Mrs Lee, a 56-year-old homemaker, visited your clinic requesting for a Pap smear. Her last Pap smear had been done during a postpartum visit at the age of 35 years. Her friend had recently encouraged her to resume cervical cancer screening. Mrs Lee said that she had reached menopause two years ago and did not have any postcoital or postmenopausal bleeding.
WHAT IS CERVICAL CANCER SCREENING?
Cervical cancer screening involves tests to detect abnormal cervical cells at the pre-invasive stage (i.e. cervical pre-cancer). Early treatment can then be instituted to prevent the development of cervical cancer. Two types of cervical smears are used: high-risk human papillomavirus (HR HPV) DNA testing and the Papanicolaou (Pap) smear. The sampling procedure is the same for both; a brush is inserted into the vagina to collect exfoliated cervical cells from the surface of the cervix for testing.(1) HR HPV DNA testing looks for the presence of any of the 14 cancer-causing HPVs, while a Pap smear is a cytology-based test that looks for abnormal cervical cellular changes resulting from persistent HR HPV infection.
Cervical cancer is caused by persistent high-risk HPV infection. Out of the more than 150 types of HPVs that are currently known, 14 are linked to cervical cancer, with Type 16 and 18 causing the majority (70%) of cervical cancers worldwide.(2) HPV infection is common among young, sexually active women. A local study in 2014 showed that the highest prevalence of HPV infection was in those aged 20–24 years (26.1%).(3) However, most HPV infections are transient and will be cleared by the body without increasing the risk of cervical cancer. Studies have shown that 90% of those infected with HPV will be cleared of infection within two years from acquisition, via the host immune system. Risk factors for future cervical cancer development include increased exposure to high-risk HPV (e.g. multiple sexual partners, sexual activity at an early age) or an inability to eradicate the infection owing to an immunocompromised state.(2)
HOW RELEVANT IS THIS TO MY PRACTICE?
Singapore saw an initial decline in the incidence of cervical cancer since the introduction of the national cervical cancer screening programme in 2004. This programme was initially launched as a cytology-only-based programme, with the recommendation that all women aged 25–69 years who had ever had sexual intercourse get a Pap smear done every three years. Data has shown that a screening coverage of at least 70% is required for a screening programme to be effective.(4) However, data from 2004 to 2008 showed that only 10% of Singaporean women had their routine re-screening.(5) Over the years, despite efforts made to improve screening uptake, the latest Singapore population health survey showed that the rates still remain at a dismal 48.2%.(6) In 2013, while 64.8% of Singaporean women reported that they had done at least one Pap smear in their life,(7) this is still not ideal. This is because a single cervical screen, regardless of whether it is a Pap smear or HPV DNA test, provides protection from cervical cancer for only a limited time interval.(8) As cervical cancer develops over a long time-period of 10–20 years,(9) regular screening is the only effective way to pick up the disease early for treatment.
Currently, screening is available islandwide as part of the Screen for Life programme, in both polyclinics and general practitioner (GP) clinics under the Community Health Assist Scheme (CHAS). Screen for Life is a national screening programme that encourages Singaporean citizens and permanent residents to be screened for chronic conditions such as diabetes mellitus and certain cancers such as colorectal and cervical cancer. The CHAS scheme provides subsidised medical and dental care for Singaporean citizens at GP and dental clinics. Based on the level of subsidy, costs per cervical screening test can range from being free to SGD 5 at CHAS GP Clinics, and up to about SGD 22 at polyclinics for Singaporeans. The Singapore Cancer Society also provides free cervical cancer screening for Singaporeans aged 25 years and above at one of their centres.(1,10) Thus, screening is now highly affordable and accessible to all.
WHAT CAN I DO IN MY PRACTICE?
Cervical cancer is preventable, and prevention is achieved not just through screening but also through vaccination. As mentioned, the uptake of cervical cancer screening in Singapore has continuously been suboptimal despite various initiatives introduced by the government. One of the main barriers to screening is lack of understanding of the importance of regular cervical cancer screening. A local study cited the top reasons why Singaporean women had never gone for cervical screening: 39.4% felt that they were healthy and it was unnecessary, while 13.6% had never heard of a Pap smear test.(6) Much remains to be done to correct these misconceptions and raise awareness about screening. Additionally, the uptake of HPV vaccination is low; a study done in a Singaporean tertiary institution in 2016 showed that only 9.8% of the female students had received the HPV vaccine.(11)
Family physicians play a pivotal role in increasing the uptake of these programmes, as they are at the heart of the community and have considerable power to influence the community’s health. Preventive health is an essential part of a family physician’s job scope. In order to be effective advocates for prevention of cervical cancer, all family physicians should continuously enhance their knowledge about important aspects of cervical cancer screening and prevention, such as the role of HPV in screening and HPV vaccines. Various societies in Singapore offer continued medical education in this aspect, including the Singapore Cancer Society, Society for Colposcopy and Cervical Pathology of Singapore, and the Health Promotion Board.
HPV vaccines as primary prevention against cervical cancer
HPV vaccines are prophylactic viral-like particles designed to enhance host immunity against certain high-risk HPVs while lacking the ability to infect the host. The safety profile of HPV vaccines is well documented.(12) Currently, there are three types of HPV vaccines (bivalent, quadrivalent and nanovalent) in Singapore. All these vaccines are equally effective in protecting against the most common high-risk HPV types (Type 16 and 18). The main difference among them is the additional coverage provided (
Table I
HPV vaccines available in Singapore.
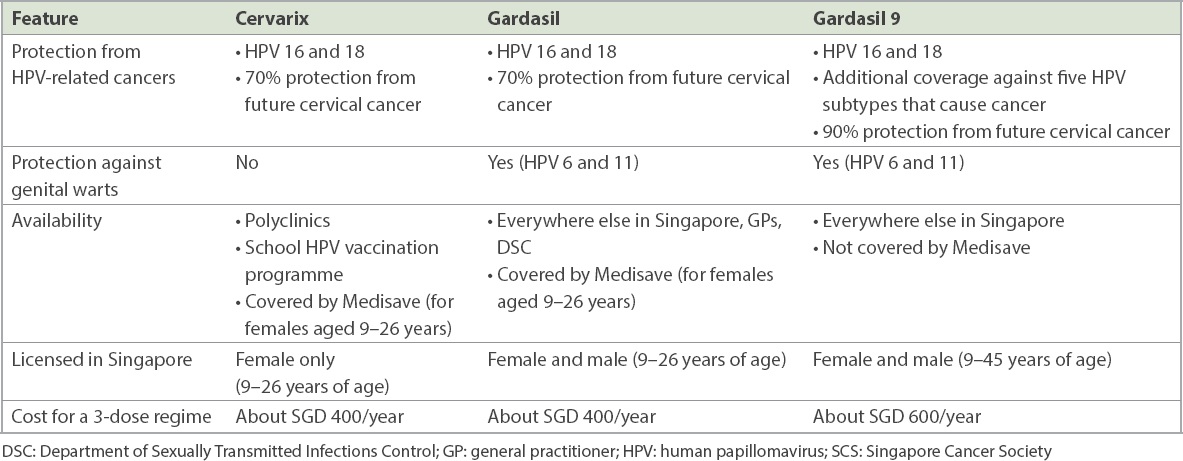
As exposure to HPV can occur during sexual intercourse,(2) it is recommended that the vaccine be given to adolescents prior to their first sexual contact. Family physicians should target these population groups when advocating for vaccination. In Singapore, HPV vaccination is licensed to be given to both men and women between the age of nine and 26 years for both the bivalent and the quadrivalent vaccines. In September 2020, the nanovalent vaccine was approved to be given to men and women up to the age of 45 years, following emerging evidence of continued protective benefits for these groups.(13,14)
In May 2019, the Ministry of Health (MOH) launched the national school HPV vaccination programme, which offers the bivalent HPV vaccine to all female Secondary 1 students. The bivalent and quadrivalent HPV vaccines are also available under Medisave coverage to all women in Singapore between the ages of nine and 26 years.
Cervical screening as secondary prevention against cervical cancer
At the same time, the MOH also launched the updated national cervical cancer screening guidelines (Cervical Screen Singapore) incorporating HPV primary screening for women aged 30 years and above.(15)
Table II
Old vs. new cervical cancer screening guidelines in Singapore.
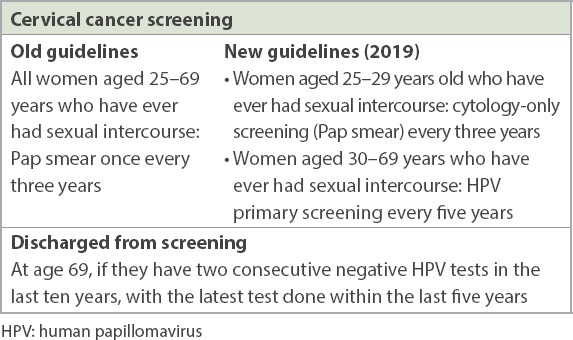
These changes in the national cervical screening guidelines were made as a response to the plethora of emerging evidence over the years regarding the superiority of HPV DNA tests compared to cytology in detecting pre-invasive cervical disease. Other benefits include the increased screening interval, providing better cost-effectiveness compared to conventional cytology screening.(16)
The guideline recommends conventional cytology screening for women aged 25–29 years rather than HPV screening. This is because a positive HPV test in this age group is not a true reflection of a woman’s risk of cervical cancer in the future. In this age group, and particularly in Singapore, where uptake of HPV vaccination is low, there is a high incidence of transient HPV infection.(3) Most women would eventually be clear of the HPV infection, without increased risk of cervical cancer in the future. Additionally, there are concerns that high rates of HPV positivity in this age group would result in an increased number of unnecessary colposcopies and invasive interventions such as cervical biopsy and colposcopy treatment. These, in turn, expose women to unnecessary physical and psychological morbidities later. Unnecessary colposcopy treatment has been shown to lead to significant future reproductive and pregnancy-related morbidities as well.(17)
Lastly, if patients have symptoms such as abnormal per vaginal bleeding or suspicious cervical lesions on speculum examination, a cervical smear is inappropriate. Such patients should be referred for further evaluation by a gynaecologist. The aim of cervical cancer screening is to detect women at high risk of pre-invasive cervical disease, and it should be done on asymptomatic women with a normal-looking cervix during speculum examination. Pre-cancer cells and HPV infection do not present with any symptoms and are invisible to the naked eye; screening is the only way to detect their presence.
Interpretation of results
This section serves to complement the local cervical cancer screening guidelines through interpreting the various possible results and explaining the rationale for subsequent steps. The following are some updates on cytology-only screening.
-
Patients who show NILM (negative for intraepithelial lesion and malignancy) and absent endocervical cells no longer need to have an annual Pap smear but should return to routine screening. This is because the absence of endocervical cells is not associated with increased risk of pre-invasive cervical disease.(18)
-
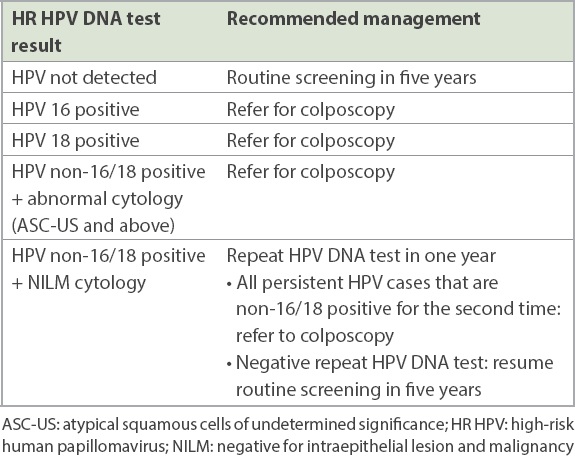
Those who show ASC-US (atypical squamous cells of undetermined significance) no longer need a repeat Pap smear in six months. If cytology shows ASC-US, the laboratory will automatically perform an HPV DNA test on the original sample. If HPV negative, the woman returns to routine screening. If HPV positive, the patient should be referred for colposcopy.
-
If NILM is present and endometrial cells are seen, the guideline varies based on age. The age cut-off for referral to a gynaecologist has now been raised from 40 years to 45 years. As many women aged 40–45 years still have menstrual cycles, benign endometrial cells on Pap smear in this age group do not correlate with significant pathology.(19) However, if the woman is aged below 45 years and has any positive risk factors (abnormal vaginal bleeding, chronic anovulation, family history of endometrial cancer), she should also be referred to a gynaecologist for risk assessment of endometrial cancer.
Screening for special populations is not within the scope of this article. These include immunosuppressed women, post-hysterectomy patients and patients with previous abnormal results. More details can be found in the 2019 cervical screening guidelines.(15)
WHEN SHOULD I REFER TO A SPECIALIST?
Tables
Table III
A guide to management of cytology (Pap smear) results.
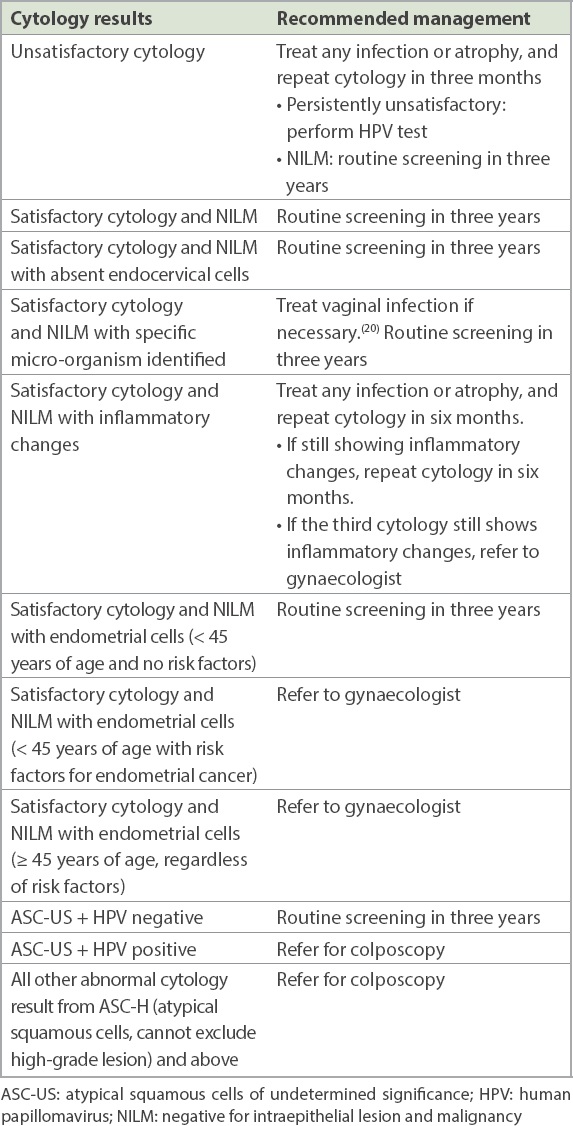
Table IV
A guide to management of HR HPV DNA test results.
TAKE HOME MESSAGES
-
Cervical cancer is highly preventable through both screening and vaccination.
-
Screening uptake is the most important factor for a successful cervical cancer screening programme. Uptake in Singapore is still suboptimal, and primary care physicians have a vital role to play in promoting understanding and uptake of screening in the local community.
-
It is important for primary care physicians to be familiar with the appropriate tests and relevant intervals for cervical cancer screening, especially with the introduction of HR HPV testing in the latest guidelines.
-
Primary care physicians should know how to interpret screening results and the subsequent steps, including indications for a gynaecology referral.
-
Preventive health goes hand in hand with screening. Primary care physicians should be familiar with the various HPV vaccinations available and advocate vaccination for those in the relevant age groups.
As Mrs Lee was in the 30–69-year age group, you performed a high-risk human papillomavirus (HPV) test for her, which was negative. You also reminded her to take another HPV test in five years’ time. She felt reassured and thanked you for your time. She wanted to bring her 24-year-old daughter to see you to discuss HPV vaccination.
SMJ-63-129.pdf


