Abstract
Awake intubation with a flexible fibrescope is usually done electively in patients with a known difficult airway. Herein, we describe the case of an elective awake tracheal intubation that was performed on a patient with a large, obstructive supraglottic mass. The intubation was successfully performed using the Bonfils fibrescope after several failed attempts with a flexible fibrescope. This case highlights the usefulness of the Bonfils fibrescope and the limitations of the flexible fibrescope in certain clinical situations.
INTRODUCTION
Indirect laryngoscopy performed using a flexible fibreoptic laryngoscope remains the gold standard in the management of predicted difficult intubation.(1) Traditionally, awake tracheal intubation is performed using a flexible fibreoptic bronchoscope. The Bonfils Retromolar Intubation Fibrescope (
Fig. 1
Photograph shows a Bonfils Retromolar Intubation Fibrescope.

CASE REPORT
A 61-year-old man, who weighed 51 kg and had a medical history of hyperlipidaemia, presented at our institution for panendoscopy, biopsy of a supraglottic mass and tracheostomy under general anaesthesia. The patient had a three-month history of dysphagia, cough, weight loss and blood-stained saliva, for which he was initially referred to our institution’s Ear, Nose and Throat (ENT) Department. Nasendoscopy revealed a large exophytic, supraglottic lesion arising from the left pyriform sinus and extending to the right aryepiglottic fold (
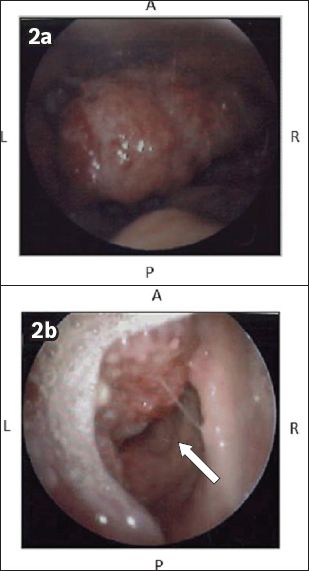
Fig. 2
Nasendoscope images show (a) the supraglottic tumour; and (b) the glottis opening (arrow).
During induction, the patient was placed in a 30° head-up position. Glycopyrrolate 200 µg, midazolam 1 mg, remifentanil infusion 0.05 µg/kg/minute and supplementary oxygen were administered via nasal prongs. Topicalisation of the airway was performed by spraying 2 mL of 10% lidocaine over the mucosa of the mouth, tongue and oropharynx. Size 5.0 microlaryngoscopy tubes were loaded onto an Olympus 4.1 mm LF-V flexible fibrescope and a Bonfils fibrescope. Initially, the flexible fibrescope was passed via the oral route with the tongue protruded. At the level of the oropharynx, the supraglottic mass, which involved the entire epiglottis, was visualised. It obscured the view of the laryngopharynx and laryngeal inlet except for a 1–2 mm opening in the right lower quadrant of the mass.
Before we attempted to manoeuvre the scope past the mass through the small opening, the mucosa was further topicalised with 2 mL of 2% lidocaine via the scope’s side port (
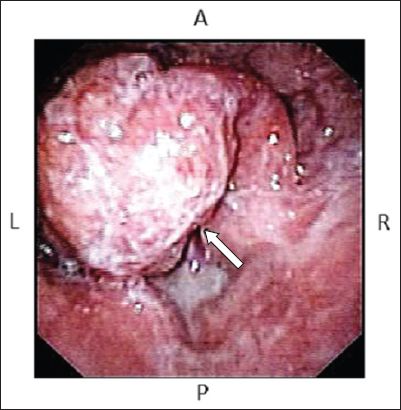
Fig. 3
Flexible fibrescopic image of the supraglottic tumour shows the small opening (arrow) in the right lower quadrant of the mass.
DISCUSSION
The Bonfils fibrescope is a 40-cm-long, straight and rigid fibrescope with an outer diameter of 5.0 mm and a fixed anterior curvature of 40° (
Fig. 4
Bonfils fibrescopic images show (a) the tumour and the small glottis opening (arrow) visualised from the right lateral approach; and (b) visible tracheal rings, the lateral margin of the tumour (arrow) and the aryepiglottic fold (arrowhead), after the Bonfils fibrescope was advanced past the tumour.
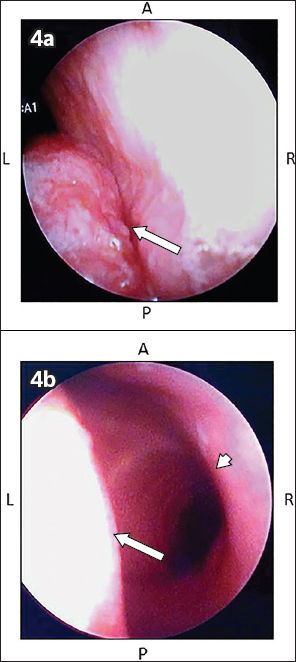
Compared to the flexible fibrescope, the Bonfils fibrescope is less expensive, easier to prepare, quicker to clean, and more portable and durable. The Bonfils fibrescope has a rigid body that is able to lift large epiglottises and push away solid tumours to gain access to the glottis. The rigid body allows for easy navigation through the oral cavity, as it is able to displace collapsed soft tissue and obstructions. Railroading the ETT with a Bonfils fibrescope is more straightforward than railroading it with a flexible fibrescope due to the distal loading of the ETT. The Bonfils fibrescope has also been effectively used in awake intubation for patients with difficult airways and/or ENT cancers. Leong and Wong previously reported the successful intubation of five patients, who had tumours that obstructed their airways, using the Bonfils fibrescope.(12) The rigidity and small diameter of the Bonfils fibrescope enables the gentle displacement of tumours obstructing the glottic opening, with minimal trauma to the tumour structure.(12) This reduces the risk of distal seeding of the tumour, as well as the bleeding and breaking off of pieces of tumour that could obstruct the airway. In addition, the Bonfils fibrescope allows manipulation with a single hand and therefore provides a more precise translation of hand movement to the tip of the scope. However, unlike the flexible fibrescope, it cannot be used for nasotracheal intubation. Newer models of the Bonfils fibrescope also do not have a working channel for accurate local anaesthetic delivery.
The flexible fibrescope is the primary airway device for managing anticipated difficult airways and awake intubation. As flexible fibrescopes are more readily available than Bonfils fibrescopes in most centres, it is expected that more anaesthetists would be trained in the use of flexible fibrescopes. However, previous surveys have shown that the flexible fibrescopy skills of anaesthetists were fairly limited.(13,14) A learning curve is expected with the training and teaching of any airway device. The Bonfils fibrescopy is considered to be more difficult to master than other types of videolaryngoscopy. The learning curve may be steep for most clinicians at the start, as its use is not readily intuitive. Some reports suggest that the learning curve improves significantly after performing 20 intubations.(15) However, the learning time for Bonfils orotracheal intubation is likely to be shorter than that for flexible fibreoptic nasotracheal intubation.(16) Nevertheless, the lack of Bonfils fibrescopes in most centres makes training with the device difficult.
The present case report demonstrates that the Bonfils fibrescope can be used effectively for awake tracheal intubation in patients with suspected or known difficult airways once competence with the device has been achieved. It also highlights the limitations of flexible fibrescopy. Bonfils fibrescopy offers advantages over flexible fibrescopy in certain situations, such as when dealing with patients who have large obstructive oropharyngeal tumours (unless nasotracheal intubation is required). In the present case, the flexible fibrescope was unable to negotiate the difficult route around the extensive airway tumour. On the other hand, the Bonfils fibrescope was able to push between the lateral margin of the tumour and the aryepiglottic fold to reach the glottic opening, with minimal trauma to the tumour and airway. When dealing with difficult airways such as the one observed in the present case, extensive airway assessment, careful planning, and a well-thought-out and thorough backup plan are paramount. The backup plan may include the use of flexible fibrescopy, Bonfils fibrescopy and/or awake tracheostomy, as well as expert assistance, airway adjuncts and readily available surgeons. In an elective situation, one should perform an atraumatic and unrushed fibreoptic examination to determine the best approach to intubate the obstructed and distorted airway. Knowledge from preoperative investigations (e.g. nasendoscopy) and careful attention to airway sounds, movements and bubbles should be used to determine the airway structures and their relation to the glottic opening. Since it is not always possible to intubate via flexible fibrescopy, Bonfils fibrescopy should be regarded as an alternative for managing patients with difficult or compromised airways.


