Dear Sir,
Non-fatal drowning carries significant morbidity, mainly from concurrent hypoxic brain injury and lung injury.(1) Treatment is supportive, although a significant number of patients have refractory hypoxaemia and hypercapnia despite aggressive ventilatory support.(2) Extracorporeal membrane oxygenation (ECMO) has potential benefits for patients when mechanical ventilation is insufficient to maintain adequate gas exchange.(3) We illustrate a remarkable case of rapid recovery, despite adverse clinical and radiological prognostic factors, after early initiation of ECMO.
A 29-year-old woman was taken to the emergency department 30 minutes after she had a drowning episode in a river while alcohol-intoxicated; she fell from a height of at least 3 m, possibly hitting a boat. The duration of submersion was approximately five minutes. The patient’s pulse oximetry oxygen saturation levels (SpO2) were 88%–90%, pulse rate was 126 beats/min, respiratory rate was 20 breaths/min, blood pressure was 136/88 mmHg and temperature was 36.0°C. Her Glasgow Coma Scale (GCS) score was E1V2M1. There were bilateral crepitations in her lungs and multiple abrasions on her body. The patient was intubated and mechanically ventilated.
Chest radiographs showed bilateral infiltrates (
Fig. 1
Chest radiographs show (a) bilateral ‘white-out’ lungs from extensive consolidation at presentation to the emergency department; and (b) complete resolution of the radiological abnormalities six weeks later. CVP: central venous pressure; ECMO: extracorporeal membrane oxygenation
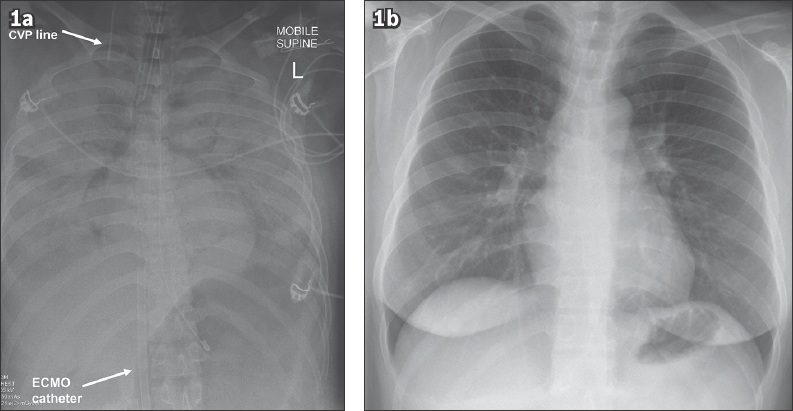
After initiation of ECMO, the patient’s SpO2 rapidly improved to 85% on Day 1 and 93%–100% thereafter. The patient made a rapid recovery, with her P/F ratio increasing from 54 mmHg before ECMO to 273.6 mmHg on Day 3 prior to explantation. Ventilator settings were set to maintain lung rest on ECMO (Day 1 pressure control ventilation: Fi 0.5, Pi 14 mmHg, PEEP 8 mmHg, achieved VT 60 mL; Day 3 pressure control ventilation: Fi 0.3, Pi 10 mmHg, PEEP 8 mmHg, achieved VT 271 mL). Serum lactate concentration also normalised from 6.5 mmol/L to 1.8 mmol/L within 18 hours of hospitalisation. The patient was progressively weaned off ECMO and explanted on Day 3, then extubated and transferred to the general ward on Day 5. She presented to the clinic six weeks later, showing complete resolution of the chest radiograph abnormalities (
ECMO is increasingly being used in drowning patients with respiratory failure refractory to ventilatory support. The speedy recovery and good outcomes of this patient were in line with the positive results seen in other studies.(3-5) ECMO should be considered early in the course of resuscitation, even if there are adverse clinical and radiological features present. Pan-CT imaging can be used to exclude concurrent physical injury prior to instituting the anticoagulation required for ECMO.
Yours sincerely,
Acknowledgement
The authors gratefully acknowledge the assistance of Dr Mariko Koh, Department of Respiratory and Critical Care Medicine, Singapore General Hospital, Singapore, for her domain expertise and contribution to the literature review.


