Abstract
INTRODUCTION
Arterial base excess is an established marker of shock and predictor of survival in trauma patients. However, venous blood is more quickly and easily obtained. This study aimed to determine if venous base excess could replace arterial base excess as a marker in trauma patients at presentation and if venous base excess is predictive of survival at 24 hours and one week.
METHODS
This was a prospective study of 394 trauma patients presenting to the emergency department of a tertiary hospital over a 17-month period. Data on base excess at presentation, vital signs, shock index (SI), injury severity score (ISS), and mortality at 24 hours and one week was collected and analysed.
RESULTS
Arterial and venous blood gas tests were performed on 260 and 134 patients, respectively. Patients were stratified into groups based on their SI and ISS for analysis. There was no statistical difference between mean venous blood gas and arterial blood gas levels at presentation when SI > 0.7, regardless of ISS (p > 0.05). The mortality rate was 4.57%. Both venous and arterial base excess was lower in nonsurvivors compared to survivors (p < 0.05). However, at 24 hours and one week, the difference in base excess values at presentation between survivors and nonsurvivors was greater when using venous base excess compared to arterial base excess (11.53 vs. 4.28 and 11.41 vs. 2.66, respectively).
CONCLUSION
In conclusion, venous base excess can replace arterial base excess in trauma patients as a means of identifying and prognosticating early shock.
INTRODUCTION
The use of vital signs alone may be inadequate in the resuscitation of trauma patients due to the presence of compensatory physiologic mechanisms in early shock. Scalea et al found that up to 80% of critically ill patients who are normotensive and have adequate urine output may remain in a state of compensated shock.(1) As such, the use of adjunctive biochemical markers of shock to assess tissue hypoxia and prevent under-resuscitation in a timelier manner has been investigated. Arterial base excess has emerged as an important marker in assessing resuscitation, as well as prognosticating trauma patients.(2-4) Numerous authors have correlated arterial base excess with ongoing haemorrhage,(5) eventual development of multiple organ failure(6,7) and mortality.(8,9)
However, venous blood is more easily obtained during the establishment of venous access, an essential early step in trauma management. Therefore, the use of venous base excess as a marker reduces the number of procedures performed in a busy trauma resuscitation. It also avoids the inherent risks of performing an arterial puncture. Venous base excess has been shown to correlate well with arterial base excess in critically ill,(10-12) mechanically-ventilated trauma(13) and acute trauma patients.(14-16) In addition, it has been suggested that venous base excess better reflects overall tissue perfusion and is therefore a better predictor of severity of shock and mortality.(17)
As it has not been established if venous base excess can replace arterial base excess in acute trauma, Schmelzer et al undertook a prospective study in 2007 that compared venous and arterial base excess values in acute trauma patients; the study found that venous base excess, but not arterial base excess, was predictive of survival at 24 hours.(4) However, correlation with survival after a longer interval was not studied.(4) The present study aimed to determine if venous base excess could replace arterial base excess in a trauma patient at presentation. We compared venous and arterial base excess values of acute trauma patients, and analysed the predictive value of venous versus arterial base excess for survival at 24 hours and one week.
METHODS
We conducted a single-centre prospective study at a tertiary hospital in Singapore with a dedicated trauma service. All acute trauma patients presenting at our institution’s emergency department between January 2009 and May 2010 were included. Trauma patients were identified based on our institution’s trauma activation criteria (
SI is defined as heart rate divided by systolic blood pressure. It has been shown to be useful in identifying early shock and correlates with mortality.(18-20) Patients were divided into groups with SIs of ≤ 0.7 (‘nonshock’ group), > 0.7 to 1 (‘early shock’ group) and > 1 (‘shock’ group) based on previous study data.(18,19,21) The ISS was developed by Baker et al in 1974 as a scalar measure of all anatomical injuries sustained during trauma.(22) It is the sum of the squares of the highest Abbreviated Injury Scale grade (developed by the Association for the Advancement of Automotive Medicine) in each of the three most severely injured body regions. The ISS has been validated to correlate with mortality and a score > 15 is defined as major trauma.(23) Patients were divided into two groups; ISS score ≤ 15 (designated as the non-major trauma group) and ISS score of > 15 (designated as the major trauma group).
The patients who had venous or arterial base excess values taken at presentation were stratified into three and two groups based on their SI and ISS scores, respectively. We compared the distribution of patients into various SI and ISS score strata in the venous base excess group versus the arterial base excess group using chi-square test. Two-sample t-tests were performed for each stratum to determine if base excess from arterial and venous samples yielded similar results. The arterial and venous base excess values of nonsurvivors versus survivors were also analysed via the two-sample t-tests to determine if either could be predictive of survival at 24 hours and one week. A p-value of < 0.05 was considered statistically significant. All analyses were performed using Stata version 10.1 (StataCorp, College Station, TX, USA).
RESULTS
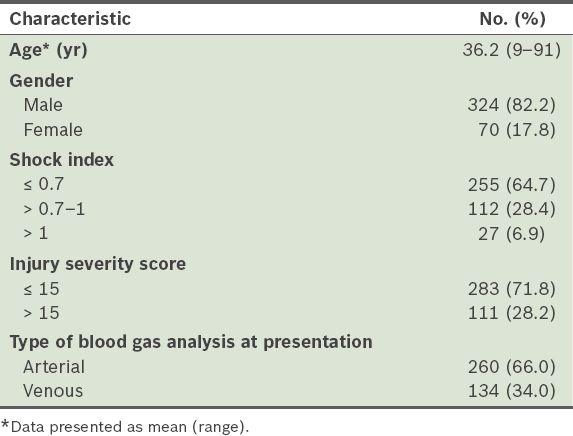
A total of 485 patients fulfilled our institution’s trauma activation criteria. Of these patients, 91 were excluded as their blood gas levels were not measured on presentation. The mean age of the patients was 36.2 years and 324 (82.2%) were men. The mean SI score was 0.720 and the mean ISS score was 10.6. Of the 394 patients finally included in the study, 134 (34.0%) had venous base excess performed on arrival, while the rest of patients had arterial base excess performed. The characteristics of the study population are summarised in
Table I
Characteristics of the trauma patients (n = 394).
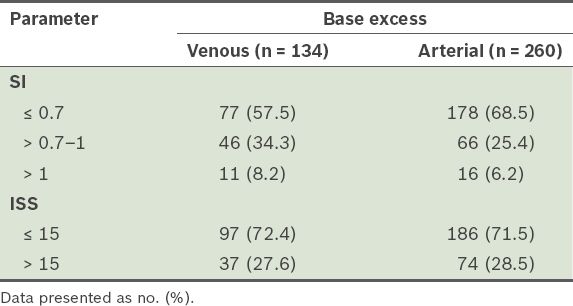
For our analysis, we stratified patients in the venous and arterial base excess groups according to their SI and ISS scores (
Table II
Venous and arterial base excess stratified by shock index (SI) and injury severity score (ISS).
We analysed the mean venous and arterial base excess groups stratified by SI (
Table III
Comparison of mean venous and arterial base excess values stratified by shock index (SI) and injury severity score (ISS).
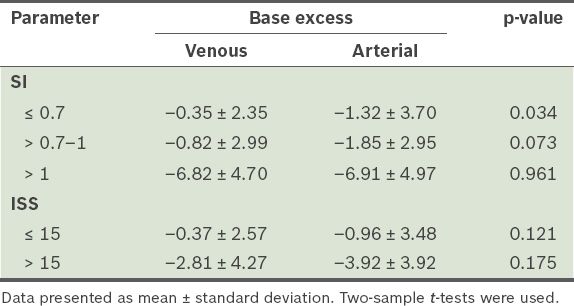
In the analysis of the data stratified by ISS, the mean venous base excess value was –0.37 in the non-major trauma group and –2.81 in the major trauma group. Comparatively, the mean arterial base excess value was –0.96 and –3.92 in the non-major and major trauma groups, respectively. The differences between mean venous and arterial base excess values in either ISS group was not statistically significant (p > 0.05,
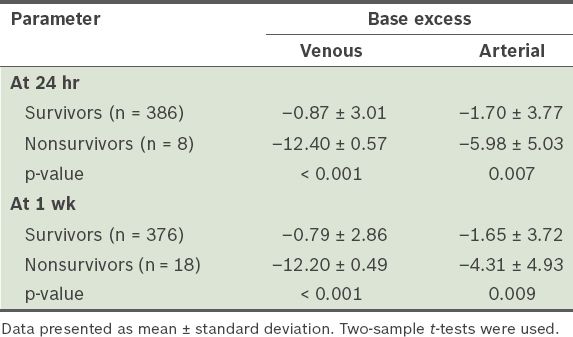
Table IV
Mean venous and arterial base excess values of the survivors and nonsurvivors (n = 394).
DISCUSSION
Many prior studies have shown that arterial and venous base excess demonstrate good correlation.(10,12,13,15,16) However, Rudkin et al(16) also pointed out that despite the good correlation between paired arterial and venous base excess values in trauma patients, the 95% limits of agreement were unacceptably wide in 20% of the patients. Our study approached this clinical question from a different angle. We compared arterial and venous base excess values between groups of patients in the same SI and ISS stratum, rather than in the same patient. This approach would aid us in identifying specific groups of patients for whom arterial and venous base excess values are interchangeable. No prior study to date has stratified trauma patients in this manner to investigate the correlation between arterial and venous base excess.
Our results show that when patients were stratified by ISS, there was no significant difference in patients’ arterial and venous base excess values within the ISS ≤ 15 and ISS > 15 groups (p > 0.05). This is the first study to suggest that venous and arterial base excess values are comparable within the different ISS stratification groups. In addition, there was no significant difference between arterial and venous base excess values when SI was > 0.7–1 (‘early shock’ group) and when SI was > 1 (‘shock’ group). However, when SI was ≤ 0.7 (‘nonshock’ group), arterial base excess showed significantly lower values than venous base excess (p = 0.034). Although venous and arterial base excess results do not appear to be comparable in this group of patients, some studies have suggested that venous base excess may be superior, as discussed below.
Arterial base excess is more widely accepted as a surrogate laboratory marker of shock in trauma patients, although there are studies that suggest that when arterial and venous base excess values do not correlate, venous base excess is a better marker of early changes in tissue perfusion. Rudkin et al proposed that this may be because postcapillary acid-base status better reflects tissue hypoperfusion.(16) Schmelzer et al(4) proposed that the lung’s ability to readily exchange carbon dioxide and oxygen might mean that arterial blood gases may not demonstrate the hypercarbia that exists in venous blood. As such, venous blood gases may better reflect tissue perfusion, while arterial blood gases better reflect the adequacy of ventilation and oxygenation.(4) In addition, Oropello et al monitored arterial and venous blood gas continuously in an animal model of haemorrhagic shock and found that changes in venous blood gas levels occurred earlier and were more significant than changes in arterial blood gas levels.(17)
Arterial base excess has been used to prognosticate trauma patients at presentation.(6-9) Therefore, this study further investigated the utility of venous base excess in comparison with arterial base excess as a predictor of mortality in trauma patients. The results show that both arterial and venous base excess values at presentation were significantly lower in nonsurvivors compared to survivors (p < 0.05) at 24 hours and one week. However, the difference was greater for venous base excess values, suggesting that venous base excess is not inferior to arterial base excess at predicting survival of trauma patients at 24 hours and one week. In concordance with the results of our study, Schmelzer et al(4) studied the survival of 100 trauma patients at 24 hours and found that while the mean venous base excess value was significantly lower in nonsurvivors than survivors (–2.9 vs. –0.3, p = 0.004), the difference in arterial base excess value was not significant.
We were unable to obtain paired arterial and venous blood gas samples from our study population. Therefore, we could not study the 95% limits of agreement between arterial and venous base excess, a statistic that was reported by other similar studies on this topic. Furthermore, the decision to have an arterial or venous blood sample taken at presentation was made at the discretion of the trauma team leader. It can be argued that this may introduce bias to our results; therefore, we performed an analysis of the proportion of patients in the SI and ISS strata to ensure that there was no significant difference in the SI and ISS of patients who had an arterial or venous blood gas sample taken.
The strength of our study is that data was collected prospectively. In comparison to similar studies on this topic, the present study included among the largest number of trauma patients and investigated the ability of venous base excess to predict survival not only at 24 hours, but also one week, which was not investigated by other similar studies.
Venous base excess shows similar results to arterial base excess in patients with more than early shock (SI > 0.7), regardless of severity of injury as measured by the ISS. It also appears to be comparable to arterial base excess in predicting mortality at both 24 hours and one week. Venous base excess may therefore be a viable alternative to arterial base excess for assessing and prognosticating trauma patients at presentation.
Supplementary Material
SMJ-57-76-Appendix.pdf


