Abstract
Levocardia (left-sided cardiac apex) with abdominal situs inversus is extremely rare. This is also known as isolated levocardia and is almost always associated with severe forms of congenital heart defects with poor prognosis. We report isolated levocardia in a 13-year-old symptomatic male patient. The purpose of this paper is to outline the imaging features of isolated levocardia and to highlight the role of cardiovascular magnetic resonance imaging (CMR) in the diagnosis and management of such cases. Other forms of cardiac malposition, including dextrocardia, mesocardia and criss-cross heart, with chest radiograph and CMR correlation, are also discussed.
CLINICAL PRESENTATION
A 13-year-old male patient on long-term follow-up for complex congenital heart disease at the paediatric cardiology unit presented with shortness of breath. He was born via elective lower section Caesarian section (LSCS) at 38 weeks due to the mother’s two previous LSCSs. He had normal body weight and Apgar scores at birth. He was apparently well until Day 3 of life, where he was found to have a cardiac murmur prior to discharge. Echocardiography then showed complex congenital heart disease with a single ventricle, left-sided major aortopulmonary collaterals and pulmonary atresia. At two months of life, he was admitted for an elective right Blalock-Taussig (BT) shunt. A subsequent left BT shunt was performed at 20 months of age. Chest radiography was performed for the patient (
Fig. 1
Frontal chest radiograph of the patient.
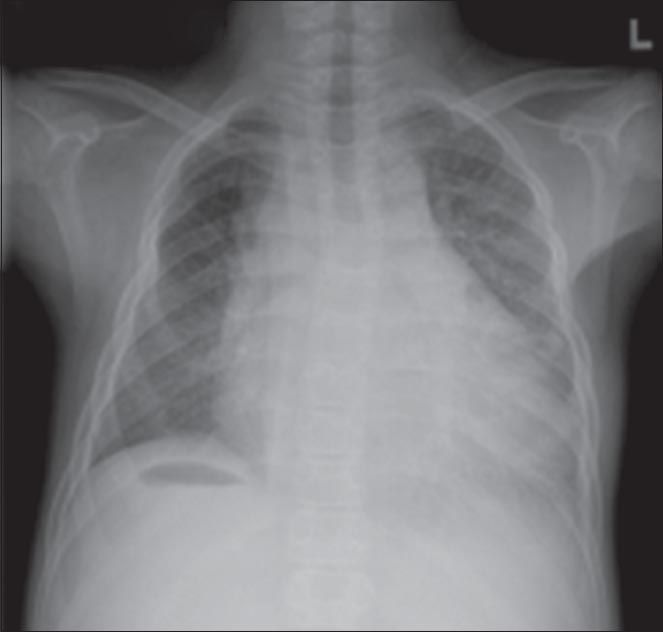
IMAGE INTERPRETATION
The chest radiograph (
DIAGNOSIS
Levocardia with abdominal situs inversus.
CLINICAL COURSE
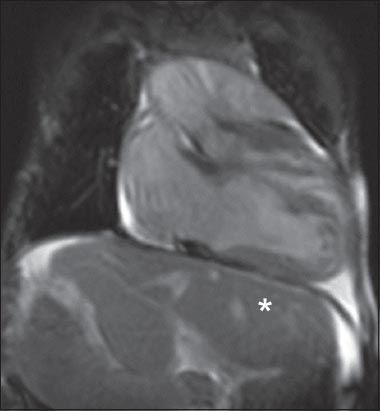
By the time the patient was 13 years old, his left BT shunt was patent. However, the flow of the right BT shunt into the right pulmonary artery (RPA) was not well demonstrated on echocardiography, and the patient had developed poor effort tolerance. Early in the patient’s life, it was decided that a long-term Fontan operation was deemed unsuitable, as he had non-confluent pulmonary arteries on angiography and reconstruction may not be possible. Cardiovascular magnetic resonance imaging (CMR) was performed after echocardiography in order to better delineate the anatomy, and to quantify volumes and function. This was because further palliative surgery was considered given that the patient’s average oxygen saturation level was 80% on room air. CMR demonstrated atrial situs inversus, right-sided univentricular atrioventricular connection, double outlet right ventricle, and single ventricle physiology with an outlet ventricular septal defect (
Fig. 2
Selected CMR still image from a cine coronal gradient-echo sequence of the heart and upper abdomen shows the presence of levocardia with abdominal situs inversus. The right lobe of the liver is seen below the left hemidiaphragm (*).
The patient subsequently developed IgA nephropathy, which augmented his congestive cardiac failure. He had repeated admissions for decompensated congestive cardiac failure, but succumbed at the age of 17 years to end-stage heart failure secondary to complex congenital heart disease and IgA nephropathy with superimposed pneumonia.
DISCUSSION
Situs refers to the position of the atria (not the cardiac apex) and abdominal viscera relative to the midline. Levocardia, dextrocardia and mesocardia are general terms that indicate the position of only the cardiac apex and do not give any indication of the cardiac structure or abdominal situs.
Situs solitus is the normal arrangement of abdominal organs with levocardia (
Fig. 3
(a) Conventional chest radiograph shows normal arrangement of the heart and abdominal organs. The stomach bubble (*) is seen on the left upper quadrant and the liver on the right upper quadrant. (b) Corresponding image from a coronal localiser gradient-echo sequence CMR.
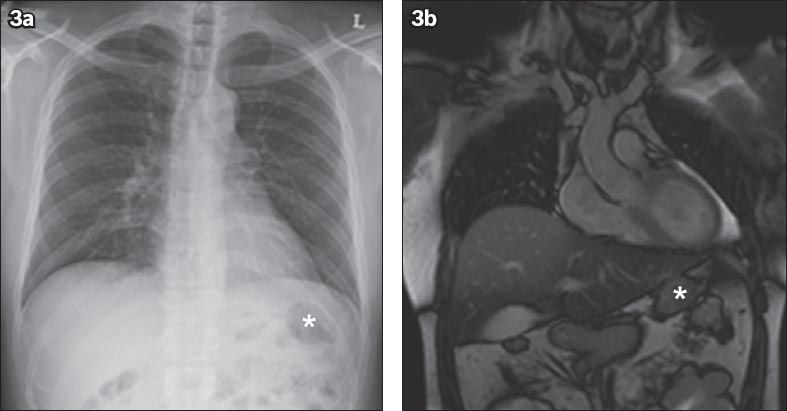
Fig. 4
(a) Chest radiograph shows dextrocardia with situs solitus, as evidenced by the stomach bubble (*) located below the left hemidiaphragm. (b) Selected image from a coronal half-Fourier acquisition single-shot turbo spin-echo (HASTE) CMR confirms the diagnosis.
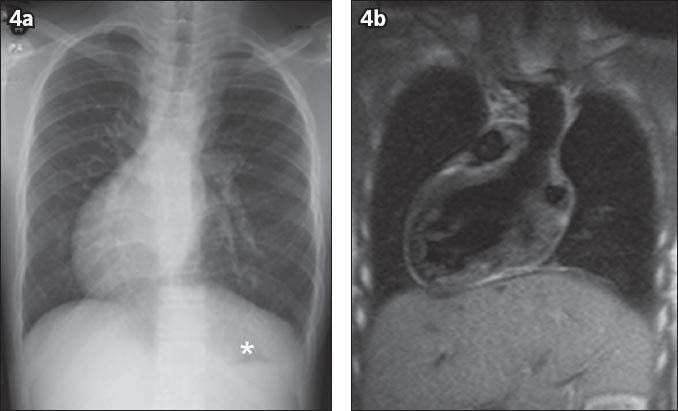
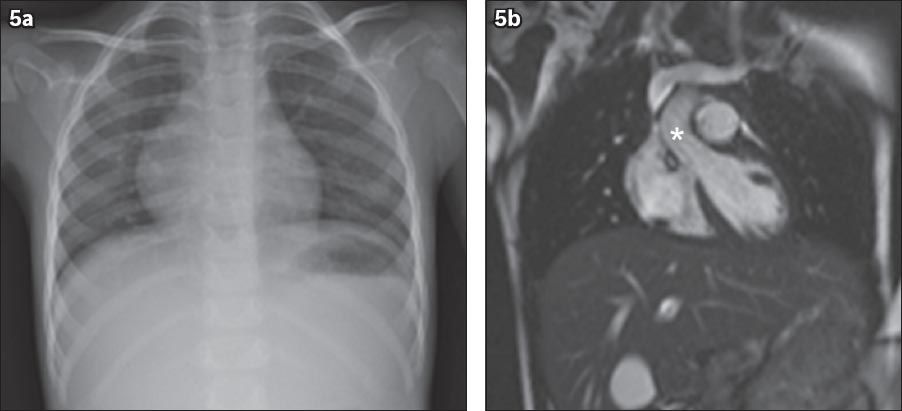
Fig. 5
(a) Chest radiograph of a 7-year-old girl shows midline cardiac position in the presence of thoracic and abdominal situs solitus. The cardiac silhouette extends equally to the right and left of midline. The cardiac silhouette is hump-shaped due to superimposition of the right atrium and right ventricle. (b) Selected image from a cine gradient-echo left ventricular outflow tract view of the same patient confirms that the bulk of the cardiac mass is in the centre of the thorax. Normal position of the ascending aorta is noted (*).
In situs ambiguous (situs indeterminatus or heterotaxia), there is abnormal arrangement of the organs and major blood vessels, which is different from that of situs solitus and situs inversus (
Fig. 6
(a) Chest radiograph shows dextrocardia. (b & c) Selected images from a coronal HASTE sequence of the same patient show normal position of the liver and stomach bubble (*) with polysplenia (S).
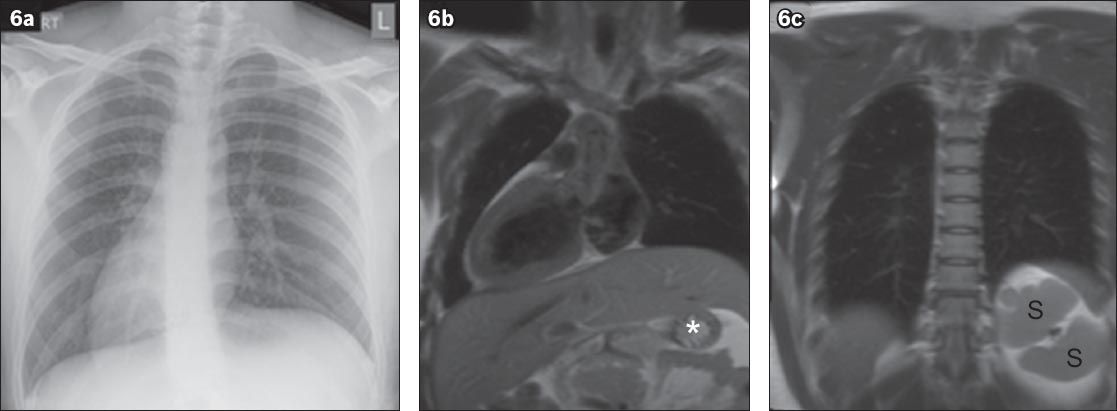
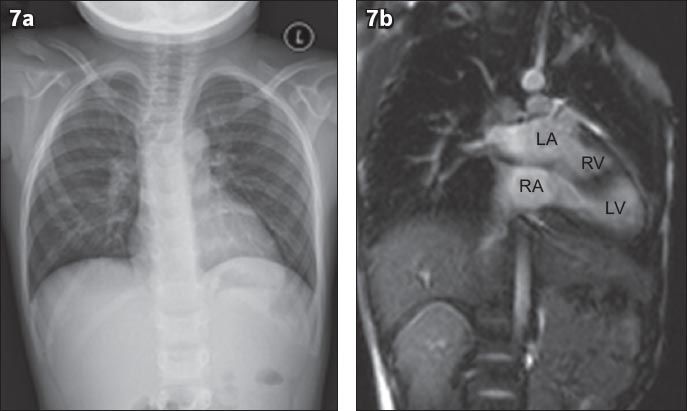
Fig. 7
(a) Conventional chest radiograph shows normal arrangement of the heart and abdominal organs. (b) Selected still image of the same patient from a coronal cine gradient-echo sequence shows the left atrium (LA) located superiorly to the right atrium (RA). LV: left ventricle; RV: right ventricle.
Our patient had situs inversus, which is almost always associated with dextrocardia. Its association with levocardia where the cardiac apex is located in a normal position is extremely rare.(1) Almost 100% of cases of situs inversus with levocardia are associated with congenital heart disease,(2) most of which are severe or associated with asplenia or polysplenia syndromes, or situs ambiguous.(5) Situs inversus with levocardia has a reported incidence of 1:22,000 in the general population and accounts for 0.4%–1.2% of all individuals with congenital heart diseases.(5)
The exact cause of situs inversus with levocardia is not fully understood.(5) The condition can be identified or excluded via a thorough history and physical examination, chest radiography, electrocardiography and echocardiography.(6) Depending on the initial examination findings, computed tomography (CT) or CMR may also be used. CT provides good anatomic detail for confirming visceral organ position, cardiac apical position, intracardiac anatomy and great vessel branching. CT, however, entails radiation, which should be avoided in the paediatric age group. CMR, which does not utilise ionising radiation, is the optimal imaging modality for confirming the above. CMR is also the gold standard for determining cardiac volumes and function.(7-9)
The prognosis of situs inversus with levocardia is poor, and only 5%–13% of patients survive for more than five years, mainly due to the severity of an associated cardiac abnormality.(6) It is important for clinicians to be aware of the fact that discordant cardiac shadows and stomach bubbles are usually found in association with severe abnormalities of the heart and major blood vessels. These imaging findings should prompt a thorough investigation for potential abnormalities. CMR is usually used for complex and difficult cases.


