Abstract
Our sleep-wake cycle is determined by the interaction between our homeostatic sleep drive and circadian rhythm. Each of us has a personalised biological rhythm or chronotype that determines the optimal time to fall asleep and wake up. Chronic sleep deprivation has been linked to the development of several physical and mental health disorders, as well as accidents and occupational errors. Around the world, growing recognition of the importance of sleep has led to the adoption of practices that promote sleep health. Given that Singaporeans were consistently found to be one of the most sleep-deprived populations in the world, we believe that there is an urgent need to pursue the introduction of community-based sleep health interventions here. This includes sleep education and promotion of sleep hygiene, adopting practices to reduce social jetlag and improve sleep health, and enhancing screening and treatment of sleep disorders.
INTRODUCTION
Virtually all of us are innately cognisant of the importance of sleep. However, the daily sleep-wake cycles of many individuals are no longer driven by the light and dark cycle, but by work schedules, economic interests and increasing globalisation. With multiple role demands and expectations, sleep is often considered an expendable luxury. This article aims to inform the reader about human chronobiology, the importance of sleep and the consequences of sleep deprivation. We also discuss and examine possible sleep health interventions in the community, including the role of the primary care physician.
HUMAN CHRONOBIOLOGY
The human sleep-wake cycle is determined by the homeostatic sleep drive and the circadian rhythm.(1) The interaction between these two processes has been conceptualised in the ‘two-process model of sleep’.(2,3) The homeostatic process (Process S) involves an increasing sleep drive that accumulates during our waking hours and dissipates during sleep. The circadian rhythm (Process C) is an internal biological clock that regulates our subjective alertness, performance levels, core body temperature and hormonal rhythms, such as that of cortisol. The major circadian pacemaker in humans is the suprachiasmatic nucleus (SCN) in the hypothalamus of the brain. The SCN relies on a combination of internal and external cues for its rhythm. Light exposure is the primary external cue, or zeitgeber,(4) for this circadian pacemaker. The circadian regulation of sleep creates a drive for wakefulness during the day, which then declines at night.(5,6) Each of us has a personalised biological rhythm or chronotype that determines the optimal time to fall asleep and wake up.
SLEEP AND SLEEP HEALTH
In recent decades, increased research into sleep medicine has resulted in greater awareness and understanding of the effects of sleep on both physical and mental health. Sleep serves several important functions. It helps to maintain cognitive functions, such as attention, processing speed, executive function and memory.(7-9) Sleep plays a role in the maintenance of the immune system(10) and also encourages body restoration,(11) growth and repair. It is also believed that sleep clears the brain of metabolic waste via the glymphatic system.(12) With sleep being recognised as being crucial to good health, researchers have begun to define the term ‘sleep health’. According to Buysse,(13) sleep health is a ‘multidimensional pattern of sleep-wakefulness, adapted to individual, social and environmental demands, that promotes physical and mental well-being’. Buysse characterised good sleep health by the presence of ‘subjective sleep satisfaction, appropriate sleep timing, adequate sleep duration, high sleep efficiency and sustained alertness during waking hours’.
ADVERSE EFFECTS OF SLEEP DEPRIVATION
The importance of sleep is also illustrated through the consequences of sleep deprivation. It is now well-known that sleep deprivation, apart from affecting physiological activity, can also affect mental functions.(14) A study on the effect of sleep disruption showed that disrupted sleep is associated with DNA damage, which has been linked to the development of chronic medical diseases.(15) Chronic sleep deprivation has been linked to hypertension,(16,17) diabetes mellitus,(18) hyperlipidaemia,(16,19) obesity, and cardiovascular and cerebrovascular diseases.(20) Long-standing sleep deprivation can contribute to emotional dysregulation and the development of mental disorders.(21) For children and adolescents, studies have shown that inadequate or poor quality sleep in early childhood impairs socio-emotional and cognitive function via effects on the developing brain.(22,23) There has also been greater appreciation of the complex and bidirectional relationship between psychiatric disorders and sleep, in place of the traditional view that disordered sleep is merely a symptom of psychiatric disorders. Insomnia has been recognised as a risk factor for depression, anxiety and suicide.(24-26) Sleep deprivation is also a well-known trigger for manic episodes in bipolar patients.(27) In recognition of this, the International Society for Bipolar Disorders announced in 2019 that it has set up a Chronobiology Task Force to study the relationship between chronobiology and bipolar illness.(28) A recent population-based study in Singapore(29) found that poor sleep quality combined with short sleep duration (less than six hours a day) was associated with a higher chance of having any physical disorder and several mental disorders, such as major depressive disorder, bipolar disorder, generalised anxiety disorder and obsessive compulsive disorder.
Sleep deprivation has been linked to increased occupational errors,(30) industrial accidents(31,32) and motor vehicle accidents.(33-35) This is likely a result of impaired attention, slowed reaction times and impaired judgement that follow lack of sleep. Chronic sleep deprivation has also been associated with increased work absenteeism.(36,37) Hence, it is clear that chronic sleep deprivation is also a public health burden that can incur significant direct and indirect healthcare costs.
SLEEP HEALTH INTERVENTIONS IN THE COMMUNITY
As the world becomes more aware of chronobiology and the importance of sleep, some places in the world have started to introduce changes to school and work schedules in order to better align them to the natural human sleep-wake cycle. Bad Kissingen, a town in Germany, has set a goal to become the first ‘Chrono-City’ in the world.(38) Its residents have managed to weave the principles of chronobiology into their daily life. Schools start later in the day and businesses are encouraged to offer flexitime. This allows people to work and study when they feel at their best. In the United States, researchers from the University of Minnesota observed an improvement in school attendance, as well as in students’ engagement, focus and motivation, after delaying the start time for several high schools.(38) The medical fraternity has also started to take notice. In 2014, the American Academy of Pediatrics issued a position statement that supported a school starting time of 8.30 am or later.(39) This was followed by a similar recommendation by the American Academy of Sleep Medicine (AASM) in 2017.(40) In 2015, the AASM and the National Sleep Foundation also updated their recommended daily sleep duration, which differs across age groups: 7−9 hours for adults, 8−10 hours for teenagers, 9−11 hours for children aged 6−13 years, and 10−13 hours for children aged 3−5 years.(41,42)
Singaporeans have been consistently found to be one of the most sleep-deprived populations in the world.(43,44) A 2016 study on 350 individuals in Singapore showed that 44% of them had inadequate sleep (less than seven hours) on weekdays and 26% of them had inadequate sleep (less than seven hours) on weekends.(45) Given the evidence-based adverse effects of sleep deprivation on physical and mental health, we believe there is an urgent need to pursue the introduction of community-based sleep health interventions in Singapore. This would include sleep education and promotion of sleep hygiene, adopting practices that reduce social jetlag and improve sleep health, and enhancing screening and treatment of sleep disorders.
Educate the public about sleep and promote sleep hygiene
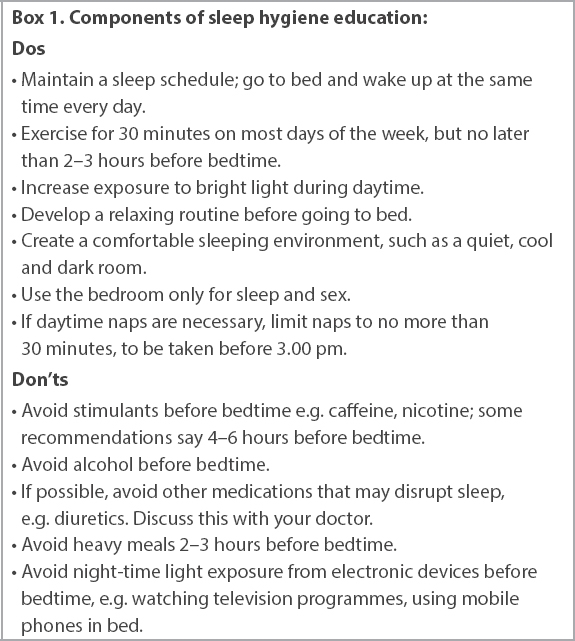
Public education about the human chronobiology and the importance of sleep is required to foster a paradigm shift in the community’s stance on sleep. This is especially important in Singapore, home to one of the world’s most competitive economies,(46) where an ‘always-on’ culture is pervasive and seen as highly desirable. A nationwide health promotion drive providing information on the benefits of sleep, as well as the negative consequences of sleep deprivation on physical and mental health, could help to raise awareness among the general population. Promotion of sleep hygiene could also improve sleep among the population. Sleep hygiene includes a variety of habits and practices that are necessary to have a good night’s sleep and daytime alertness, such as maintaining a regular sleep schedule, having a relaxing routine before going to bed, avoiding heavy meals near bedtime and avoiding excessive light stimulation before bedtime. Nocturnal exposure to blue-wavelength light emitted from multimedia screens has the ability to modify our circadian rhythm and sleep.(47-50) The widespread use of portable electronic devices, such as smartphones and handheld tablets, in the bedroom has been associated with sleep problems such as later bedtimes,(51) shorter sleep duration,(51-54) longer sleep latency(52,55) and reduced sleep efficiency.(56) Given that the majority of Singaporeans own a smartphone or a handheld tablet,(57) public education and the promotion of healthy screen habits could help to improve sleep hygiene and sleep health in the population. The components of sleep hygiene education(58-61) are summarised in
Box 1
Components of sleep hygiene education:
Integration of sleep-related content into the educational curricula of all age groups would be helpful in inculcating good sleep hygiene habits from a young age. Workplace educational programmes focused on sleep hygiene and fatigue management have been shown to improve sleep duration, sleep quality and self-reported sleepiness complaints.(62) Having similar programmes in Singapore could hence benefit the working population to achieve better sleep health while fulfilling their work commitments. Primary care physicians could play the role of an educator by imparting good sleep hygiene advice to patients with sleep difficulties. These interventions would help to create and sustain a broad societal commitment to engaging in proper sleep habits as a primary tenet of health.
Adopt practices that reduce social jet lag and improve sleep health
‘Social jet lag’ is a term coined by Roenneberg(63) to describe the discrepancy between our individual circadian rhythm (biological time) and the external clock and timings that dictate our lives (social time). According to Roenneberg’s research,(64) the most frequent chronotype sleeps from about midnight to 8.00 am. In Singapore, however, most schools start at 8.00 am and require the student to be awake by 6.00 am to arrive on time. Most workplaces also start the day at 8.30−9.00 am, requiring working adults to wake up at around 7.00 am or earlier in order to navigate the morning commute and reach their workplaces on time. Hence, for many children, adolescents and adults, their biological time and social time are in a state of perpetual desynchrony.
It is often postulated that developmental shifts in sleep physiology and academic pressures in Singapore reduce the typical sleep of adolescents on a school night.(65,66) Delaying school start time to 8.30 am or later could reduce social jet lag among children and adolescents. This small change would reduce sleep curtailment experienced by most students and potentially benefit their physical and mental well-being. In a study conducted by Lo et al,(67) a school in Singapore implemented a 45-minute delay in school start time – from 7.30 am to 8.15 am. After one month, the students demonstrated improvements in sleep, alertness and mental well-being. These positive changes were maintained at nine months as well. Re-evaluation of the scheduling of co-curricular activities and regulation of the amount of homework assigned to students would also facilitate the practice of good sleep hygiene, as students would be able to have an early evening dinner, complete their homework, and have adequate time to unwind and relax before bedtime.
The introduction of flexitime at the workplace could improve sleep health among the working population. Flexitime usually refers to a schedule that allows employees to choose their starting and finishing times daily, as long as they complete a stipulated number of working hours. There are many benefits of flexitime that could impact mental health directly or indirectly. Employees could choose the time of the day to start work depending on their chronotype, so that it coincides with the time they feel most alert and productive. Flexitime could also enable employees to meet their personal responsibilities, for example, fetching their children to and from school. This arrangement would help employees balance their work and personal lives better, resulting in reduced stress levels and potentially increased productivity and motivation at work. It is thus heartening to read that in 2019, the Ministry of Manpower, Singapore, reported that more companies in Singapore were offering flexible work arrangements to employees.(68) The Work-Life Grant, which provides funding support to companies that implement flexible work arrangements, received a boost in 2019 when the government added SGD 70 million to its budget in order to encourage more companies to offer flexible work arrangements for their employees.(69) These initiatives were introduced with the aim of improving work-life balance. The incorporation of ‘achieving better sleep health’ as another objective behind these initiatives would help to underscore the importance of sleep health.
In France, there is a ‘right to disconnect’ law that bars employers and employees alike from sending work-related emails and text messages after office hours.(70) A similar policy could be beneficial to sleep health in the local working population. Instead of being encumbered with work-related concerns in the period leading up to bedtime, working individuals could use the time after work to exercise and unwind in preparation for a good night’s sleep.
Given that exposure to light-dark patterns is one of the main environmental cues for the circadian rhythm, poorly designed workspaces that do not allow adequate natural lighting could upset the individual’s sleep-wake cycle and contribute to poor nocturnal sleep. Fluorescent lights used in some workspaces do not emit the luminous intensity seen in natural daylight and hence do not have the same effect on the circadian rhythm as natural daylight. Blue-enriched light-emitting diodes, on the other hand, can mimic the intensity and spectrum of natural daylight, and has been shown to improve subjective alertness, performance and evening fatigue.(71) Some studies(62,72) have shown that workplace environmental modifications, such as access to windows and daylight exposure, are associated with improved nocturnal sleep and daytime function. Designing workspaces with these considerations in mind could go a long way towards helping workers achieve better sleep health and improve work performance.
Enhance screening and treatment of sleep disorders
The primary care physician has an important role to play in the screening and treatment of sleep disorders. The chief benefit of physicians enquiring about sleep is early detection and treatment of sleep disorders. In addition, improvements in sleep may lead to improvements in other chronic medical conditions.(73-75) Screening could be targeted at patient populations who are more susceptible to sleep difficulties, such as those with chronic medical conditions, chronic pain or other mental illnesses. In the elderly, research has shown that sleep patterns change with normal ageing independent of medical comorbidities and medications, such as reduced nocturnal sleep duration, reduced sleep efficiency, reduced slow-wave sleep and increased nocturnal awakenings.(76-80) Patients who are overweight are at higher risk of sleep-related breathing disorders such as obstructive sleep apnoea(81-83) as well as chronic insomnia,(84) while patients who work shifts or irregular hours are at risk of shift work sleep disorder.(85) Primary care physicians could include screening questions about sleep in their conversations with these higher-risk patients, asking open-ended questions such as, ‘How is your sleep?’ or ‘How many hours of sleep do you get on a typical night?’ These questions help to screen for patients with sleep difficulties; a more detailed sleep history can be taken from the patient. History-taking for sleep would include questions pertaining to sleep habits and symptoms suggestive of a sleep-wake disorder, such as a parasomnia, breathing-related sleep disorder or circadian rhythm sleep-wake disorder. This would facilitate early referral of patients to a sleep medicine specialist.
Specific education and training strategies are also needed to increase awareness among healthcare professionals. Continuing medical education for primary care physicians on the topic of sleep and sleep disorders could increase their proficiency in sleep health management. Improved curriculum content and certification requirements for the training of sleep medicine, and the potential creation of sleep medicine as a new medical subspecialty, would expand local capabilities in treatment and research of sleep disorders.
CONCLUSION
Sleep medicine is a rapidly evolving field that has led to an increased understanding of human chronobiology and an increased recognition of the importance of sleep health. While there has been a wealth of new research findings, little of this knowledge has been translated into practical changes that can be introduced into daily life to improve sleep health. However, other countries that implemented various sleep health interventions have reported promising results, and similar interventions could bring about positive changes to sleep health in the local community.

About the First Author
Dr Hatta Santoso Ong is an Associate Consultant Psychiatrist at the Department of Psychological Medicine and the Department of Sleep Medicine, Surgery and Science at Changi General Hospital, Singapore. He treats a variety of conditions, including mood and anxiety disorders, psychotic disorders, sleep disorders and addiction disorders. His academic appointments include Clinical Instructor, Duke-NUS Medical School, and Clinical Lecturer, Yong Loo Lin School of Medicine, National University of Singapore. He is also a Physician Faculty Member for the SingHealth Family Medicine Residency Programme.


