Abstract
INTRODUCTION
It remains unclear which advanced airway device has better placement success and fewer adverse events in out-of-hospital cardiac arrests (OHCAs). This study aimed to evaluate the efficacy of the VBM laryngeal tube (LT) against the laryngeal mask airway (LMA) in OHCAs managed by emergency ambulances in Singapore.
METHODS
This was a real-world, prospective, cluster-randomised crossover study. All OHCA patients above 13 years of age who were suitable for resuscitation were randomised to receive either LT or LMA. The primary outcome was placement success. Per-protocol analysis was performed, and the association between outcomes and airway device group was compared using multivariate binomial logistic regression analysis.
RESULTS
Of 965 patients with OHCAs from March 2016 to January 2018, 905 met the inclusion criteria, of whom 502 (55.5%) were randomised to receive LT while 403 (44.5%) were randomised to receive LMA. Only 174 patients in the LT group actually received the device owing to noncompliance. Placement success rate for LT was lower than for LMA (adjusted odds ratio [OR] 0.52, 95% confidence interval [CI] 0.31–0.90). Complications were more likely when using LT (OR 2.82,0 95% CI 1.64–4.86). Adjusted OR for prehospital return of spontaneous circulation (ROSC) was similar in both groups. A modified intention-to-treat analysis showed similar outcomes to the per-protocol analysis between the groups.
CONCLUSION
LT was associated with poorer placement success and higher complication rates than LMA. The likelihood of prehospital ROSC was similar between the two groups. Familiarity bias and a low compliance rate to LT were the main limitations of this study.
INTRODUCTION
Establishing an airway is integral in the management of out-of-hospital cardiac arrests (OHCAs). There is still some debate with regard to the benefit of paramedic-performed endotracheal intubation. While previous studies showed improved survival outcomes with endotracheal intubation,(1,2) recent data suggest that supraglottic airways in OHCAs result in better outcomes, likely owing to reduced interruptions to chest compressions and shorter placement times.(3-6) These devices are designed to be inserted without direct laryngoscopy and do not require the level of training and experience that is required for endotracheal tube insertion.
Several devices are available in the market, including the laryngeal mask airway (LMA), VBM laryngeal tube (LT; VBM Medizintechnik GmbH, Baden-Württemberg, Germany) and the Combitube® (Tyco-Healthcare-Kendall-Sheridan, Mansfield, MA, USA). They provide a direct route of ventilation via the trachea and avoid the complication of gastric insufflation that comes with bag-valve-mask ventilation. The LT and Combitube have a distal cuff to prevent regurgitation.
In Singapore, about 79% of patients with OHCA receive advanced airway in the form of LMAs.(7) The self-reported success rate of LMA insertion by Singapore paramedics is 50%–87%.(8) Complications reported internationally include incomplete seal and partial airway obstruction.(9) In contrast, the LT is reported to have higher insertion success rates when compared with the LMA in the prehospital setting, together with lower complications of regurgitation, vomiting and dislodgement.(10,11) The LT has also been used by minimally trained non-medical staff for OHCAs, with some success.(12) This ease of placement was associated with reduced ‘hands-off’ time during chest compressions.(13)
The present study aimed to evaluate the placement success and complication rates of VBM LT usage, as compared with the Ambu Aura-i LMA (Ambu A/S, Ballerup, Denmark), by paramedics in patients with OHCAs in Singapore.
METHODS
We conducted a real-world, prospective, parallel-group, cluster randomised trial. All patients with OHCAs aged over 13 years and attended to by Singapore Civil Defence Force (SCDF) paramedics from March 2016 to January 2018, both medical and traumatic, were included. Patients who did not meet the criteria for resuscitation by paramedics, such as cases of rigor mortis, decapitation and dependent lividity, were excluded. In order to achieve 80% power for detecting a difference of 15% for insertion rates and an alpha level of 0.05, we calculated that 875 patients were required, assuming a dropout rate of 20%.
Stratified randomisation was conducted with four strata based on the number of ambulances each station had, which ranged from 1 to 4. Block randomisation was then performed within each stratum to assign the ambulances to administer the LMA or LT. The ambulances randomised to the LT group continued to carry the LMA as a back-up device during their runs.
Because the LT was new to the paramedics, all paramedics attended an eight-hour training programme comprising a lecture and a hands-on session conducted by the study investigators and were required to demonstrate competency on a manikin before being allowed to participate in the trial. Paramedics in Singapore are taught the use of the LMA as part of their certification to be a paramedic, and participants were presumed competent in the use of LMA for the purpose of this study.
Ethical approval was obtained from the SingHealth Centralised Institutional Review Board and a waiver of consent was obtained. The study was also approved by the SCDF’s Medical Advisory Committee, which oversees the medical care delivered by paramedics in Singapore.
The primary outcome was placement success, and the secondary outcomes were complication rates and the presence of prehospital return of spontaneous circulation (ROSC). Per-protocol analysis was conducted to evaluate the results. We compared the association between outcomes and the airway device group using multivariate binomial logistic regression analysis. Statistical analysis was performed using IBM SPSS Statistics version 24.0 (IBM Corp, Armonk, NY, USA).
Modified intention-to-treat analysis was conducted using backward selection models as well as comparison of adjusted odd ratios to ensure robustness of models. These were adjusted for age above 65 years, gender, ethnicity, type of case, witness by paramedics, bystander cardiopulmonary resuscitation, initial electrocardiogram rhythm, collapse-to-paramedic arrival time, time at scene and paramedic experience.
RESULTS
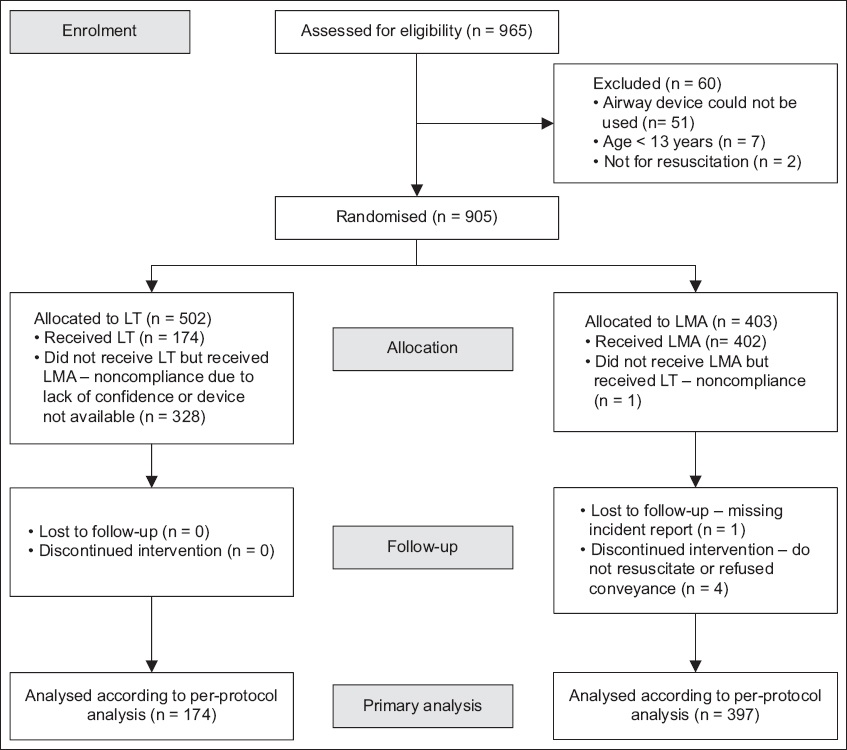
A total of 965 patients were recruited for the study, of whom 60 were excluded owing to reasons such as inability to use airway devices, age less than 13 years and patients deemed unsuitable for resuscitation. Among the remaining patients, 502 (55.5%) patients were allocated to the LT group and 403 (44.5%) to the LMA group. In the LT group, 174 patients actually received LT but none were lost to follow-up. Among the LMA group, 402 patients received LMA, with one patient lost to follow-up and four patients having the intervention discontinued (
Fig. 1
Flowchart shows recruitment of patients into the study arms. LMA: laryngeal mask airway; LT: laryngeal tube
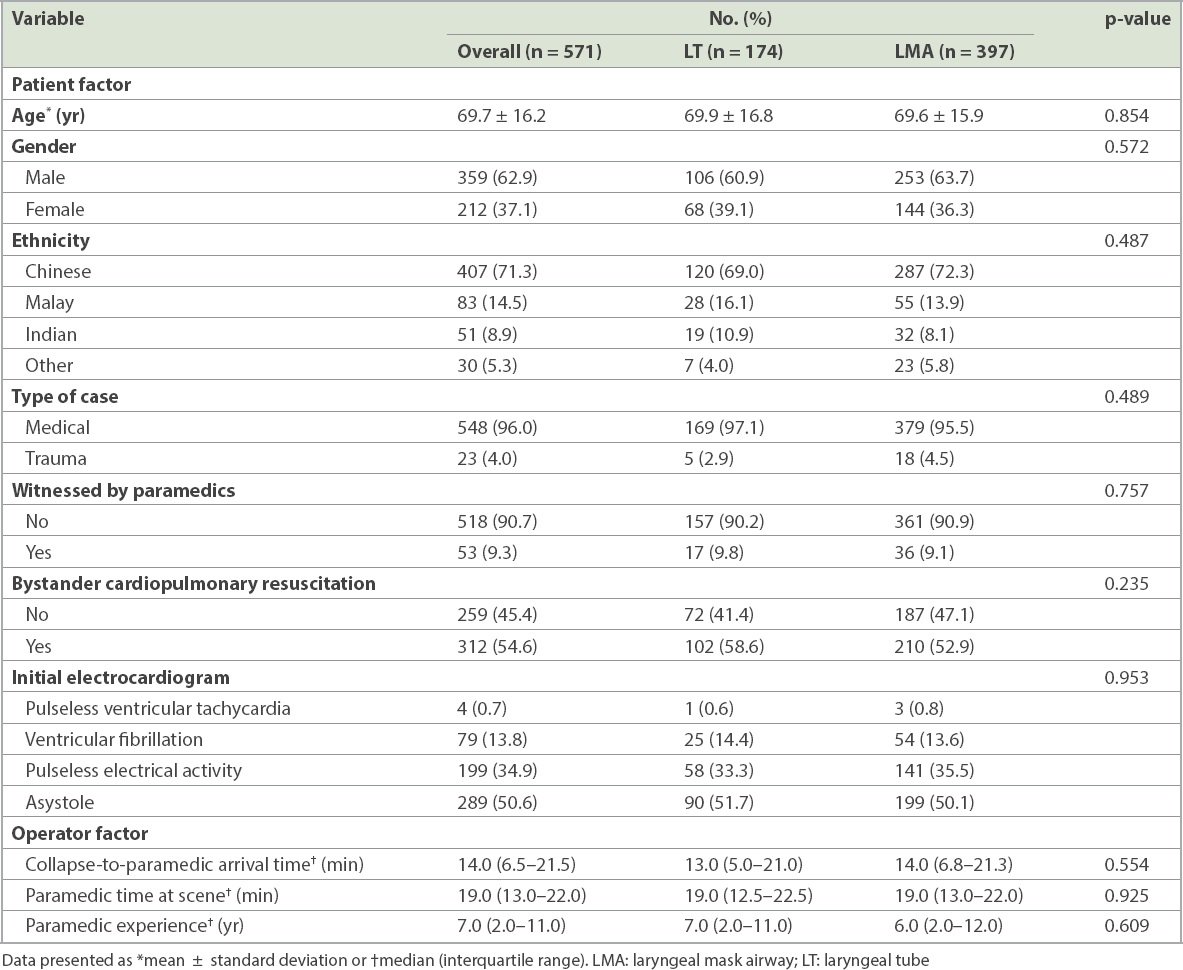
Per-protocol analysis was conducted. The mean patient age was 69.7 ± 16.2 years, with 62.9% of the patients being male and 37.1% being female (
Table I
Demographics and per-protocol analysis results of the study population.
More successful placement attempts were recorded in the LMA group (89.4%) than in the LT group (82.8%), and those in the LMA group had a higher success rate at the first attempt (75.6% vs. 66.1%) (
Table II
Outcome measures by airway management.
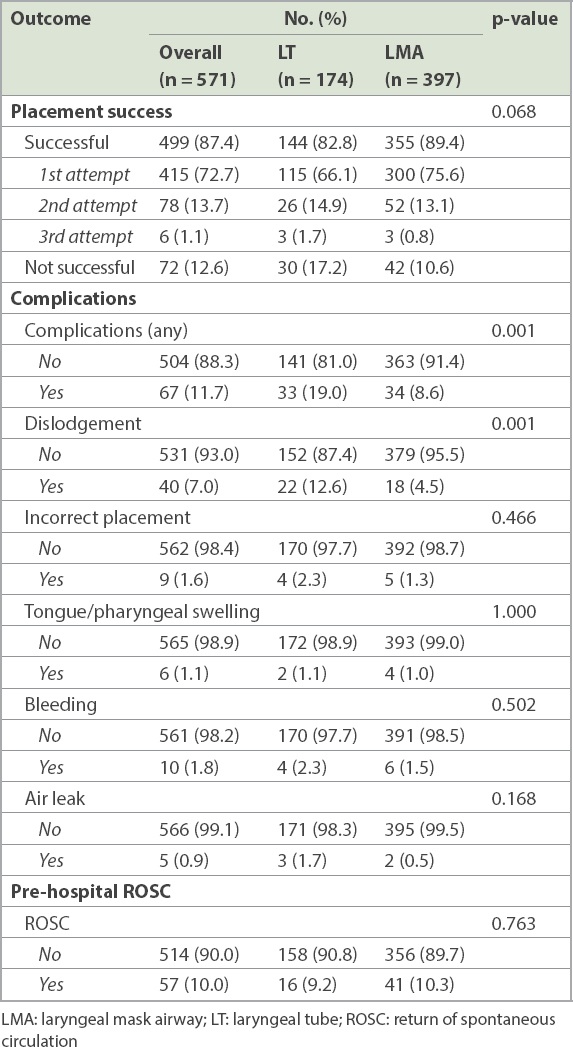
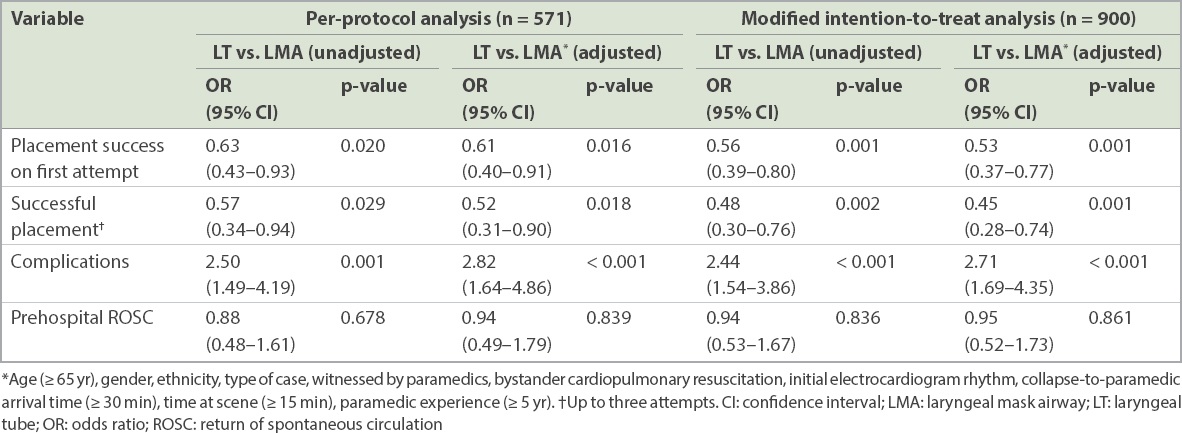
On applying modified intention-to-treat analysis, the odds of successful LT placement (odds ratio [OR] 0.53, 95% confidence interval [CI] 0.37–0.77, p = 0.001) and LT-related complications (OR 2.71, 95% CI 1.69–4.35, p < 0.001) were both significant (
Table III
Association between airway management and outcome measures.
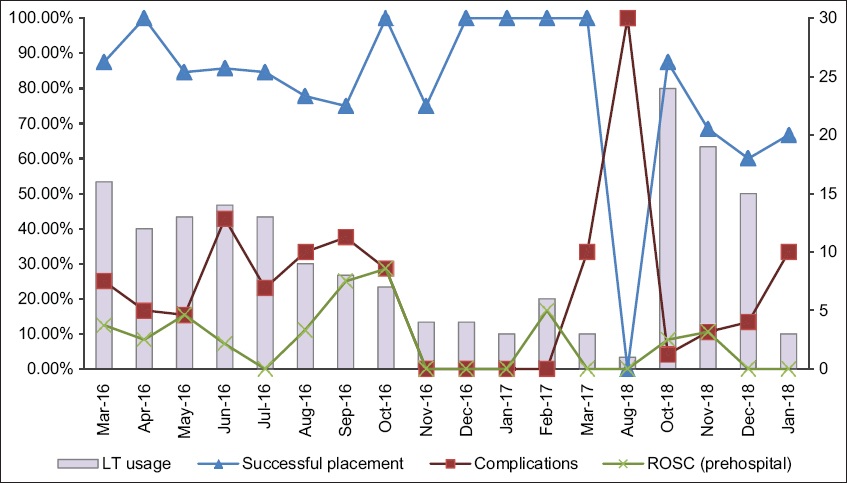
Use of LT was highest in the first five months of the trial, as were the placement success and complication rates. LT usage then decreased to half during the rest of the trial period. The placement success rate also decreased in the second half of the trial (
Fig. 2
Graph shows monthly outcome measures for the LT group over time. LT: laryngeal tube: ROSC: return of spontaneous circulation
DISCUSSION
We found that LT was associated with more complications and fewer successful placement attempts by paramedics for patients with OHCAs in Singapore. Prehospital ROSC rates were similar between the LT and LMA groups. The main limitation of this study was the high noncompliance rate with the new LT device and familiarity bias. Time to successful placement of airway device was also not recorded.
It was difficult to determine whether the poorer outcomes were attributed to the LT itself or to the unfamiliarity with the device. The LMA has been used by Singapore paramedics for over a decade, and prior to the study, none of the paramedics had any experience with LT. For patient safety, the LMA was initially carried by all ambulances allocated to the LT group as a rescue device. The sample size was increased from 875 to 1,015 to account for an unexpected dropout rate of 45% instead of the initially anticipated 20%. This change was performed with approval from the institutional review board.
Familiarity bias was significant in our study. While a survey conducted immediately after the LT training was held showed that a majority of paramedics found LT easy to use, and the initial usage rate seemed to support this, it appeared that paramedics were still uncomfortable using it, possibly owing to a much greater familiarity with the use of the LMA. A five-month interruption in LT supply to ambulance stations during the second half of the trial also likely resulted in further unfamiliarity and increased lack of confidence, as evidenced by the decreased placement success rate and increased rates of complications that were associated with the LT group in the latter half of the trial. It is also likely that the placement success and complication rates themselves were affected by this lack of familiarity and confidence, as was self-reported.
Previous studies have suggested that using LT instead of endotracheal intubation improved OHCA survival.(3) However, studies have also shown that the use of LT may be associated with severe complications, such as life-threatening tongue swelling, massive gastric distension and incorrect placement.(14,15) A follow-up study is thus warranted, with more rigorous study design, after intensive training and involving paramedics with a longer period of experience in using LT to better evaluate the efficacy of whether the LT truly results in improved patient outcomes. Time to placement of airway device should also be assessed. Other clinical outcomes, such as survival to admission and discharge, can also be looked into, in addition to a qualitative evaluation of paramedic attitudes towards new airway devices.
This preliminary study served to identify gaps to improve the training of paramedics in using LT, as the group had fewer successful placements and more complications as well as low paramedic compliance. With more elaborate studies, the choice for supraglottic airway device for the prehospital care of patients with OHCAs will become clearer.
ACKNOWLEDGEMENTS
We would like to thank Ms Masnita Rahmat, Warrant Officer 1 at SCDF’s Medical Department, for her assistance in training the paramedics and Dr Takashi Tagami, Fellow at Duke-NUS Medical School, for aiding in the statistical analysis. We are also grateful to the coinvestigators of Pan-Asian Resuscitation Outcomes Study Clinical Research Network Singapore for their contributions to this study.


