INTRODUCTION
The geriatric population is increasing rapidly in developing countries. India and China are the main contributors to this rise in Asia.(1) It is estimated that by 2050, about 53% of the total world population aged more than 60 years will be living in these two countries.(2) In India, where there is inadequate income and no social security, older persons often find it difficult to support themselves. The impact of population ageing is already affecting India.(3) A great number of older individuals require long-term care, and the old age dependency has increased. In addition, the steady decline of the traditional support system of the joint family has put a strain on their overall health and well-being. The increasing elderly population poses a definite challenge to the country’s healthcare system. It has become essential to ensure good nutrition in older people so that they can lead an active and independent life.
Studies have shown that undernourished older people require more hospitalisation and prolonged hospital stays as compared to well-nourished individuals.(4,5) This can be prevented by early and periodic nutritional and functional assessments of the elderly population. A useful tool that is standard and validated is the Mini Nutritional Assessment (MNA).(6,7) The MNA includes six components for screening: decreased food intake; weight loss and psychological stress/acute disease in the last three months; mobility; neuropsychological problems; and body mass index (BMI). It also includes 12 components of assessment: living independently; taking more than three prescription drugs per day; pressure sores; number of daily full meals consumed; daily protein intake; daily fruit/vegetable intake; daily fluid intake; mode of feeding; self-view of nutritional status; self-perception of health status; mid-arm circumference (MAC); and mid-calf circumference (MCC). The MNA is a simple tool consisting of an easy questionnaire that only takes a few minutes to complete. In patients who have malnutrition or are at risk of malnutrition, nutritional intervention can be instituted early so as to improve quality of life.
The physical and cognitive abilities that are needed for a geriatric patient to live an independent life can be comprehensively evaluated through functional assessment. This includes evaluation of daily activities, cognition, mobility, and bladder and bowel continence. Specific tools and scales can detect moderate impairment of functional capacity in an older person, which is very significant because it may indicate the beginning of a disease. Geriatric patients have multiple problems that are often difficult to recognise clinically. Thus, structured assessment of functional status is essential in the elderly, not only for diagnosis but also for comprehensive management.(8,9) Tools available include the Barthel Index for activities of daily living (ADL), Katz Index of Independence in ADL, and instrumental ADL (IADL) scales such as the Lawton-Brody IADL scale. Additionally, muscle strength or physical performance can be measured using simple and easily available instruments such as sphygmomanometers or mechanical dynamometers. Assessing hand grip strength using a sphygmomanometer helps in identifying elderly people who are at risk of functional disability.(10,11)
There is a paucity of data regarding the nutritional and functional status of the geriatric population from the western part of India. Thus, this study was undertaken with the goal of assessing the nutritional and functional status of these geriatric patients and to find a correlation between the two, if any.
METHODS
This study was carried out at GMERS Medical College and Hospital, Gotri, Vadodara, in the state of Gujarat in western India from January to December 2017. Approval for the study was received from the Institutional Hospital Ethics Committee and the written consent of the patient or his close relative was obtained. For this cross-sectional study, all consecutive patients were enrolled to ensure an adequate representative sample.
A detailed clinical history was taken and a general and systemic physical examination was done, which was part of the protocol of the geriatric clinic. Nutritional assessment was done using the full original version of MNA tool. Data was collected from the patients using a structured valid questionnaire in the local vernacular language (Gujarati) by a qualified trained dietician and the scores were interpreted (< 17 = malnourished, 17–23.5 = at risk of malnutrition and > 23.5 = normal nutritional status). Weight, height, BMI, MAC and MCC were measured by a trained paramedical staff using the standard method to indicate the nutritional status of patients.
Functional status was assessed using the Barthel Index for ADL. The domains pertaining to self-care and mobility of daily living include continence of bowel and bladder, grooming, toilet use, feeding, transfer and mobility, dressing, ability to use stairs and bathing. Total possible scores ranged from 0 to 20, with lower scores indicating increased disability. A score of < 15 usually represents moderate disability and < 10 represents severe disability.(12)
Hand grip strength was measured by one of the study investigators using a mercury sphygmomanometer cuff. The cuff was inflated up to 20 mmHg and the patient was asked to exert maximum grip on the inflated cuff with their dominant hand (or non-dominant hand if there was any pathology on the dominant side), and the increase in pressure from baseline was recorded. This test was repeated three times and the highest of the three readings was taken as the final assessment from which the initial 20 mmHg was subtracted. The European Working Group on Sarcopenia in Older People has suggested that a grip strength of 30 kg and 20 kg for males and females, respectively, can be considered as cut-off values for low grip strength using a Jamar dynamometer. However, we used a mercury sphygmomanometer for measuring hand grip strength and hence applied the formula validated by Hamilton et al (Jamar = 0.54 × sphygmomanometer value – 45.12). We considered the grip strength of 138 mmHg and 120 mmHg for males and females, respectively, as low grip strength.(13)
Data was entered into a Microsoft Excel worksheet (Microsoft Corporation, Redmond, WA, USA) and analysed using EpiData software version 2.8.3 (EpiData Association, Odense, Denmark). The primary outcome variable for this study was the MNA score. Descriptive statistics were presented in the form of frequency and proportion. Bivariate analysis was done to find the association between sociodemographic variables and the primary outcome (MNA score) using chi-square test. The correlation coefficient (r) was calculated to find the correlation between MNA and BMI, Barthel Index score, hand grip measurement, MAC, MCC, haemoglobin and albumin values. A p-value < 0.05 was considered to be statistically significant.
RESULTS
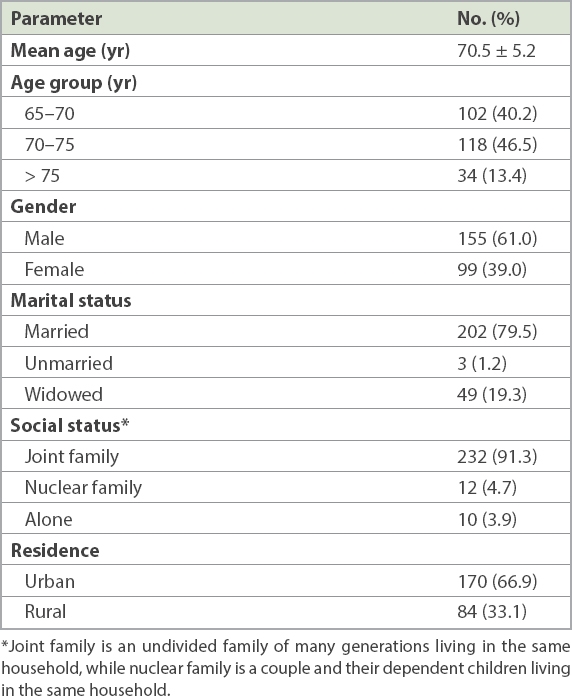
A total of 254 patients who were aged ≥ 65 years and attending the geriatric clinic in the outpatient department were included. All patients attending the clinic consented to participate and hence none were excluded.
Table I
Sociodemographic parameters of the study participants (n = 254).
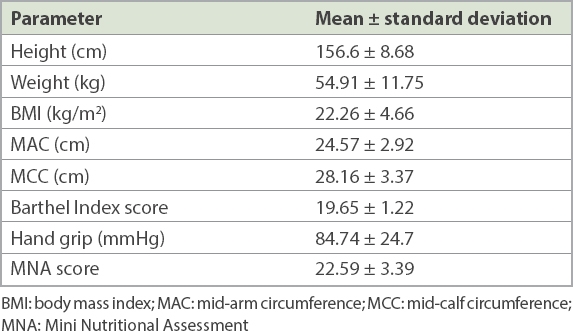
The clinical and laboratory parameters used for nutritional and functional evaluation are shown in
Table II
Clinical and laboratory parameters of the study participants (n = 254).
The nutritional status of 121 (47.6%) patients was normal (MNA score 24–30), while 124 (48.8%) patients were at risk of malnutrition (MNA score 17–23.5) and 9 (3.5%) patients were malnourished (MNA score < 17).
Table III
Association of sociodemographic factors with malnutrition or risk of malnutrition among the study population (n = 254).
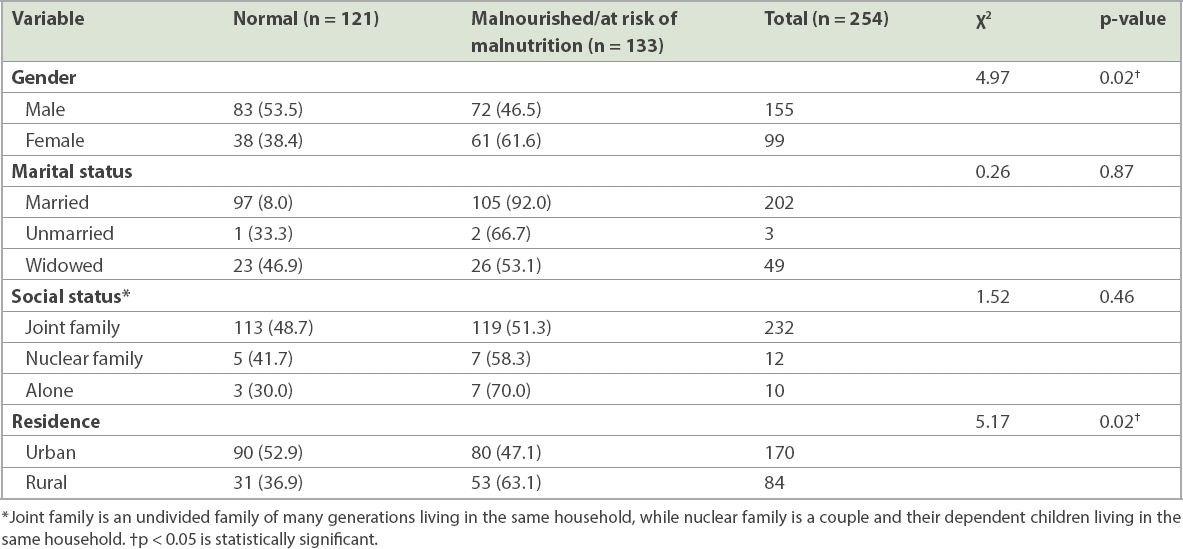
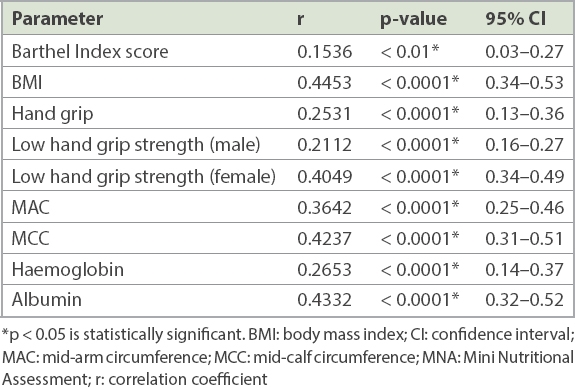
Table IV
Relationship of MNA score with other parameters among the study population (n = 254).
DISCUSSION
Malnutrition is very common in the geriatric population but often goes unnoticed. Many factors such as poor diet, poverty, psychosocial problems and chronic diseases may lead to malnutrition. Ageing also causes reduced bone mass, impaired muscle function and decreased immunity, leading to increased morbidity and decline in function status. The MNA tool is a quick and easy method to identify elderly patients at risk of malnourishment.(6,7) Such patients can be treated with the simple measures of nutritional therapy.
There have been many studies assessing the nutritional status of hospitalised or nursing home dwelling geriatric population using this tool.(3,5,14-16) In contrast, our study included patients from the community who attended the geriatric clinic of our outpatient department. Out of the 254 patients in our study, 3.5% had malnutrition, 48.8% were at risk of malnutrition and 47.6% patients were nutritionally healthy. These results also correlated with normal mean haemoglobin and serum albumin levels. This is in contrast to a study done by Paul and Abraham in a rural block of North Tamil Nadu where the prevalence of ‘at risk of malnutrition’ was only 24.4%, while 75.6% of the population had normal nutrition.(17) In their study, out of the 37 patients who were ‘at risk of malnutrition’, 17 (45.9%) were found to be anaemic, showing a positive correlation between the two. Studies by Mathew et al,(18) Lahiri et al(19) and Agarwalla et al(20) have reported a higher prevalence of malnutrition in the geriatric population, which correlates with our findings. Agarwalla et al studied the elderly population in the community setting and found that only 30% had normal nutrition, whereas a significant number (70%) were either malnourished or were at risk of malnutrition.(20)
There were 61 (61.6%) malnourished elderly female patients in our study as compared to 72 (46.5%) male patients. This is in accordance with other studies where malnutrition is more frequently found in females.(17,19-23) The association between MNA status and gender was also shown to be statistically significant. This is probably due to socioeconomic factors including gender bias and the predominant patriarchal values in Indian society, especially in rural areas. The financial dependence of females also adversely affects their nutritional status.
The majority of our study population belonged to a joint family (91.3%) with many generations of members living in the same household. Although 202 (79.5%) patients were married, no correlation was found between sociomarital status and malnutrition. Mathew et al(18) have reported a strong association between social factors such as lower economic status, single or widowed marital status, and low MNA scores. A study by Pai(24) also showed that subjects living in old age homes had lower MNA scores and BMI as compared to elderly people staying in their own homes.
We assessed the functional status of the elderly based on their ability to perform daily activities using the Barthel Index score and hand grip strength. Total possible scores for the Barthel Index ranged from 0 to 20, with lower scores indicating increased disability. The mean Barthel Index score was found to be 19.65, out of a total of 20. 33 (12.9%) patients were found to have a score of less than 20 and were considered as having some functional disability. With increasing age, there are restrictions in carrying out activities such as climbing stairs, dressing, grooming and using the toilet. The main value of applying this scale was to find patients’ level of dependence in carrying out daily activities. On reviewing the literature, for the score range of 0–100, most authors agreed on a 60/61 score as a cut-off for more-than-moderate disability. In a review by Lewis and Shaw,(25) a score of less than 14 is generally considered to indicate some disability. In our study, only 2 (0.79%) patients scored less than 14. Based on the Oxford Handbook of General Practice,(12) a score of less than 10 indicates severe disability, which was not found in our patients. Gupta et al(26) reported a 23.4% prevalence of functional disability in an elderly population from a rural area of Jhansi district of the state of Uttar Pradesh in northern India. A similarly high prevalence has been seen in studies done in West Bengal (16.16%) by Chakrabarty et al(27) and in rural South India (22%) by Venkatoraoet al.(28) The prevalence of functional disability was lower in our study as compared to these studies.
Another tool used for assessing functional capacity was measuring hand grip strength using a sphygmomanometer. Measuring hand grip strength using a sphygmomanometer or simple dynamometer is an easy and cheap screening method to predict disability in the geriatric population. It has been found that no association exists between comorbid conditions such as diabetes mellitus, neuropathy or cognitive impairment and a person’s ability to squeeze the inflated manometer cuff. Giampaoli et al(10) have reported that the prognostic value of hand grip strength measured by any dynamometer is independent of osteoarthritis, diabetes mellitus and impaired cognitive function.
A systematic review by Bohannon(29) compared 45 peer reviewed articles collected from major databases to establish the value of grip strength as a predictor of future clinical outcomes, and found that low grip strength was associated with higher chances of premature mortality, development of disability and increased risk of complications or prolonged hospital stay. Hence, grip strength measured by a dynamometer should be considered as a useful and easy method for screening older adults. With increasing age, there is a gradual loss of muscle mass known as sarcopenia. Coupled with poor nutrition, this leads to decreased strength, bone mass, impaired immune function, reduced cognition and overall increase in morbidity as well as mortality. A review article by Doherty(30) stated that in the seventh and eighth decade of life, maximum muscle strength reduces by about 20%–40%. After the age of 50 years, there is loss of lean body mass of up to 3 kg every decade. This decrease in muscular strength and muscle mass is responsible for the deterioration of physical function.(9,31,32)
By comparing MNA scores with Barthel Index scores and hand grip strength, our study showed a statistically significant positive correlation between nutritional status and functional capacity (
However, this study had certain limitations. Since it was a cross-sectional study conducted at a single centre, the findings of the study cannot be extrapolated to a larger population. In addition, the standards used for low hand grip strength cut-off were based on European guidelines (i.e. European Working Group on Sarcopenia in Older People), so low hand grip strength in Indians may have been overestimated.
In conclusion, the prevalence of malnutrition and risk of malnutrition was 3.5% and 48.8%, respectively, in our geriatric study population. It is essential to determine the nutritional and functional condition of older adults by using easy, simple and feasible screening tools to allow early intervention to take place. Those who are at risk of malnutrition can be counselled and appropriate measures can be taken to ensure good nutrition. This would help to strengthen their functional capacity and reduce morbidity. Our study shows that simple methods of nutritional functional assessment can help to detect malnutrition and risk of malnutrition in the geriatric population at an early stage.


