The Critical Haemorrhage to Operation Room Patient (CHOP) protocol was designed for Khoo Teck Puat Hospital (KTPH), Singapore, to facilitate recognition, escalation and mobilisation of resources in the context of major trauma, with the goal of bringing a severely injured patient rapidly to definitive care. It targets critically injured trauma patients who have, or are assumed to have, ongoing or potentially massive haemorrhage. These patients have the potential for rapid and devastating deterioration and require access to early definitive care by a multidisciplinary trauma team.(1-3)
The hospital receives an average of 1,200 trauma patients per year, of which 350 are Tier 1 or severely injured patients, making KTPH the centre with the second highest volume of Tier 1 trauma cases in Singapore. The mechanism of trauma for these patients is mainly blunt trauma secondary to road traffic accidents or falls from a height. The hurdles that the trauma team faces in bringing a patient to early definitive care include balancing the immediate need for resuscitation, logistical coordination with the various specialists and mobilisation of appropriate resources – all of which necessarily occur in a high-stress situation. This is made more challenging, as our audits have shown, because less than a third of these patients presented during office hours when a dedicated trauma team is present to facilitate the above.
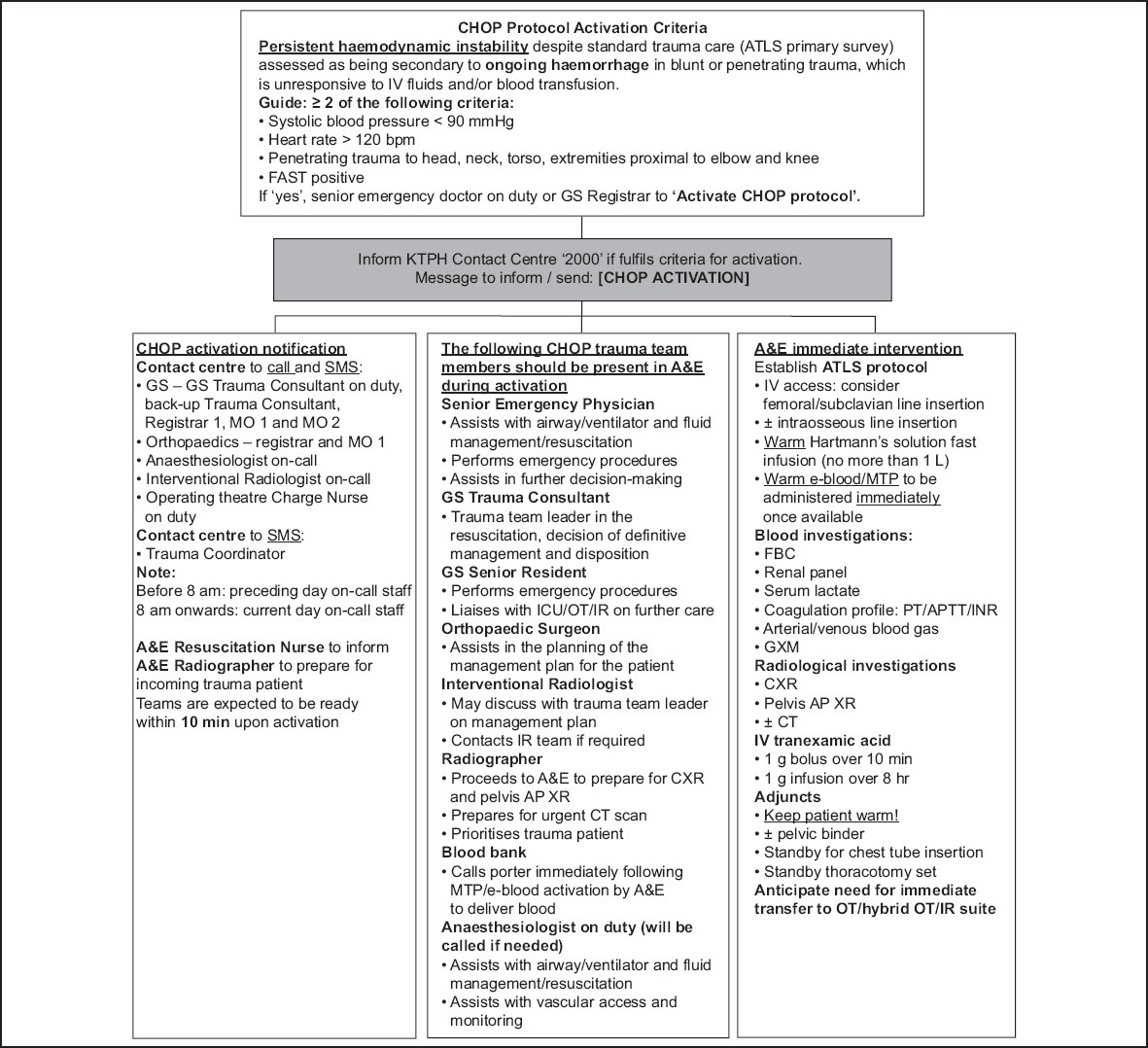
The CHOP protocol acts to facilitate second-tier activation for a subset of severely injured trauma patients who meet two out of four criteria that are suggestive of active or massive exsanguination: (a) systolic blood pressure (SBP) < 90 mmHg; (b) heart rate > 120 beats per minute (bpm); (c) penetrating injuries to the head, neck, torso or proximal extremities; and (d) positive FAST (focused abdominal sonography in trauma) imaging indicating intra-abdominal or intra-thoracic free fluid. These simple guidelines are based on the Assessment of Blood Consumption Score,(4) which is validated to predict the need for a massive transfusion protocol. The trauma team may also choose to activate the CHOP protocol for patients who do not fulfil the above criteria but have progressive haemodynamic instability, or who are found to have injuries requiring immediate surgical intervention or angioembolisation.
The second-tier activation kicks off an automated chain of calls from the hospital switchboard to these additional on-call specialists: (a) a general surgery consultant; (b) an anaesthesiologist/intensivist; (c) an interventional radiology consultant, with an additional step to inform; and (d) a backup trauma general surgery consultant, if necessary. It also enables the mobilisation of resources, such as activating the operating theatre (OT) sister to put the OT staff on standby and the blood bank to send two packs of uncrossmatched E-blood immediately to the resuscitation area.
The need for second-tier activation for critically injured patients is not a novel concept. The advent of various protocols, such as Code Crimson in Westmead Hospital, Australia,(5) and Code Red in Royal London Hospital, United Kingdom,(6) have integrated themselves into the management of trauma. However, there has been no equivalent protocol introduced in Singapore yet. The CHOP protocol seeks to fill that role within the local context – taking into account a patient pool that consists mainly of blunt trauma cases – where interventional radiology procedures have taken a step up in importance for minimally invasive procedures, such as embolisation of pelvic vessels.
The CHOP protocol was first implemented in KTPH in March 2018. It blends seamlessly with the pre-existing trauma activation guidelines and Advanced Trauma Life Support protocol to boost efficiency. The key outcome of the CHOP protocol is for definitive care to be initiated within 90 minutes of CHOP activation.
Fig. 1
Flowchart shows the workflow for activation of the Critical Haemorrhage to Operation Room Patient (CHOP) protocol. A&E: Accident and Emergency Department; AP: anteroposterior; ATLS: Advanced Trauma Life Support; CT: computed tomography; CXR: chest radiography; GS: General Surgery; FAST: face, arm, speech test; FBC: full blood count; ICU: intensive care unit; IR: interventional radiology; IV: intravenous; KTPH: Khoo Teck Puat Hospital; MO: medical officer; MTP: massive transfusion protocol; OT: operating theatre; PT/APTT/INR: prothrombin time/activated partial thromboplastin time/international normalised ratio; SMS: short message; XR: radiography
The initial experience of the first ten patients covered by the CHOP protocol is described in
Table I
Initial experience under the CHOP protocol (n = 10).
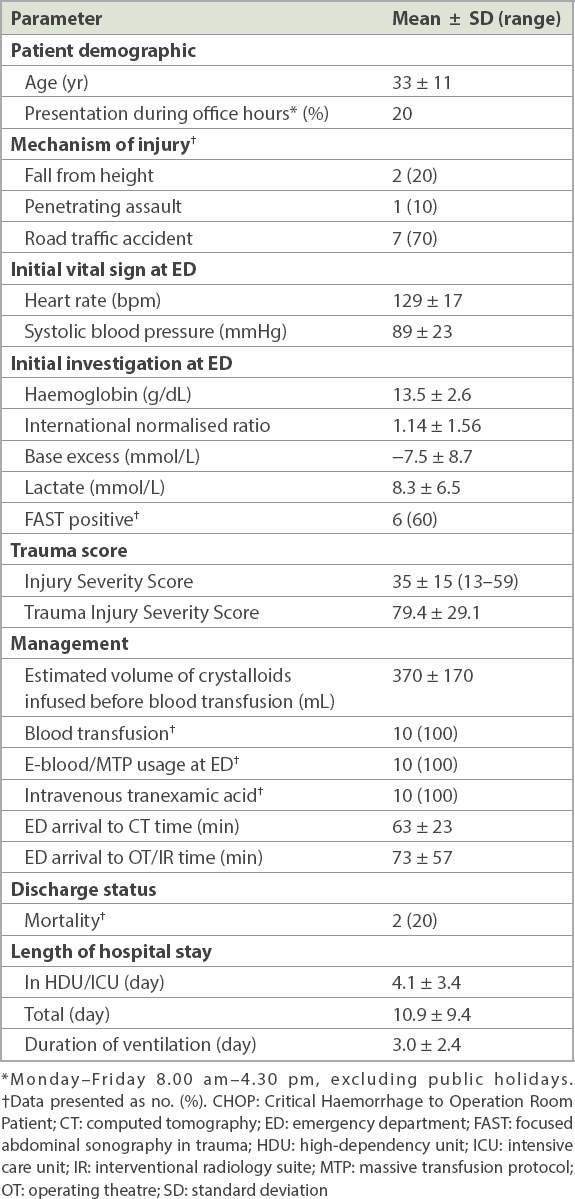
Early analysis of outcomes in these first ten cases of CHOP activation shows that the target (i.e. access to definitive intervention within 90 minutes) was achieved overall, with an average time of 73 minutes from arrival at the emergency department to transfer to the OT or interventional radiology suite. Upon briefing, the two cases that showed a delay to intervention of more than 90 minutes were noted to have the following contributory factors: delay in activation of CHOP protocol and unfamiliarity with the CHOP protocol. These issues were addressed subsequently with multidisciplinary briefings and simulations to familiarise key members of the trauma teams with the new protocol and availability of resources.
Subsequent outcomes showed a mean length of stay of 4.1 days in intensive care and a mortality rate of 20%. Both cases of mortality had an ISS of 50 and presented with high likelihood of a non-salvageable pattern of injury, as evident from TRISS scores of 17.5 and 36.4, respectively.
In conclusion, the early experience of the CHOP protocol in KTPH shows that second-tier activation enables the multidisciplinary trauma team to be deployed to provide early definitive intervention for Tier 1 trauma patients. The CHOP protocol, the first of its kind in the local context, has integrated itself with the trauma workflow of our hospital and become an essential part of the pathway to promptly direct critically injured patients to the best possible care.


