Abstract
INTRODUCTION
The purpose of this study was to compare the clinical outcomes of elderly hip fracture patients who received surgical treatment with those who received non-surgical treatment.
METHODS
This retrospective study involved 2,756 elderly patients with hip fractures who were admitted over a six-year period. The patients’ biodata, complications, ambulatory status at discharge and length of hospital stay were obtained from the institution’s hip fracture registry.
RESULTS
Among the 2,756 hip fracture patients, 2,029 (73.6%) underwent surgical intervention, while 727 (26.4%) opted for non-surgical intervention. The complication rate among the patients who underwent surgical intervention was 6.6%, while that among the patients who underwent non-surgical intervention was 12.5% (p < 0.01). The mean length of hospital stay for the surgical and non-surgical hip fracture patients was 15.7 days and 22.4 days, respectively (p < 0.01).
CONCLUSION
Surgical management of hip fractures among the elderly is associated with a lower complication rate, as well as a reduced length of hospital stay.
INTRODUCTION
Hip fractures are one of the most common types of fragility fractures encountered by orthopaedic surgeons.(1) The worldwide incidence of hip fractures was 1.26 million in 1990,(2) and this number has been projected to reach 6.3 million by 2050.(3) In Singapore, the proportion of elderly patients in the general population is expected to increase over the next several decades. Geriatric patients are at high risk of hip fractures, and the management of hip fractures adds a significant economic burden to healthcare systems.(4,5)
There are two main types of hip fractures – femoral neck fractures (i.e. intracapsular) and intertrochanteric fractures (i.e. extracapsular). Management of hip fractures can be either surgical or non-surgical. Patients with hip fractures, regardless of whether they received surgical or non-surgical intervention, are predisposed to high complication rates (range 14%–52%).(6-8) The one-year mortality rates range from 22% to 51% and are reported to be six times higher than in the general population.(9) While surgical intervention is expected to be the ideal treatment option (since it permits faster functional recovery), there are limited studies comparing the outcomes of surgical and non-surgical treatments for hip fractures.(10-12)
Tan Tock Seng Hospital (TTSH), Singapore, is a major trauma centre in which hip fractures constitute about 8% of all orthopaedic emergency admissions. Clinical data on all patients who were admitted to TTSH with hip fractures has been entered into a hip fracture registry since the year 2000. The purpose of the present study was to review the epidemiological data of all patients with hip fractures and the clinical outcomes of surgical and non-surgical treatments for hip fractures.
METHODS
In TTSH, a hip fracture registry was developed for clinical audit, and has been in use since 2000. The clinical data of all patients aged ≥ 60 years who were diagnosed with a hip fracture was entered into the registry. A hip fracture is defined as a femoral neck (i.e. intracapsular) fracture or an intertrochanteric (i.e. extracapsular) fracture. A dedicated research coordinator entered the relevant clinical data into an electronic database (Stata 9.0; StataCorp LP, College Station, TX, USA). Data was collected over a six-year period (2000–2005). The present study, a retrospective observational review of the hip fracture registry, was approved by the institutional review board.
During the six-year period, all the patients were under the care of senior orthopaedic surgeons, and geriatric physicians oversaw the clinical optimisation of the patients. They were advised to undergo surgical treatment and informed of the risks of both surgical and non-surgical management. No patient was excluded from surgical management on the basis of their age or American Society of Anesthesiologists (ASA) score.
Patients who consented to surgery underwent operative procedures that the senior orthopaedic surgeons deemed appropriate for their diagnosis. Orthopaedic registrars and consultants performed all the procedures. At the induction of anaesthesia, the patients were administered broad-spectrum antibiotics as a prophylaxis; this was continued postoperatively until the surgical drains were removed. Following surgical intervention, the patients were placed on a standardised postoperative clinical pathway for hip fractures. All the patients received antithrombotic stockings, but pharmacological agents for deep vein thrombosis (DVT) prophylaxis were selectively administered only to high-risk patients. When the patients attained satisfactory ambulatory status, they were discharged home or to an outpatient rehabilitation facility.
Patients who opted for non-surgical management were treated with skin leg traction until early fracture consolidation or clinical resolution of pain was noted. The patients were then started on appropriate assisted ambulation following physiotherapist review, and discharged to their own homes, rehabilitation hospitals or nursing homes once they had made stable early recovery. A multidisciplinary team, consisting of orthopaedic surgeons, geriatric physicians, physiotherapists, occupational therapists and orthopaedic specialist nurses, reviewed the patients in both the surgical and non-surgical treatment groups daily prior to their discharge.
Retrieval of clinical data was done by a single person (the author who was not involved in the clinical management of the hip fracture patients). The patients’ biodata, operative interventions, complications following surgical/non-surgical treatment, ambulatory status at discharge and length of hospital stay (LOS) were reviewed. Chi-square test and Mann-Whitney U test were used to compare the clinical characteristics and ambulatory status at discharge of both the surgical and non-surgical patients. Robust regression using iteratively reweighted least squares was applied to ascertain how the identified covariates were associated with LOS. All data was analysed with Stata 9.0. A p-value < 0.05 was considered to be statistically significant.
RESULTS
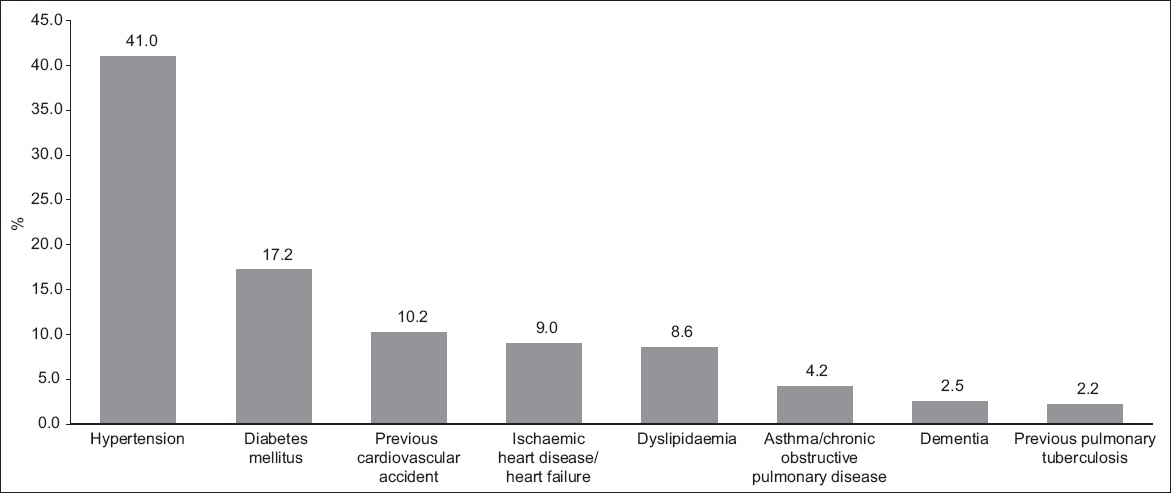
A total of 2,756 patients aged ≥ 60 years were admitted to TTSH with a diagnosis of hip fracture during the six-year period. The female-to-male ratio was 3:1, and the ethnic distribution of the patients was as follows: Chinese 89.2%; Malay 5.3%; Indian 4.0%; Eurasian 0.5%; and others 0.9%. The types of hip fracture diagnosed were intertrochanteric fractures and femoral neck fractures. The mean age of the patients was 79.6 (range 50–108) years. The two most common comorbidities were hypertension and diabetes mellitus (
Fig. 1
Bar graph shows the comorbidity distribution of the patients with hip fractures (n = 2,756).
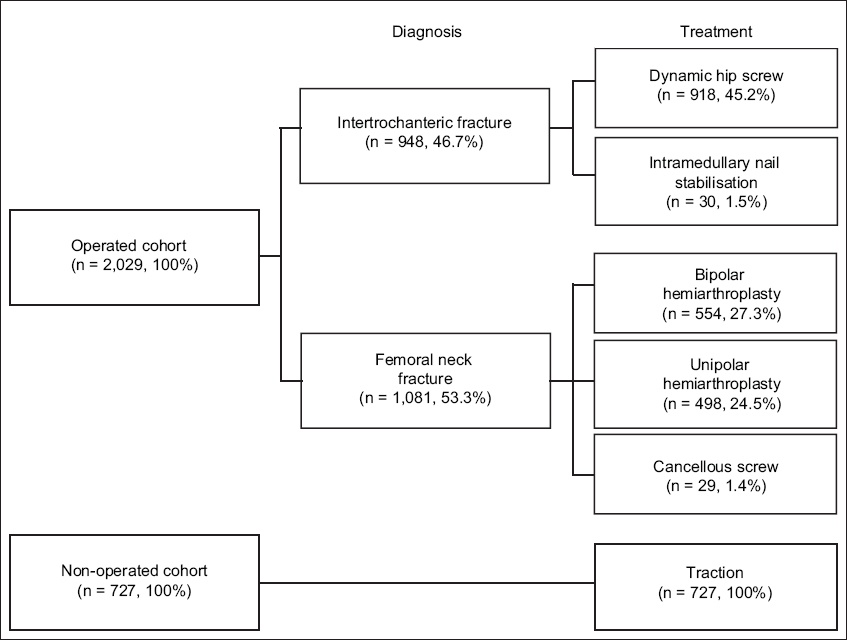
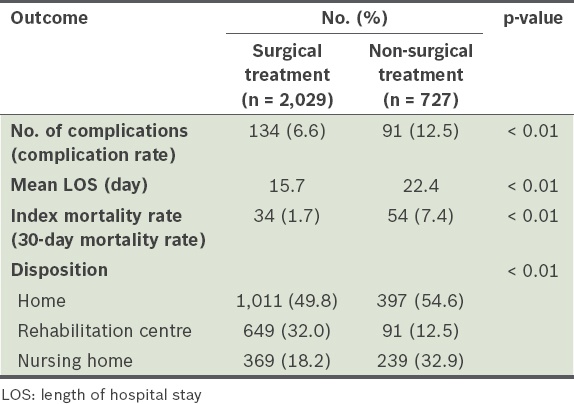
Among the 2,756 patients, 2,029 (73.6%) underwent surgical intervention and 727 (26.4%) opted for non-surgical intervention (
Table I
Clinical characteristics of patients (n = 2,756) according to type of treatment.
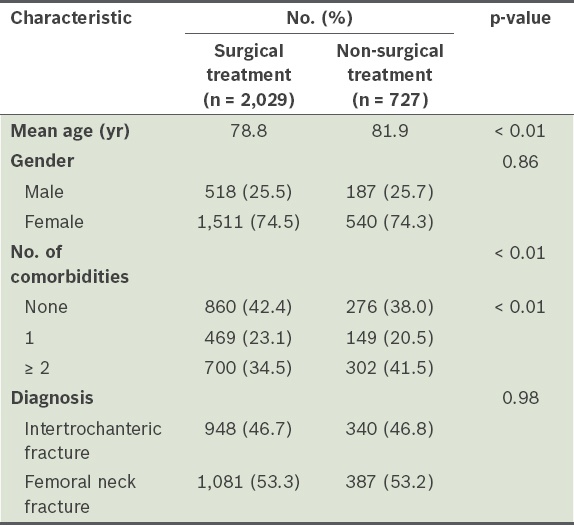
Fig. 2
Flow chart shows the diagnoses and types of treatment of patients with hip fractures (n = 2,756).
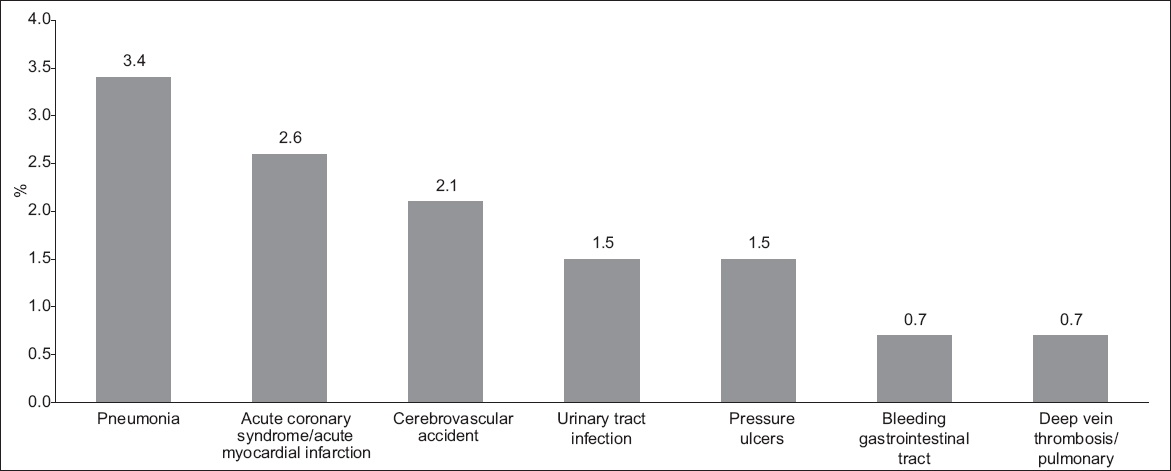
Complications following surgical treatment were recorded for 134 of the 2,029 patients (complication rate: 6.6%). Most patients (5.4%) presented with only one complication. The three most common complications were urinary tract infection (1.9%), pressure sores (1.0%) and wound infection (0.7%). Among the 2,029 surgical patients, DVT was diagnosed in 11 (0.5%); these patients were treated with appropriate oral anticoagulation therapy. The index mortality rate among the patients who underwent surgical treatment was 1.7% (i.e. 34 of the 2,029 patients died within 30 days following surgical intervention). Among the patients who opted for non-surgical treatment, 91 had complications (complication rate: 12.5%). The three most common complications were pneumonia (3.4%), acute coronary syndrome (2.6%) and cerebrovascular accident (2.1%). There were 54 (7.4%) mortalities within the 30-day period following admission for hip fracture among this group of patients.
The breakdown of complications among the patients who underwent surgical and non-surgical treatments is shown in Figs.
Fig. 3
Bar graph shows the complications among the patients who underwent surgical treatment (n = 2,029).
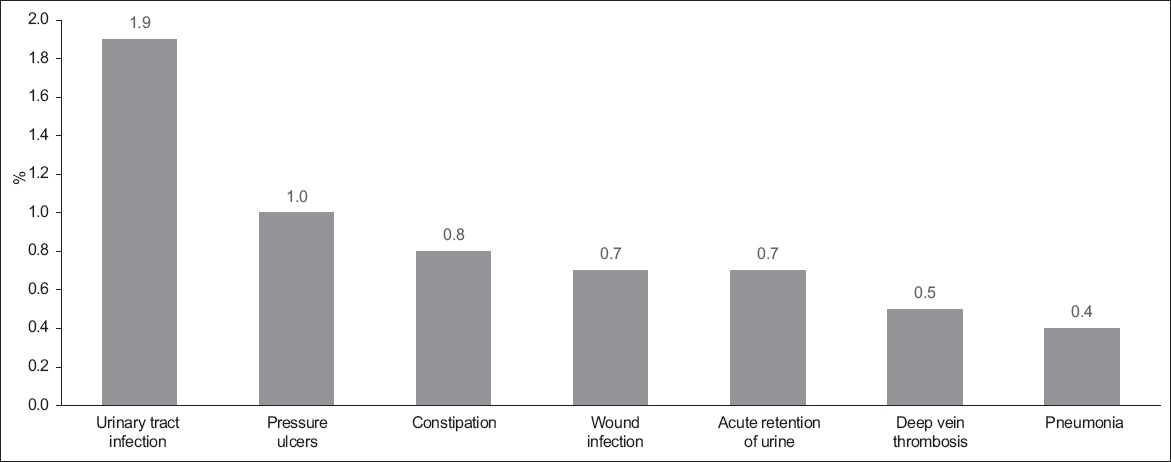
Fig. 4
Bar graph shows complications among the patients who underwent non-surgical treatment (n = 727).
The median (range) and mean LOS of the patients who underwent surgical treatment were 14 (range 2–93) days and 15.7 days, respectively, while those of the patients who underwent non-surgical treatment was 18 (range 0–163) days and 22.4 days, respectively. By comparison, the mean LOS of the patients who underwent surgical treatment was significantly lower than that of the patients who underwent non-surgical treatment (p < 0.01). Among the patients who received surgical treatment, more than half (55.0%) attained independent ambulatory status (with or without walking aids) and most were discharged home (49.8%) or to a rehabilitation centre (32.0%). Among the non-surgical patients, 397 (54.6%) were discharged home, while 91 (12.5%) were discharged to a rehabilitation hospital to continue to gain assistance in mastering daily living skills for an extended period of time. The disposition outcome data of the two groups of patients is shown in
Table II
Clinical outcomes of patients (n = 2,756) according to type of treatment.
DISCUSSION
Patients with hip fractures have a considerable risk of various medical and surgical complications, prolonged LOS and mortality.(7,8,13) Surgical fixation of these fractures facilitates favourable clinical recovery, and the various determinants of clinical outcome have been extensively reviewed.(14-16) Many authors have noted that undue delay in surgical treatment increases morbidity and mortality following hip fractures.(17,18) Surgical intervention facilitates early mobilisation and early discharge of patients, thereby lowering LOS. Extended LOS is unfavourable, as it increases the risk of acquiring nosocomial infections.(19) Furthermore, early mobilisation decreases the risk of the typical complications associated with recumbency (i.e. pneumonia, decubitus ulcers and DVT).
In the present study, the complication rate was significantly lower among hip fracture patients who underwent surgical treatment than those who underwent non-surgical treatment. Although some studies have suggested that there is an increased risk of complications among older patients who undergo surgery for hip fractures, other studies have shown no such association.(8,15) The patients in this study were not denied surgical treatment on the basis of age or ASA scores; this might account for the fact that the index mortality rate in the present study (1.7%) was comparable to the rates reported in other studies.(5,7) Although the overall complication rate was lower for the patients who underwent surgical treatment, there is a finite risk of mortality associated with undergoing surgery for hip fractures. Since hip fractures almost exclusively affect older patients (who have lower physiological reserves), there is a definite operative risk secondary to anaesthesia and blood loss. Also, despite the immediate benefits of surgical intervention, complications secondary to suboptimal fracture fixation have been reported, at 15%–55%.(16)
Non-surgical treatment conventionally involves the use of skeletal traction for an extended period of several weeks.(11,20) This, however, increases the risk of pin-site infections and decubitus ulcers. In TTSH, most of the patients who opted for non-surgical treatment were given skin leg traction for 4–8 weeks until clinical resolution of pain; thereafter, the patients were started on early rehabilitation exercises. It has been reported that an extended period of bed rest with traction can increase the risk of morbidity and mortality among patients with hip fractures who opt for non-surgical treatment.(21)
The literature comparing surgical and non-surgical treatment of hip fractures is sparse, and there is a lack of objective comparisons.(10,11,13) Ethical considerations hinder the possibility of randomised studies to evaluate the immediate postoperative outcomes of these two treatment modalities. Although the differences between the two treatment modalities may seem obvious, the present study provided clinical data on the different postoperative outcomes of surgical and non-surgical treatments, which was based on a sizable study population. This data can be used by physicians to advise patients about their treatment options, as part of the informed consent process.
The present study was not without limitations. As this was a retrospective study, randomisation of treatment received by the patients could not be done. While significant differences in age and comorbidities between the two treatment groups should ideally be matched, the patients in both treatment groups were similar in their age and comorbidity distribution. Hence, matching techniques (such as propensity score matching) were not carried out, as the disadvantages associated with the use of such techniques (including introducing bias and a loss of power)(22) were anticipated to outweigh the minor confounding effect of age and comorbidity. Other than that, since the data used in this study was retrieved from the hip fracture registry of our hospital, which only tracked patients during their inpatient stay and for any readmissions within 30 days, no long-term data was available on the patients who underwent surgical and non-surgical treatments.
To conclude, surgical management of hip fractures has a more favourable postoperative outcome (i.e. decreased complication rate) and is also associated with a shorter LOS than non-surgical management of hip fractures.


