INTRODUCTION
Long-term use of acid-suppressing drugs has led to recent concerns about gastric structural and functional changes.(1) It has been reported that the prevalence of fundic gland polyps and enterochromaffin-like cells increased after long-term proton pump inhibitor (PPI) therapy.(1) PPIs, developed in the 1980s, have been widely used for the treatment of acid-related disorders. PPIs are frequently used for long-term maintenance therapy of patients with gastro-oesophageal reflux disease (GERD) and long-term use of low-dose aspirin for cardiovascular disease or non-steroidal anti-inflammatory drugs for arthropathy. The administration of PPIs is continuously increasing worldwide, and the long-term safety of acid-suppressing agents is important. Vonoprazan (VPZ), a potassium-competitive acid blocker, was first available in 2015. VPZ is widely used for the long-term treatment of GERD and Helicobacter pylori (H. pylori) eradication therapy.(2,3) VPZ blocks H+-K+ exchange in gastric parietal cells competitively and reversibly, resulting in superior acid suppression to that afforded by PPIs.(4)
The long-term use of PPIs is associated with various gastric mucosal lesions such as fundic gland polyps, gastric hyperplastic polyps, multiple white elevated lesions and cobblestone-like mucosa.(5,6) There are no reports about the influence of long-term VPZ use, compared to PPIs, on the morphological changes of gastric mucosa, despite its strong acid suppression and the increasing use of VPZ. There is concern that the stronger acid suppression effect of VPZ may lead to more gastric morphological changes than those caused by PPIs. Clarification of the morphological changes due to VPZ or PPI use facilitates risk estimation and helps to clarify the benefits of their long-term use. This study aimed to investigate gastric morphological changes during long-term acid suppression therapy using VPZ compared to PPIs and histamine-2 receptor antagonists (H2RAs).
METHODS
This retrospective observational study was based on endoscopic findings and medical records. The inclusion criterion was having undergone oesophagogastroduodenoscopy (EGD) between November 2018 and November 2019 at the Shinozaki Medical Clinic, Utsunomiya, Japan. The exclusion criteria were: (a) receiving acid suppression therapy for less than one year in patients currently treated with acid-suppressing drug; (b) current H. pylori infection; and (c) prior oesophageal or gastric surgery. When multiple EGDs were performed on one patient during the study period, we included only the first EGD. At our clinic, we always try to identify all medications that a patient is taking before EGD by checking their personal ‘medicine notebook’ issued by the Japan Pharmaceutical Association, which documents all prescriptions for the patient regardless of the prescribing facility. Therefore, we confirmed the one-year administration of acid-suppression drugs by reviewing both the medical records and the ‘medicine notebook’.
We used ultrathin endoscopes including EG-L580NW7, EG-580NW and EG-580NW2 (Fujifilm Corporation, Tokyo, Japan). We began using an endoscopic system for linked colour imaging in March 2019. Endoscopic reporting included the grade of gastric atrophy and the presence or absence of fundic gland polyps, gastric hyperplastic polyps, multiple white elevated lesions (
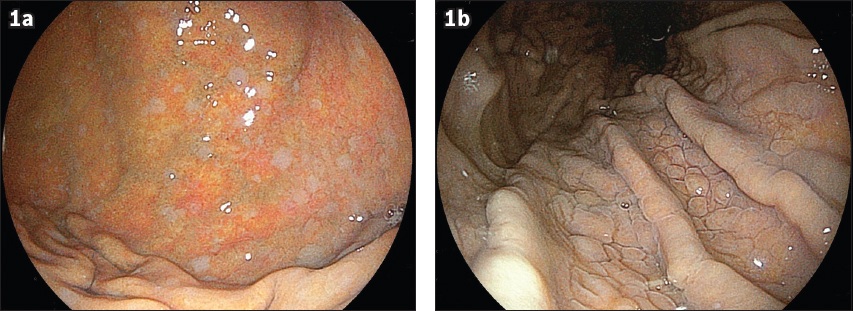
Fig. 1
Endoscopic images show (a) multiple white elevated lesions and (b) cobblestone-like mucosa using linked colour imaging.
Medical records and endoscopic reports were retrospectively reviewed. The use of acid-suppressing medications including VPZ, PPI and H2RA was investigated. When endoscopic findings were unclear, we reviewed the endoscopic images and videos. The Institutional Review Board approved this retrospective review.
The frequency of gastric lesions was compared between the groups using chi-square test. To reduce the influence of confounding factors, we performed univariate and multivariate logistic regression analysis. We selected factors for multivariate analysis based on clinical significance. StatFlex software version 7.0 (Artech Co Ltd, Osaka, Japan) was used to perform these analyses. Differences were considered significant when p < 0.05.
RESULTS
During this period, 1111 patients underwent EGD. A total of 106 patients were excluded from the study for the following reasons: H. pylori positive status (n = 57), acid suppression therapy for less than one year in patients currently being treated with an acid-suppressing drug (n = 26) and a history of gastric surgery (n = 23). Consequently, 1,005 patients were included in the final analysis, where 441 patients received acid-suppression therapy using VPZ, PPI or H2RA, and 564 patients in the control group did not.
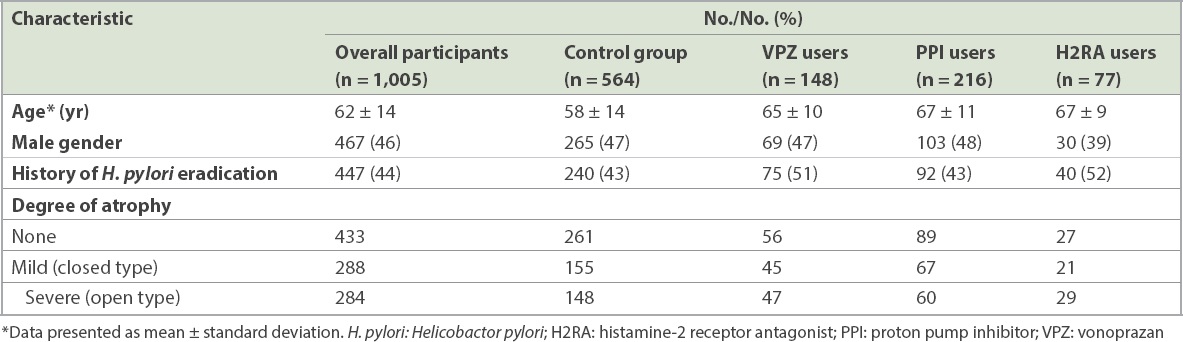
Indications for EGD in the remaining 1,005 patients included screening (n = 911), investigation of abdominal symptoms (n = 75), investigation of an abnormality on an upper gastrointestinal series (n = 12), investigation of anaemia (n = 4) and observation of known lesions (n = 3). Almost half of the patients underwent acid-suppressing therapy for more than one year (n = 441, 44%) and had a history of H. pylori eradication therapy (n = 447, 44%) (
Table I
Baseline characteristics of patients (n = 1,005).
The overall prevalence of fundic gland polyps was 30% (n = 303). The prevalence in the PPI group was significantly higher than that in the control, VPZ and H2RA groups (
Fig. 2
Charts show the prevalence of gastric lesions in (a) fundic gland polyps; (b) gastric hyperplastic polyps; (c) multiple white elevated lesions; and (d) cobblestone-like mucosa. All differences among groups were evaluated, but only statistically significant results are described. H2RA: histamine-2 receptor antagonist; PPI: proton pump inhibitor; VPZ: vonoprazan
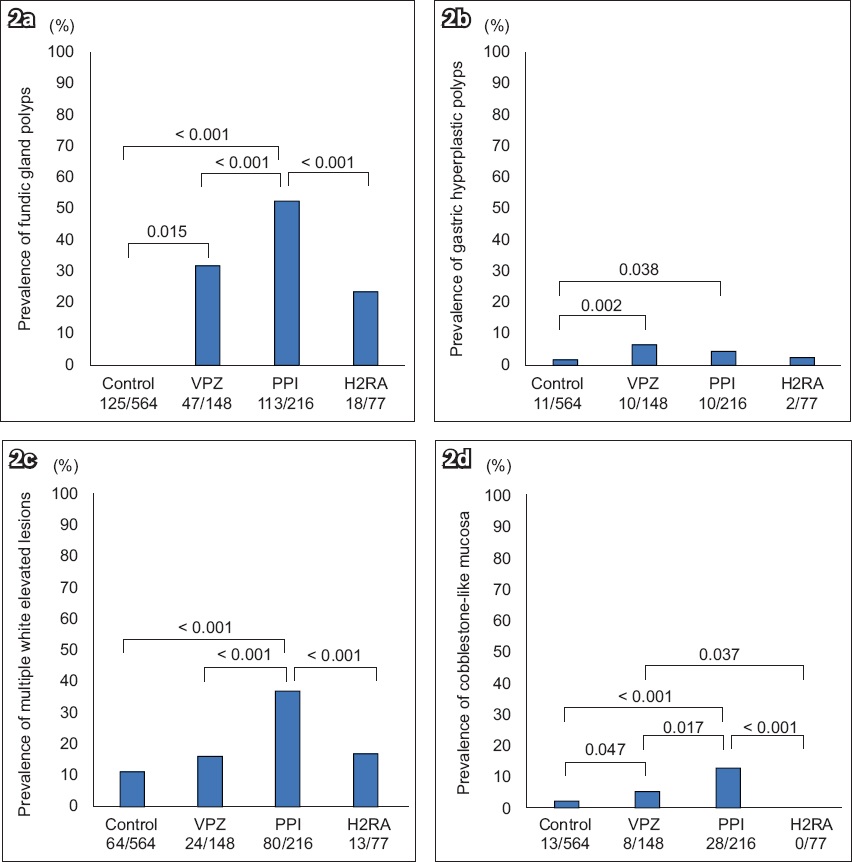
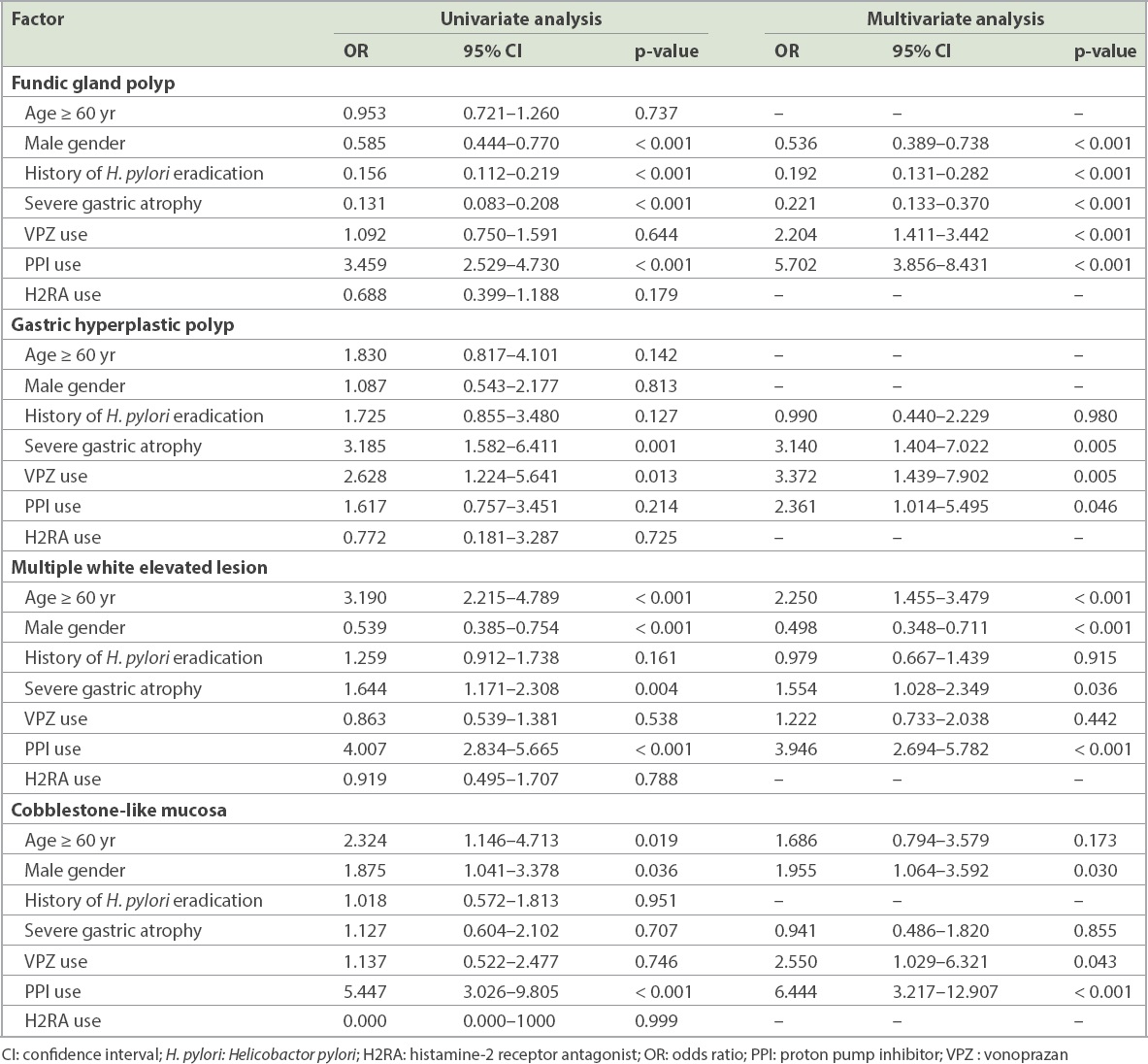
Table II
Presence of factors associated with gastric lesions.
The overall prevalence of gastric hyperplastic polyps was 3% (n = 33). The prevalence in the VPZ and PPI groups was significantly higher than that in the control group (
The overall prevalence of multiple white elevated lesions was 18% (n = 181). The prevalence in the PPI group was significantly higher than in the control, VPZ and H2RA groups (
The overall prevalence of cobblestone-like mucosa was 5% (n = 49). The prevalence in the PPI group was significantly higher than that in the control, VPZ and H2RA groups (
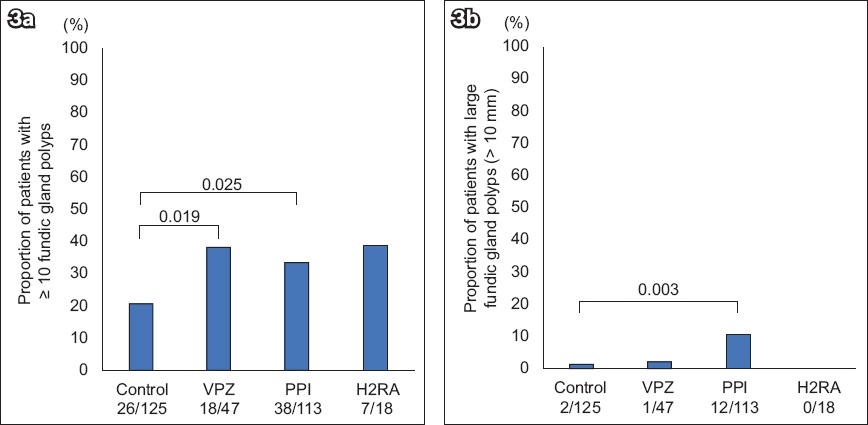
The number and size of fundic gland polyps in the 303 patients with fundic gland polyps were investigated. First, we evaluated the number of patients with ten or more fundic gland polyps in each group (
Fig. 3
Charts show the proportion of patients with (a) ≥ 10 fundic gland polyps; and (b) large fundic gland polyps (≥ 10 mm). All differences among groups were evaluated, but only statistically significant results are described. H2RA: histamine-2 receptor antagonist; PPI: proton pump inhibitor; VPZ: vonoprazan
DISCUSSION
This retrospective study reports gastric morphological changes in patients with long-term acid-suppressing agents, including VPZ. Long-term VPZ use increases the prevalence of fundic gland polyps, gastric hyperplastic polyps and cobblestone-like mucosa, and long-term PPI use increases the prevalence of fundic gland polyps, gastric hyperplastic polyps, multiple white elevated lesions and cobblestone-like mucosa. Long-term VPZ or PPI use also increases the number of fundic gland polyps per patient. This is the first study reporting gastric morphological changes after long-term use of VPZ.
A systematic review reported a clear association between long-term PPI use and the prevalence of fundic gland polyps.(11) The malignant potential of fundic gland polyps is negligible.(12) The mechanism of fundic gland polyp formation due to long-term PPI therapy is characterised by the development of cystic gland dilation (fundic gland cysts) and parietal cell hyperplasia.(12) A 6% frequency of new fundic gland polyps after one year of PPI use has been reported,(13) and the incidence of fundic gland polyps is proportional to the duration of PPI use.(12) This study demonstrates that long-term use of VPZ increases the number of fundic gland polyps in each patient. Considering the strong acid-suppressing effect of VPZ, it is reasonable that long-term VPZ use also increases the prevalence of fundic gland polyps, similar to PPI.
The relationship between long-term PPI use and the prevalence of gastric hyperplastic polyps has not been clearly reported. The increased likelihood of gastric hyperplastic polyps in PPI users was reported in a Japanese study that included as many as 42% of H. pylori-infected individuals.(5) The development of new gastric hyperplastic polyps one year after starting rabeprazole was 4% in a Japanese prospective study, including 41% of H. pylori-infected individuals.(13) Undoubtedly, the development of gastric hyperplastic polyps is strongly associated with H. pylori-positive status.(14) The present study excluded H. pylori-positive individuals to diminish any bias incurred owing to the influence of H. pylori-associated active inflammation. As a result, the prevalence of gastric hyperplastic polyps in the VPZ group was similar to that in the PPI group.
Multiple white elevated lesions are frequently observed in patients with long-term use of acid-suppressing drugs and are characterised by hyperplastic changes in the foveolar epithelium and parietal cell protrusions.(6) An association between the presence of multiple white elevated lesions and PPI use has been reported.(5,6,15) The high frequency of female gender and advanced age in patients with the morphological changes in the present study is consistent with previous Japanese studies.(5,9,15) Among healthy individuals, postprandial gastrin levels in women are two- to three-fold higher than in men.(16) During GERD therapy with PPIs, women also have higher gastrin levels compared to men.(17) This persistently higher level of gastrin in women compared to men may influence the prevalence of multiple white elevated lesions as well as fundic gland polyps.
Cobblestone-like mucosa is a phenotype of gastric mucosal hyperplasia and is strongly associated with PPI use.(10) Its pathological characteristics are parietal cell hyperplasia/protrusions and cystic dilation of fundic glands.(18) Serum gastrin concentration is not related to the presence of cobblestone gastric mucosa.(18) In the present study, cobblestone-like mucosa is strongly associated with long-term use of VPZ and PPIs and is more frequently seen in men than in women. Interestingly, the male preponderance of cobblestone-like mucosa is consistent with the results of a recent Japanese study(5) but shows an inverse result compared to the female preponderance of multiple white elevated lesions. Further studies are necessary to clarify the mechanism of this morphological change.
We acknowledge that this study has some limitations. First, this is a retrospective observational study. Second, the duration of the use of acid-suppressing medications was not uniform. As the VPZ group might include patients who had a history of previous PPI use, long-term PPI use before taking VPZ could have contributed to the observed gastric morphological changes, which would not be solely due to VPZ alone. The duration of PPI therapy may have been longer than treatment with VPZ, which was released fairly recently in 2015. Although we made efforts to obtain a complete medication history based on the ‘medicine notebook’, which is widely used by patients in Japan, there could be missing information regarding previous use of acid-suppressing medications in the control group. Third, previous chronic H. pylori infection in patients with a history of eradication might cause morphological changes. Fourth, the endoscopist was not blinded to the use of acid-suppressor medications or reports of previous endoscopic evaluations. Linked colour imaging may facilitate the detection of morphological changes. Fifth, the key morphological findings were not confirmed by biopsy and the decision was dependent on the endoscopist.
There are also some important strengths to this study. First, the definition of long-term use of acid-suppressing drugs was more than one year for all patients. Second, only H. pylori-negative individuals were included. Third, the number of VPZ or PPI users was large.
In conclusion, this is the first report of morphological changes during long-term VPZ therapy involving a large number of patients. We found that the prevalence of fundic gland polyps, gastric hyperplastic polyps and cobblestone-like mucosa was significantly associated with VPZ as well as PPI use. It is important to be aware of gastric morphological changes in long-term VPZ and PPI users.
ACKNOWLEDGEMENTS
Authors Shinozaki S, Osawa H and Miura Y received honoraria from Takeda Pharmaceutical Company and Otsuka Pharmaceuticals. Authors Hayashi Y, Sakamoto H and Yamamoto H received honoraria from Takeda Pharmaceutical Company. All other authors declare no conflicts of interest regarding this study. The funding source had no role in the design, practice or analysis of this study.


