Abstract
A 31-year-old male motorcyclist presented with prepatellar swelling of the left knee after a collision with a car. Magnetic resonance imaging of the knee showed no bony or ligamentous injury to the knee. Instead, a well-defined, thin-walled, T2-weighted hyperintense fluid collection with internal septations was identified in a prefascial location overlying the left patella and patellar tendon. The findings were in keeping with those of a Morel-Lavallée lesion, a closed internal degloving injury. Morel-Lavallée lesions are occasionally encountered after a blunt soft-tissue trauma. The presentation and imaging features are discussed.
CASE PRESENTATION
A 31-year-old male motorcyclist presented to the emergency department after hitting the side of a car. He had been travelling at approximately 50 km/h. The patient sustained blunt trauma to the left knee and bilateral upper limb abrasions. He was alert and conscious on his arrival at the emergency department.
Physical examination of the left knee revealed superficial abrasions and swelling over the patella. Anterior and posterior drawer tests and stress testing of the left knee joint were negative. Plain radiography of the left knee joint demonstrated prepatellar soft tissue swelling, but no fracture was evident. The prepatellar swelling was persistent at follow-up. Magnetic resonance (MR) imaging of the left knee was performed.
What do the MR images show? What is the diagnosis?
IMAGE INTERPRETATION
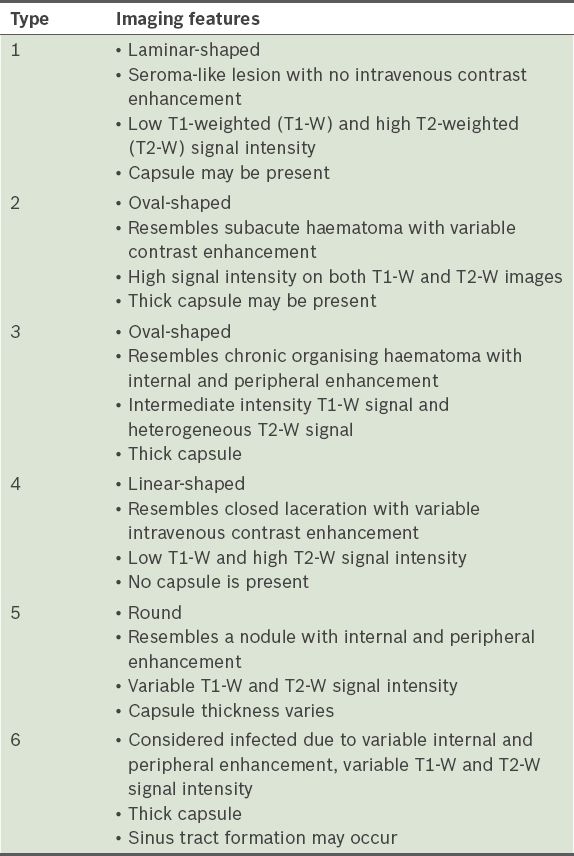
The MR images show a well-defined T2-weighted hyperintense fluid collection, sited in a prefascial location within the deep subcutaneous layers immediately overlying the left patella and patellar tendon (arrows in Figs.
Fig. 1
Axial T2-W turbo spin-echo fat-saturated MR image of the left knee joint.
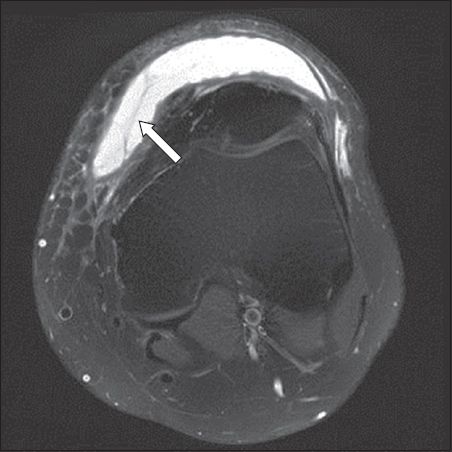
Fig. 2
(a) Sagittal PD turbo spin-echo fat-saturated and (b) 1.7 mm PD turbo spin-echo MR images of the left knee joint.
DIAGNOSIS
Morel-Lavallée lesion.
CLINICAL COURSE
The patient was managed conservatively. The Morel-Lavallée lesion subsequently resolved with compression and physiotherapy.
DISCUSSION
A Morel-Lavallée lesion is a post-traumatic, closed, internal degloving injury that was first described by French surgeon Victor Auguste Francois Morel-Lavallée in the 19th century.(1) It results from direct or tangential shearing forces across the surface of the skin, causing the subcutaneous tissue to be detached from the underlying fascia and creating a potential space between the hypodermis and the superficial fascia.(2-4) These shearing forces disrupt the perforating vessels and lymphatic channels, filling the potential space with blood, lymph, debris or fat.(2-4) In some cases, a local inflammatory reaction and granulation tissue may eventually organise to form a capsule, which can prevent resorption of the contents and lead to a persistent fluid collection.(5) In severe cases, a large area of necrosis may also occur, with the risk of superimposed infection.(3,4) The subcutaneous fluid collection can vary in internal composition depending on the severity of the injury, therefore resulting in different imaging appearances. Fluid accumulation due to arterial bleeding may develop rapidly, while fluid accumulation from lymphatic disruption develops much more slowly.(4,6) Due to early presentation, Morel-Lavallée lesions with arterial bleeding can be diagnosed early, while other lesions often present late, from months to years after the initial trauma. Morel-Lavallée lesions may resolve spontaneously or persist if a capsule is present.(7) They are usually found adjacent to osseous protuberances. Commonly reported locations are along the greater trochanter, lumbar spine and periscapular region. Other locations include the flank, buttock (
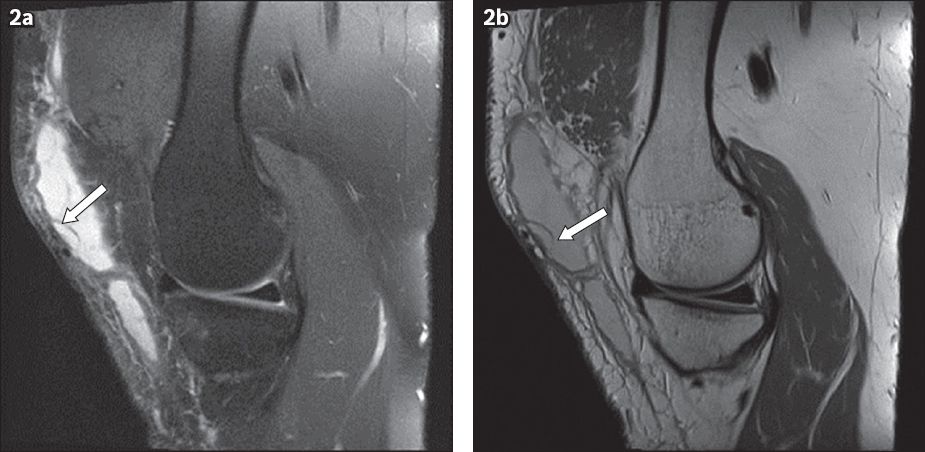
Fig. 3
(a) Axial T1-W fat-saturated and (b) T2-W fat-saturated MR images of the pelvis in a 41-year-old man who presented with a six-month history of bilateral buttock swelling. The patient had a previous history of trauma (i.e. he slipped and fell on his back). The MR images show several T1-W and T2-W hyperintense, large, well-defined, lobulated cystic lesions in the deep subcutaneous layer of both gluteal regions. Fluid-fluid levels (black arrows), internal septations (white arrows) and frond-like projections (arrowheads) in the walls of the lesion may represent remnants of fat lobules. Percutaneous drainage was performed with good response.
Patients with Morel-Lavallée lesions usually present with pain, swelling and stiffness. On physical examination, a soft, fluctuant area showing contour deformity, skin discolouration, skin hypermotility and change in sensation or skin necrosis may be found.(8) Initial investigation using plain radiography may detect a soft tissue mass and any associated fractures (
Fig. 4
Left knee plain radiographs of the patient in
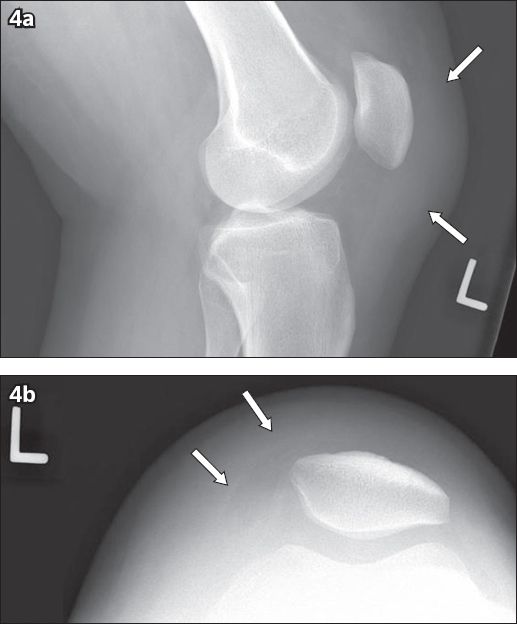
Fig. 5
A 27-year-old man presented following a road traffic accident in which he sustained a handlebar injury. Abdominal US image in transverse plane shows an encapsulated fluid collection (white arrows) within the deeper aspect of the right epigastric fat, located in the prefascial plane immediately superficial to the upper right rectus abdominis muscle (*). Note the relatively echogenic appearance of the pseudocapsule (black arrow). No internal septation, debris or vascularity is demonstrated.
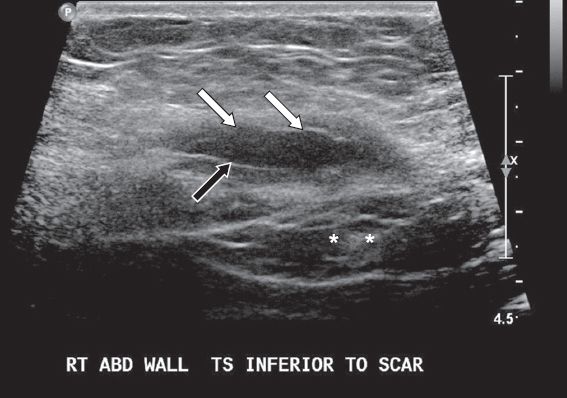
These lesions may appear anechoic, hypoechoic or hyperechoic depending on the composition of the collections, with blood and fat appearing more echogenic. There is no significant correlation between echogenicity and the age of a lesion.(9) A high index of suspicion and awareness of the condition are required to differentiate Morel-Lavallée lesions from another differential diagnosis that may mimic it on ultrasonography, including acute post-traumatic haematoma, abscess, fat necrosis, neoplasm and postoperative seroma.(9) The characteristic prefascial location of Morel-Lavallée lesions and a preceding history of trauma are important clues to reaching the correct diagnosis.
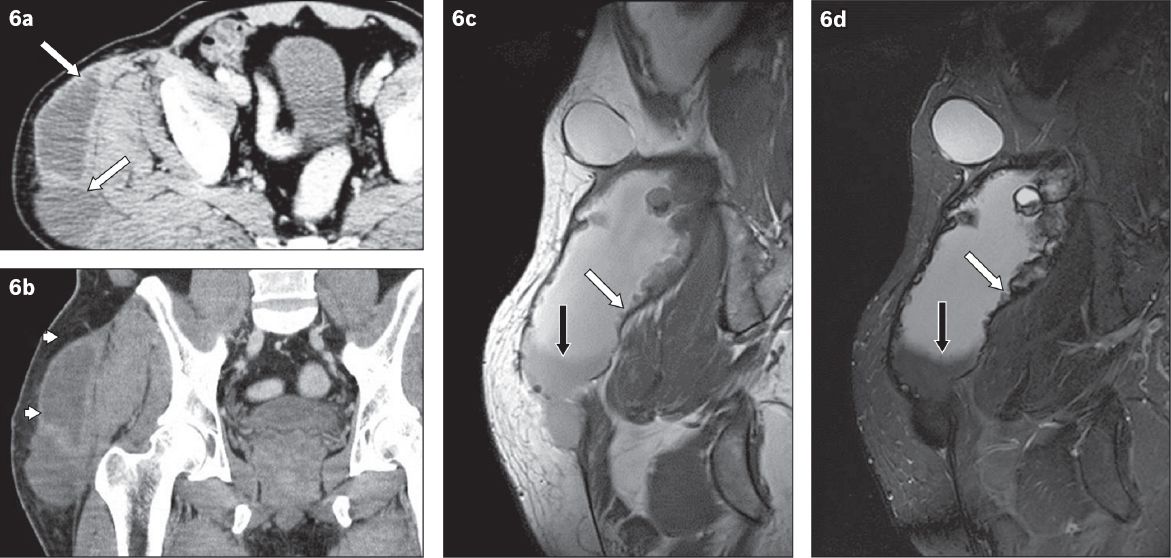
On CT, the position of the Morel-Lavallée lesions between the hypodermis and underlying fascia is clearly shown.(9) The density of the collection is dependent on the composition, with blood being +30 to +45 Hounsfield units and fat being −50 to −100 Hounsfield units. Fluid-fluid levels have been reported, which may be due to sedimentation of cellular components in blood and/or liquefied fat.(5,10) A hypodense pseudocapsule may develop following a local inflammatory response and can be readily seen on CT; it may show enhancement on intravenous contrast medium (
Fig. 6
A Morel-Lavallée lesion superior and lateral to the right hip joint in a 54-year-old man with a right gluteal soft tissue mass that gradually enlarged over the past four years. He sustained a contusion on the right hip in a road traffic accident nine years ago. (a & b) Axial and coronal CT images show two large subcutaneous cystic lesions on the lateral aspect of the right greater trochanter/hip and gluteal region. The anterosuperior lesion shows a thickened capsule (white arrows), while the more inferoposterior lesion is multiloculated (arrowheads). No internal septation or fluid-fluid level is seen. (c & d) Coronal T1-W and T2-W fat-suppressed images of the right hip show several T1-W and T2-W hyperintense, large, well-defined, lobulated cystic lesions in the deep subcutaneous layer. Note the fluid-fluid levels (black arrows) and frond-like projections (white arrows).
MR imaging is the imaging modality of choice for the evaluation and diagnosis of Morel-Lavallée lesions.(2) On MR imaging, they are well-defined and discrete, and may be oval, fusiform or crescentic in shape.(8) The margins can sometimes taper and fuse with adjacent fascial planes. The signal intensity of the lesion is dependent on the concentration of the haemolymphatic fluid.(2,5) Capsules, when present, may be complete or incomplete and are hypointense on all pulse sequences.(11) Some Morel-Lavallée lesions may show variable enhancement on postcontrast-enhanced MR imaging.
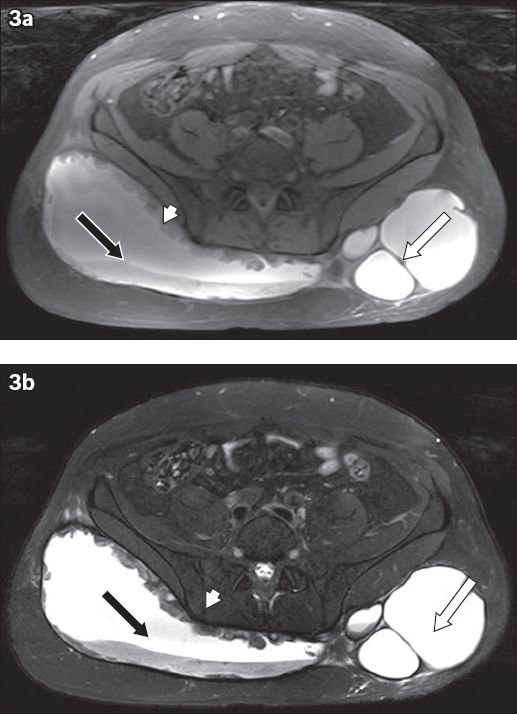
An MR imaging classification system for Morel-Lavallée lesions was proposed by Mellado and Bencardino.(2) There are six types of lesions and they are classified based on the shape of the lesion, the presence of a capsule, signal and enhancement characteristics (
Morel-Lavallée lesions should be differentiated from fluid collections that appear similar, such as bursae, abscesses or intramuscular haematomas. Bursae are fluid collections occurring in known anatomical locations and are closely related to articulating joints, whereas Morel-Lavallée lesions are usually distant from joints. Unlike these lesions, bursae tend to have some synovial lining. Morel-Lavallée lesions may also be painful to the patient, but are usually not inflamed or tender to palpation in the absence of infection; patients are, in general, not significantly unwell. Their prefascial location and well-defined outlines differentiate Morel-Lavallée lesions from intramuscular haematomas.
Treatment of Morel-Lavallée lesions is dependent on the extent and severity of the underlying injury. Conservative management with compression, motion exercises and cryotherapy can be used for small acute lesions with no capsule.(12,13) In a retrospective study of 27 Morel-Lavallée lesions of the knee by Tejwani et al, the mean time taken for such fluid collections to resolve following conservative treatment was reported to be 10.6 ± 9.2 days.(13) Percutaneous drainage and sclerodesis with doxycycline and talc were found to have good outcomes in the treatment of encapsulated lesions.(13) Aspiration of Morel-Lavallée lesions can help to relieve pain from pressure, although reaccumulation of fluid can occur post-aspiration or after an initial apparent resolution, necessitating surgery. Tejwani et al reported that Morel-Lavallée lesions requiring aspirations took 23.7 ± 28.5 days to resolve.(13) Surgical management techniques, such as open debridement, can be considered for encapsulated lesions when conservative management and percutaneous treatment have failed.(14) Antibiotic therapy is indicated for superimposed infection.
CONCLUSION
Morel-Lavallée lesions are closed, internal degloving injuries after a traumatic injury that result in detachment of subcutaneous tissues from the underlying fascia, creating a potential space that is filled with haemolymphatic fluid of any combination. Given the complex and variable appearance of Morel-Lavallée lesions, MR imaging is the diagnostic imaging modality of choice. The presence of a capsule is an important radiologic finding as lesions with capsules are unlikely to respond to conservative management.
Supplementary material
SMJ-57-51.pdf
References