al.(19)
Some of the challenges faced when discussing radiation risks with patients are the limited understanding of the actual risk of cancer currently associated with medical radiation and the many other factors that can alter the risk of developing cancer. In addition, patients may find it challenging to conceptualise risk estimates. Possible strategies to overcome some of these challenges include having imaging decision aids (i.e. clinical decision rules)(20) and electronic tools that can present radiation information (i.e. radiation dose and context to risk estimates) in a simple and concise manner.(21)
Having a structured format can also facilitate the discussion. One proposal is to discuss the anticipated benefit of the scan, followed by acknowledgement that there may be a small potential future risk. This risk can be compared to other sources of radiation exposure or other risks in our everyday life. Discussions should also include information on ways to make the scans as safe as possible for patients, including measures such as dose minimisation strategies.(11)
Information on radiation risks should also be readily available to patients and their families. Apart from educational pamphlets and Internet sites, smartphone applications can also be used as alternative modalities. A study by Ukkola et al(15) found that the majority of their patients preferred symbols to indicate the radiation doses associated with imaging, and verbal or numerical scales to indicate fatal cancer risk. Use of simple, clear language and visual charts can aid their understanding. Lastly, evaluating patient understanding of the discussion is also crucial.
Our study has several limitations. First, it was conducted at a PED of a tertiary university hospital. Demographic characteristics were obtained only from participants who consented to the survey; hence, we could not compare our responder and non-responder groups, potentially limiting the generalisability of the study. Second, the nature of a convenience sample survey may have introduced sampling bias. However, the trained recruiters attempted to enrol participants of different ages, genders and ethnicity who presented to the PED on different days of the week and at different times of the day. Third, our results did not reflect the respondents’ baseline knowledge, as the survey was administered after their consult with their physician. However, as their knowledge was generally unsatisfactory even after the encounter with the physician, it would be reasonable to conclude that the findings would be similar even if the survey had been conducted without ‘physician contamination’. Fourth, although the survey used in our study was not a validated one, the questions were derived from previous studies. Lastly, an intrinsic weakness of a survey format is that respondents may have provided what they perceived to be socially desirable answers instead of their own honest perceptions.
In conclusion, we found that radiation risk awareness among our patients and their parents/caregivers and physician risk disclosure rates are unsatisfactory. Although improving patients’ knowledge and awareness may be challenging, we should aim to routinely discuss radiation risks with our patients. With education, training and practical interventions to improve our current practice, shared decision-making can become the standard when imaging is considered in the PED.
SUPPLEMENTARY MATERIAL
The Appendix is available online at https://doi.org/10.11622/smedj.2020071.


