Abstract
The last 15 years have seen changing patterns of injury in emergency surgery and trauma patients. The ability to diagnose, treat and manage these patients nonoperatively has led to a decline in interest in trauma surgery as a career. In addition, healthcare systems face multiple challenges, including limited resources, an ageing population and increasing subspecialisation of medical care, while maintaining government-directed standards and managing public expectations. In the West, these challenges have led to the emergence of a new subspecialty, ‘acute care surgery’, with some models of care providing dedicated acute surgical units or separating acute and elective streams with the existing manpower resources. The outcomes for emergency surgery patients and efficiency gains are promising. In Singapore, Khoo Teck Puat Hospital has implemented its first dedicated acute surgical unit. This article outlines the evolution of acute care surgery and its relevance to Asia.
INTRODUCTION
The care of critically ill patients suffering from a wide spectrum of disease and trauma remains the foundation of general surgery (GS) practice. Emergency surgery and trauma (ESAT) patients provide a consistent and demanding workload, and public hospitals are expected to deliver high-quality care with limited resources. Demands on the healthcare system require dynamic models reflected in government policies and hospital planning. At the department level, workforce and skill distribution must answer the challenge presented by ESAT patients, to ensure the best possible outcomes for this vulnerable group.
The longstanding GS model of acute care requires surgeons to cover ESAT while maintaining output for the core elective disciplines of upper gastrointestinal, hepatobiliary, colorectal, breast and endocrine surgeries. As a consequence, it is not uncommon for emergency cases to be performed after hours or by unsupervised juniors. Trainee surgeons who provide care ‘at the coalface’ are increasingly subspecialty-oriented, and with the pressures of the worldwide push to reduce hours for junior doctors, limited case opportunities and competition for positions, a consultant’s ESAT work is becoming an afterthought. With the retirement of experienced older surgeons, the era of the master acute care general surgeon who was prepared to operate on any body cavity is rapidly coming to an end.(1)
Hospital management is guided by adherence to productivity and disease-specific guidelines, often dictated by health ministries. However, assessing productivity in the care of acute surgical patients beyond the emergency department (ED) is more challenging, reflecting the heterogeneous age of presentation, complexity of comorbidities, and multiple diagnoses and operative strategies. Furthermore, funding arrangements heavily favour elective surgical targets. A diminished emphasis on acute surgical patients may be a source of ongoing inefficiency and reduced quality of care. A nationwide study into the impact of emergency GS admissions across the United States (US) showed that 7% of all hospital admissions were acute surgical patients and the annual case rate per 100,000 population was found to be greater than the sum of all new cancer diagnoses. Although this significant workload is expected to increase, precious little airtime has been afforded in public health debates for the allocation of resources, healthcare access and studies into overall health improvements.(2)
THE EVOLUTION OF ACUTE CARE SURGERY
In the 1960s, trauma morbidity and mortality were identified as the “neglected disease of modern society”.(3) In response, numerous accomplishments were achieved; these included changes in prehospital care and paramedic training, development of emergency management systems and standardised approaches to trauma patients, which are now commonplace worldwide.(4) A landmark study showed that the consequence of such system development in Level I trauma centres is a significant reduction in trauma-related mortality.(5)
However, the last 15 years have seen the rise of new challenges that put the future of trauma surgery in question. These include the emergence of new interventional radiology techniques that reduced the need for operations, as well as a notable increase in elderly and non-penetrating traumas.(6) This epidemiological change has resulted in a declining operative experience for GS residents over time and calls into question their desire to commit to a full-time career in trauma surgery.(7,8) Such an ‘identity crisis’ in trauma surgery led the American Association for the Surgery of Trauma to search for future strategies, leading to the birth of a new subspecialty, ‘acute care surgery’ (ACS).(9,10) ACS needed to address the impending crisis, be viable and produce an attractive lifestyle.(4) The product of this vision, ‘the acute care surgeon’, is a subspecialist in the provision of ESAT and critical care. This American model of care has reinvigorated the management of ESAT patients. A major accomplishment is the creation of a dedicated curriculum at the fellowship level that is offered at many Level I trauma centres and has the recognition of the American Board of Surgery.(4) Other signs of the increasing recognition of ACS include the renaming of the Journal of Trauma to the Journal of Trauma and Acute Care Surgery and the publication of the first textbook on acute surgery.(11,12)
Outside of the US, however, critical care is predominantly practised by anaesthetists and considered a subspecialty in its own right. A report from 27 European centres showed that ACS is not formally recognised as a subspecialty; instead, ESAT patients may be managed by ‘all-rounders’ who specialise in general surgery and orthopaedics.(13) In the United Kingdom (UK), the Royal College of Surgeons has identified a need for change, citing the greater complexity of acute cases with higher bed occupancy and mortality rates, as well as the increasing subspecialisation of surgeons.(14) Planned changes include the prioritisation of acutely ill patients over electives, consultant-led services and a greater focus on outcome-driven care.(14) Reorganisation of manpower to allow for dedicated acute surgical units or subspecialists to access emergency rosters is now being implemented in the UK and Finland.(15,16)
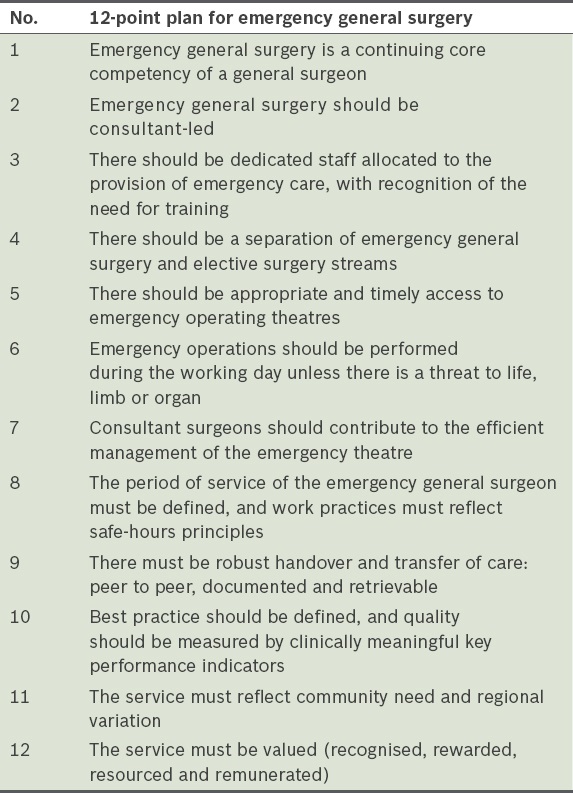
Australia and New Zealand have been the most proactive in adopting ACS models. General Surgeons Australia (GSA) has published a 12-point plan that highlights the key features of an acute surgical service (
OUTCOMES IN ACUTE SURGICAL MODELS
Measurements of the success of acute care models have focused on system efficiency and patient-centred outcomes. Several studies have reported reductions in time to surgery and complication rates, particularly for common conditions such as appendicitis and cholecystitis.(20,21) A recent meta-analysis showed improved timeliness of care and fewer appendicectomies performed after hours.(22) For cholecystitis patients, a reduction in conversion rate and a 40% increase in index-presentation cholecystectomies were noted.(22) The productivity of the department as a whole also improved, with greater utilisation of the theatre and intensive care unit (ICU), as well as increased throughput for elective surgery via redistribution of manpower.(23) Two studies have shown reductions in time to review in the ED from 2.4 hours to 1.6 hours, and 3.2 hours to 2.1 hours, respectively.(24,25) Furthermore, multiple studies have shown reductions in time to operation.(26,27) Lehane et al also reported a reduction in length of stay (LOS) from a median of six days to four.(28) In the US, a report utilising the national inpatient sample database (130,000 patients) showed that emergency general surgical patients in ACS trauma units had lower LOS, complications and costs compared to those in standard care units.(29) Such improvements could have resulted from better infrastructure, as acute care teams have shown better communication and continuity of care.(29) In a review of Australasian acute surgical units, Page et al showed that various models have resulted in reductions in after-hours operating, increases in inhouse operating or teaching, and greater consultant presence in the theatre.(30) The benefits of having ready access to senior surgical input can only improve teaching and learning opportunities for trainees. A systematic review of eight different acute models across Australia, New Zealand and the UK reported wide variations in compliance with the GSA’s 12-point plan. Key points covered by all units included consultant-led and consultant-available services, separation of acute and elective commitments, increased operations during daytime hours, acute theatre under the control of an acute surgeon, handover protocols, and units that reflect community need and variance.(19)
The ACS model has many workflow benefits. The acute team is more efficient in reviewing ED or ward-based crises, especially in the era of government-based waiting time targets. Faster diagnosis and earlier commencement of management plans can only lead to improved outcomes. Ward-based interdisciplinary reviews, surgical advice to other teams and the ability to discuss urgent cases with the radiology department, ED or ICU via direct consultant-to-consultant communication also improve the delivery of care. The concept of waiting for the ‘consultant review’ on the next day needs to be consigned to history.
ACUTE CARE SURGERY IN SINGAPORE
The literature pertaining to the pressure to improve the delivery of ESAT care and benefits of ACS models has originated from Western healthcare systems. Justifiably, one may question whether Singapore or the wider Asian ESAT models of care need to move with the times. In Singapore, the delivery of ESAT care follows the traditional pathways. However, it would be naïve to believe that the constraints of funding limitations, an ageing population, limited resources and availability of human capital are not relevant here. Furthermore, GS teams face on a daily basis the pressures of senior staff availability, clashes with elective surgery and endoscopy units, appropriate supervision of junior staff and timely review of ESAT patients. Local data has shown improved efficiency for index presentation laparoscopic cholecystectomies, and surgical leaders have identified the need for surgical systems to keep adapting, particularly in regard to training.(31,32) Three of the largest hospitals (National University Hospital, Singapore General Hospital and Tan Tock Seng Hospital) have established trauma rosters, identifying the need to separate elective and acute workflow streams based on senior clinician interests and subspecialty skill sets.
Khoo Teck Puat Hospital (KTPH) is the first hospital in Singapore to set up a dedicated acute surgical unit. Established in November 2014, the ESAT team involved a significant redistribution of workload within the department. The aims of this consultant-led team are to separate elective and acute workloads, improve efficiency within the system and standardise care of ESAT patients. A consequence for the other subspecialty teams may be an increase in workflow for elective cases, clinics and endoscopy.
The key features of the team are:
-
All admissions and ward-based referrals are seen by the ESAT team from Monday to Friday, 7.30 am to 4.00 pm.
-
The team consists of one consultant, one associate consultant, one trainee registrar, two medical officers (MOs) and three house officers.
-
After-hours and weekend on-call schedule remains the same, as per a typical GS acute roster.
-
Each morning, a handover is performed to discuss the new admissions after 4.00 pm. Consultant-to-consultant discussions determine the predisposition of the patient, who is either admitted under ESAT or stays with the original team. The Monday morning handover includes discussion of any weekend patients.
-
At 2.00 pm, a consultant-driven paper round is held to discuss all patients and a ward round of the new admissions is then conducted.
-
Attempts are made to perform as many acute GS cases as possible during the daytime.
-
Consultant-driven supervision and training of registrar and MOs is conducted in the theatre, and in trauma and ward-based emergencies.
-
Acute endoscopy is split between an on-call team and the ESAT team.
-
There are no other clinical responsibilities for the ESAT surgeon other than management of inpatient GS acute and trauma patients.
Preliminary data for the first two months showed that 65% of all acute admissions and blue letters were under the new ESAT team; this averaged out to approximately 20 patients reviewed per day. Major operative cases, including laparoscopic cholecystectomy, laparotomy (bowel resection, adhesiolysis and trauma) and acute hernia repair, comprised 30% of the workload, and the consultant was present in the theatre for all cases. The rest of the operative cases consisted of surgery for soft tissue infections and appendicitis. The average times from booking of cases to operation were 256 minutes for appendicitis, 258 minutes for cholecystitis and 480 minutes for abscess drainage. Time from ED referral to being seen by the surgical team was 90 minutes. There was a trend toward reduction in nighttime surgery, with 41% of cases performed after 4.00 pm compared to 59% in the two months prior to the commencement of the ESAT unit; similar LOS and costs were shown when these two groups were compared. This data will be corroborated in a larger study of ESAT team productivity comparing the old and new systems.
Assessment of the new ESAT team according to the GSA’s 12-point plan shows compliance with many of the key features. It is a consultant-led service with dedicated junior staff attached to the team. There is greater separation between elective and acute care, with timely access to the theatre, although it is currently not a dedicated GS theatre. Although the handover processes are new to the hospital, they are robust and easily managed among the surgeons, with ongoing analysis of outcomes measured based on key performance indicators.
The ESAT team must function seamlessly within the GS department, and this requires cooperation and goodwill among the surgeons. Patients who require specialist colorectal, upper gastrointestinal, hepatobiliary or endocrine surgical reviews are appropriately referred to these services. Some nuances must be built into the model; these include retention of patients previously operated on by other teams, the requirement that the ESAT surgeon be available for after-hours patient crises and recognition of the individual on-call surgeon’s patient preferences. New concepts introduced by this model, such as robust handover between clinicians and consistent team access by the ED, theatre and ICU staff, are all designed to improve workflow efficiency and potentially achieve better outcomes for patients.
Although it is required of ACS models, a dedicated acute theatre for GS has not been achieved in our centre. However, close communication between theatre staff and the ESAT surgeon allows for prioritisation of cases for the day and discussion of alternative arrangements when the system is under pressure. Redistribution of workload requires adequate manpower, and our current team is sufficient to review 20 patients daily (ED, ward and blue letters). It is vital that there are sufficient junior staff numbers to prevent fatigue as they divide their day between ED acute admissions, ward patients and the theatre. The benefit of four months of dedicated acute work for a GS resident is clear. So far, the residents have given very positive feedback in terms of improved confidence, clinical abilities and surgical decision-making, all monitored in real time by the ESAT surgeon.
Beyond the establishment of one service, broader questions remain to be answered. Who should participate in ESAT services? Should the model be inclusive, such that all surgeons are encouraged to participate, or exclusive, such that only dedicated ESAT surgeons run the service? What level of competency should ESAT surgeons have? Should they have exposure to subspecialty elective surgery to maintain competency to operate on diverse anatomical regions? A two-year ACS fellowship in the US covers critical care and attachments in all major subspecialties, including thoracic, vascular, orthopaedic, neurosurgical and burns units.(4) In Singapore, how can we train and incentivise registrars to show interest in ESAT as a worthwhile career, or will it just be a transitional service before they settle into subspecialty elective work? As models of care adapt and change to reflect the separation of elective and acute workloads, one would expect some trainees to show aptitude and interest in ESAT as a career.
CONCLUSION
Healthcare systems worldwide are adapting to the ongoing challenges of limited resources and ageing populations. The delivery of consistent, high-quality care to ESAT patients, who represent a significant workload in GS, is the target of ACS models, particularly in Western countries. Recognising the universality of these healthcare pressures, Singapore hospitals are now considering models of care that separate acute and elective workflows. Although the new ESAT model in KTPH is only in its infancy, it represents a positive step toward addressing some of these issues. Further quantitative and qualitative data to assess both patient outcome and system efficiency is required before its full impact can be understood.