Abstract
A 54-year-old woman presented with a large mass on her right hand that was progressively enlarging over a period of a few years. She had cosmetic concerns about the enlarging mass and experienced interference with routine activity. Physical examination revealed a soft, mobile, non-tender, lobulated mass with well-defined margins. Magnetic resonance imaging showed the soft lump to be a lipomatous mass in the deep palmar space of the hand, which was subsequently surgically resected. The imaging features of deep palmar lipomas of the hand and other common benign lesions at this location are discussed.
CASE PRESENTATION
A 54-year-old woman presented with a large mass on her right hand that was progressively enlarging over a period of a few years. It was located on the palm in the thenar eminence. She did not have any neurological symptoms or muscular dysfunction, but had cosmetic concerns about the enlarging mass and reported that it interfered with her routine activity.
Physical examination revealed a soft, mobile, non-tender lobulated mass with well-defined margins. The overlying skin was intact, with no evidence of redness or increased temperature. The patient had no clinical evidence of compressive neuropathy or muscle dysfunction. The provisional diagnosis was a soft-tissue mass of unknown aetiology, and further evaluation with radiography and magnetic resonance (MR) imaging was suggested. What do the radiographs and MR images show? Is there cause for concern?
IMAGE INTERPRETATION
Frontal and oblique radiographs of the right hand (Figs.
Fig. 1
(a) Frontal and (b) oblique radiographs of the patient’s right hand.
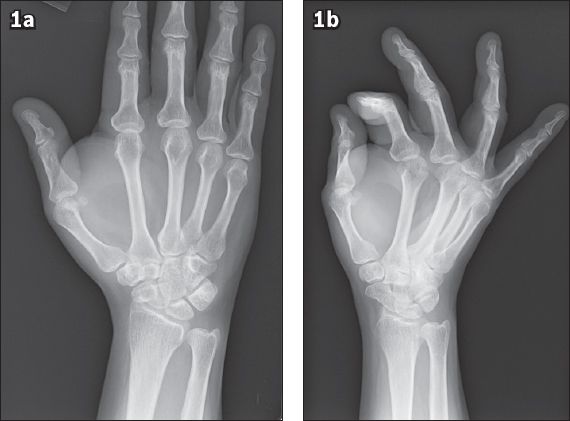
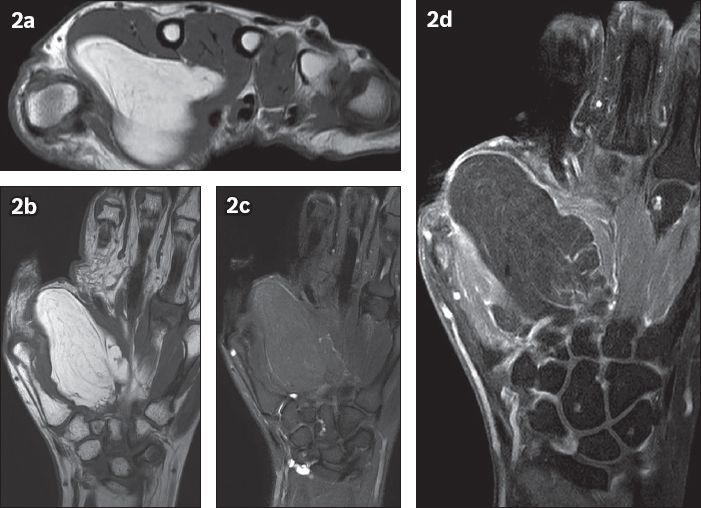
Fig. 2
(a) Axial T1-W, turbo spin-echo (TSE); (b) coronal T1-W, TSE; (c) T2-W, TSE, fat-saturated; and (d) T1-W, TSE, fat-saturated, contrast-enhanced MR images of the right hand.
DIAGNOSIS
Intermuscular lipoma in the thenar eminence of the right hand.
CLINICAL COURSE
Surgical excision was performed, as the lipomatous mass was interfering with the patient’s routine activity and for cosmetic concerns. During surgery, a soft-tissue mass was seen; it was deep to the thenar and adductor pollicis muscles, and superficial to the first dorsal interosseus muscle in the region of the deep arterial arch of the right hand. Histopathology revealed benign mature adipose tissue with occasional fibrous septations, in keeping with benign lipoma. No evidence of malignancy was noted.
DISCUSSION
Lipomas are the most common tumour throughout the body.(1) They are more frequently seen in obese individuals between the fifth and seventh decades of life. Lipomas are often associated with other conditions such as diabetes mellitus, hyperlipidaemia, goitre and Cushing’s syndrome. More rarely, they are associated with syndromes such as adiposis dolorosa, Gardner syndrome, Madelung’s disease and familial multiple lipomatosis.(2) Although fat is abundant in the deep palm, lipomas are rarely encountered in this location. The reported incidence of lipomas in the hands and fingers is about 1% of all lipomas that occur in the body.(3) Such lipomas are more commonly found in the subcutaneous plane. Less common locations include the subfascial plane, within Guyon’s canal, the carpal tunnel or deep palmar space,(4,5) where they are usually of larger size.(6) Thickness of the deep central palmar fascia may account for a more peripheral location in the thenar and hypothenar eminence.(7) This thickness also makes it clinically difficult to correctly assess the exact size and extent of the lipoma.
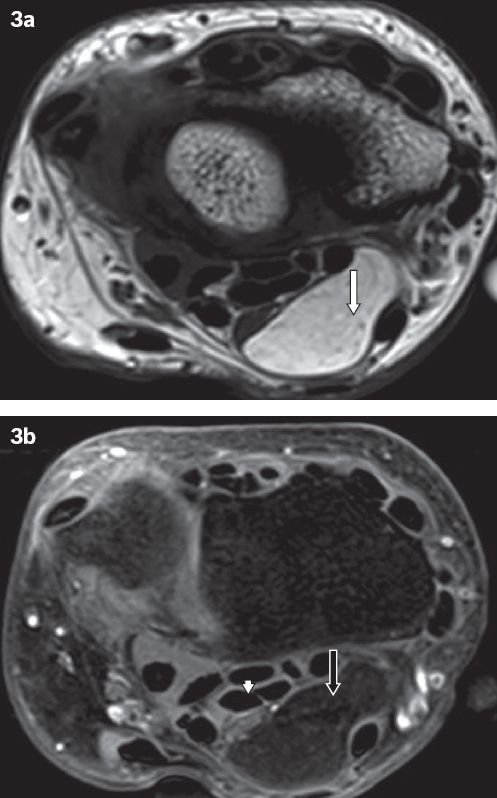
The clinical course of lipomas is often prolonged, with initial insidious growth followed by a prolonged and latent maintenance phase. Deep palmar lipomas are usually asymptomatic; symptoms arise mainly due to mass effect. Pain and paraesthesia secondary to nerve compression are more likely to occur if the lipoma is found in a closed anatomical space such as the carpal tunnel (
Fig. 3
Lipoma in the carpal tunnel in a 48-year-old woman who presented with a painless lump in the ventral aspect of the left wrist of several months’ duration. (a) Axial T1-W, turbo spin-echo MR image of the hand at the level of the left wrist shows a lipomatous mass within the carpal tunnel that is hyperintense on T1-W imaging (white arrow). (b) T1-W, turbo spin-echo, fat-saturated MR image with intravenous contrast shows the same mass with uniform suppression of signal (black arrow) without enhancement, consistent with a lipoma, with mild compression on the median nerve (arrowhead).
Lipomas larger than 5 cm are called giant lipomas,(10) such as in the case presented. Lipomas usually grow at a very slow rate and the aetiology of rapid growth into giant lipomas is debatable. It has been postulated that blunt trauma can cause disruption of fibrous septa between the skin and deep fascia, facilitating growth of fatty tissue. No apparent association has been established between tumour volume and patient symptomatology.(11) Rydholm and Berg, in a retrospective study of 428 cases of musculoskeletal lipomas, found that the incidence of solitary lipoma to sarcoma was 150/1 for lesions ≤ 5cm and 20/1 for lesions > 5cm.(12) Hence, patients should be informed that giant lipomas have an increased risk of malignancy.
History and clinical examination are usually sufficient to diagnose superficial lipomas. To diagnose deeper lesions, imaging is required to map the surrounding anatomic structures and detect any neurovascular structure involvement. Clinically, deeper lesions are soft, mobile, non-tender and doughy on palpation. However, the surgeon may not be able to palpate the entire extent of the deeper lesions due to overlying thick palmar fascia. In patients with compressive neuropathy, Tinel’s sign (defined as distal paraesthesia secondary to tapping on the tumour) may be elicited. Electrophysiological studies can be useful, but are not definitively diagnostic of lipomas.(13) On radiography, lipomas are nonspecific, often appearing simply as focal soft-tissue swelling. Lucency indicative of a fatty component (
Fig. 4
Magnified view of oblique radiograph of the right hand (seen in

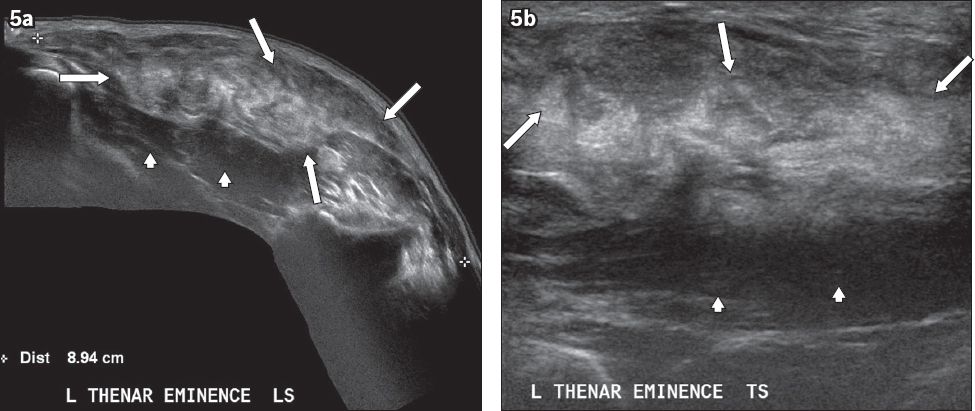
Fig. 5
Deep palmar lipoma in the thenar eminence of the left hand in a 45-year-old woman who presented with a painless lump of several months’ duration. Extended field-of-view (a) longitudinal and (b) transverse US images of the palm show a heterogeneously echogenic solid lump (arrows) in the deep thenar eminence superficial to the thenar muscles (arrowheads). The margins are slightly ill-defined.
MR imaging, with its multiplanar capability and superior tissue characterisation, is the imaging modality of choice in the assessment of lipomas. The use of MR imaging is recommended before biopsy attempts, as it may help in the selection of suspicious areas for histological evaluation. Non-image-guided biopsies can result in non-representative biopsy samples, potentially leading to misdiagnosis. In contrast, MR imaging clearly defines the deeper extension, adjacent tendons and neurovascular structures, which is vital if surgery is being contemplated; the degree of compression of the underlying nerves is often well-demonstrated. Classically, a lipoma appears as a slightly lobulated homogeneous mass with well-defined borders, and demonstrates hyperintense signal on both T1- and T2-weighted sequences. Small, thin, internal hypointense septa may be present. Complete suppression of the fat signal on fat-saturated sequences would show the benign nature of the mass. It can be located above muscle (i.e. supramuscular;
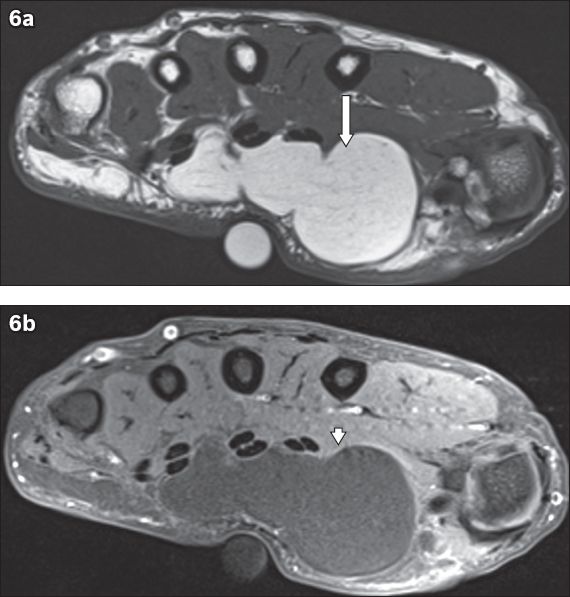
Fig. 6
Deep supramuscular palmar lipoma of the left hand in a 61-year-old woman who presented with a lump of several months’ duration associated with radial side numbness of the fourth finger. (a) Axial T1-W, turbo spin-echo (TSE) and (b) T1-W, TSE, fat-saturated with contrast MR images of the left hand show a thin-walled, septated lesion (arrow) that is hyperintense on T1-W MR imaging, with uniform suppression of fat signal (arrowhead in b) on the fat-saturated image suggestive of lipoma. The lesion is located superficial to the underlying flexor digitorum superficialis tendons and thenar muscles. No obvious enhancing soft-tissue component is seen.
Conservative management is advocated for asymptomatic patients with palmar lipoma. For symptomatic patients, surgery is the treatment of choice, ideally performed by a hand surgeon. All lipomas in the upper extremities that are > 5 cm (i.e. giant lipomas) should ideally be surgically removed due to the potential increased risk of malignancy. Monobloc resection with careful dissection of neurovascular components is performed to avoid iatrogenic injury. Local recurrence is very rare and the incidence of recurrence correlates with the heterogeneity detected on MR imaging.(11)
Other common, benign mass lesions in the palm include ganglion cysts, nerve sheath tumours, giant cell tumours (GCTs) of the tendon sheath, fibromas of the tendon sheath, arteriovenous malformations/haemangiomas and tenosynovitis. Ganglion cysts (Figs.
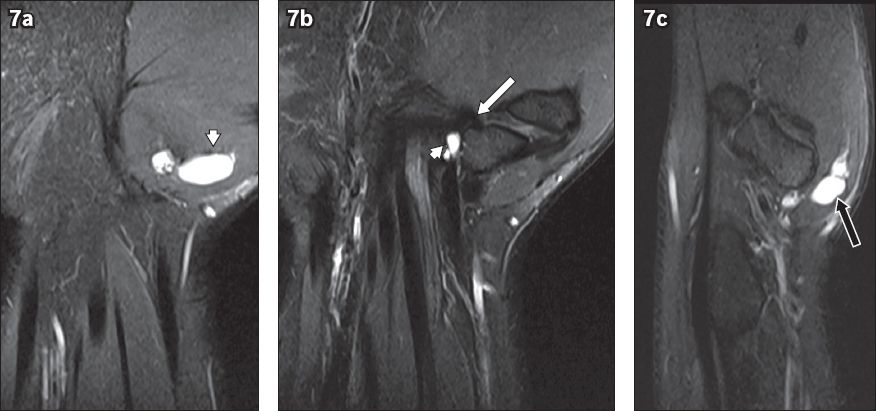
Fig. 7
Ganglion cyst in the thenar eminence of the right hand in a 40-year-old man who presented with pain in the wrist of several months’ duration. The patient experienced trauma to the wrist four years before presentation. (a & b) Coronal fat-saturated, T2-W, turbo spin-echo (TSE), images of the right hand show a lobulated, septated lesion that is hyperintense (arrowheads) on T2-W imaging. (c) Sagittal fat-saturated, T2-W, TSE MR image shows a lesion located deep in the thenar eminence (black arrow) and likely originates from the scaphoid/trapezium joint (white arrow in b), as better seen on the posterior coronal T2-W image.
GCTs of the tendon sheath (Figs.
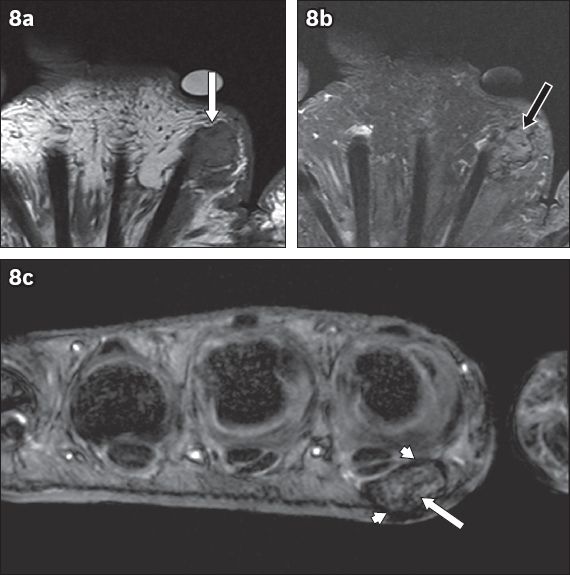
Fig. 8
Giant cell tumour of the tendon sheath in the palmar space of the left hand in a 69-year-old woman who presented with a painless lump of one year’s duration. (a) Coronal T1-W, turbo spin-echo (TSE); (b) T2-W, TSE, fat-saturated; and (c) axial T2-W, gradient-echo MR images of the left hand show a soft tissue nodule at the volar aspect of the second metacarpal that is isointense (white arrow in a) on T1-W imaging and intermediate in signal intensity (black arrow in b) on T2-W imaging, with low signal capsule (arrowheads in c) and spotty foci of hypointensity (white arrow in c) within the nodule, as better seen on the gradient-echo image.
In the hand, nerve sheath tumours usually arise from deeper, larger nerves, particularly schwannomas. Neurofibromas, however, tend to arise from smaller cutaneous nerves. Both types of tumours present in young patients and are small, solitary and slow-growing. They may be painless or present with pain and/or paraesthesia. Most of them are isolated cases without history of neurofibromatosis. On imaging, a nerve sheath tumour (Figs.
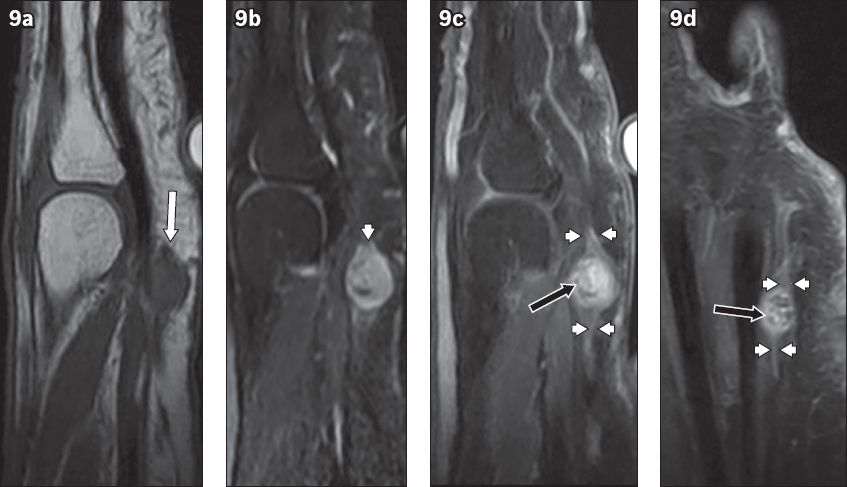
Fig. 9
Nerve sheath tumour in the left palm of a 61-year-old woman who presented with a lump and associated pain, with paraesthesia of her fourth and fifth digits, of several months’ duration. (a) Sagittal T1-W, turbo spin-echo (TSE); (b) T2-W, TSE, fat-saturated; and (c) contrast-enhanced sagittal and (d) coronal T1-W, TSE, fat-saturated MR images of the left hand show ovoid soft tissue mass in the palmar interval between the 4th and 5th metacarpal necks. The mass is isointense (white arrow in a) on T1-W imaging and hyperintense (arrowhead in b) on T2-W imaging with some central low-signal components. (c & d) There is enhancement with some hypointense foci (black arrows) on the contrast-enhanced images, with distal ends (arrowheads) that are likely continuous with the digital nerve, characteristic of a nerve sheath tumour.
Arteriovenous malformations/haemangiomas (Figs.
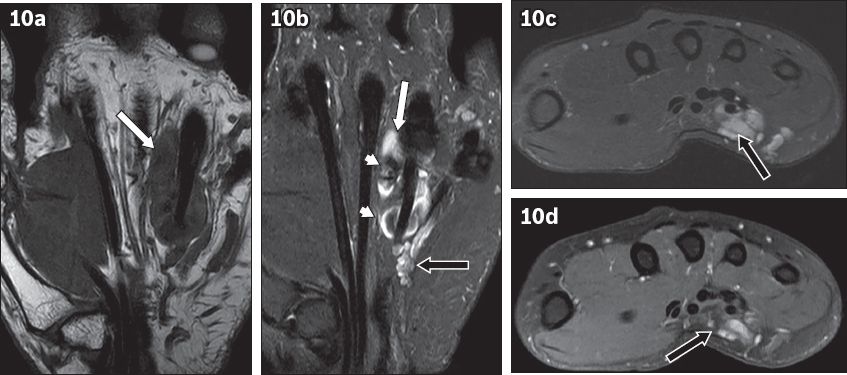
Fig. 10
Arteriovenous vascular malformation/haemangioma in the midpalmar space of the right hand in a 52-year-old woman who presented with painless swelling of several months’ duration. (a) Coronal T1-W, turbo spin-echo (TSE); (b) T2-W, TSE, fat-saturated; (c) axial T2-W, TSE, fat-saturated; and (d) axial T1-W, TSE, fat-saturated, contrast-enhanced MR images of the right hand show a lobulated mass superficial to the flexor digitorum superficialis of the ring finger in midpalmar space. The mass is isointense (white arrow in a) on T1-W imaging and hyperintense (white arrow in b) on T2-W imaging with punctate susceptibility artefacts within (arrowheads), likely representing phleboliths or flow voids. (d) There is heterogeneous enhancement (black arrow) on the contrast-enhanced image with serpiginous vessels (black arrows in b & c) on the ulnar aspect of the main lesion.
Tenosynovitis is inflammation of the synovial membrane, which surrounds the tendon sheath (Figs.
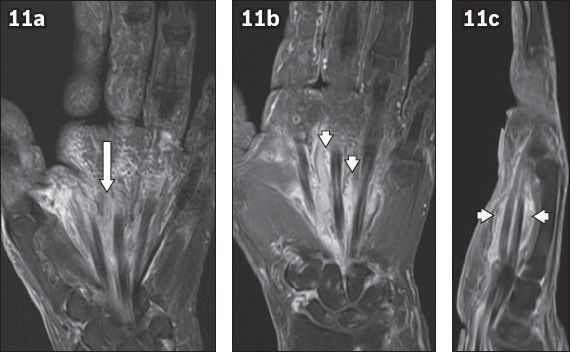
Fig. 11
Tenosynovitis in the palmar space with cellulitis in a 54-year-old woman who presented with painful swelling in her left palm of one week’s duration. (a) Coronal T2-W turbo spin-echo (TSE), fat-saturated; and (b) contrast-enhanced coronal and (c) sagittal T1-W TSE fat-saturated MR images of the left hand. The flexor tendons of the hand from the level of the wrist in the carpal tunnel to the thumb/fingers are thickened and oedematous (white arrow in a). There is significant thickening and enhancement of the tendon sheaths and lumbricals (arrowheads in b & c) on the contrast-enhanced images.
In summary, though lipomas are commonly encountered clinically, deep palmar lipomas are relatively rare. The extent and depth of these deep palmar lipomas can be easily detected and characterised with the use of MR imaging. Understanding neurovascular and tendon relationships through MR imaging can help in surgical planning. Meticulous surgery is curative and provides relief for associated neuropathy.
SMJ-57-425.pdf


