Abstract
A 30-year-old woman presented with a six-month history of left posterior heel pain. Physical examination revealed a tender, inflamed and indurated posterior heel with a visible bony prominence of the posterosuperior aspect of the calcaneus. Lateral ankle radiography showed a prominent left posterosuperior calcaneal tuberosity and thickening of the distal Achilles tendon outline. Magnetic resonance imaging demonstrated high-signal inflammatory fluid in the retrocalcaneal bursa, increased signal intensity and thickening of the Achilles tendon, and prominence of the posterior calcaneus tuberosity with reactive marrow oedema. The findings are consistent with Haglund’s deformity. The patient underwent hind foot surgery after failing a six-month course of conservative therapy. There was no further recurrence of symptoms after surgery. The clinical and radiological features of Haglund’s deformity are described, including a short discussion of other causes of hind foot pain.
CASE PRESENTATION
A 30-year-old woman presented with a six-month history of left posterior heel pain. Physical examination revealed a tender, inflamed and indurated posterior heel with an associated visible bony prominence on the posterosuperior aspect of the calcaneus. Lateral ankle radiography (
Fig. 1
Lateral left ankle radiograph.

Fig. 2
Sagittal inversion-recovery MR image of the left ankle.
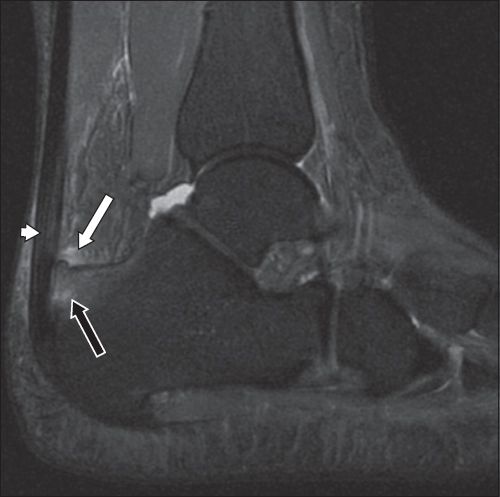
IMAGE INTERPRETATION
The lateral ankle radiograph (
DIAGNOSIS
Haglund’s deformity.
CLINICAL COURSE
The patient was prescribed a course of conservative management that included physiotherapy sessions, analgesics for pain relief and footwear modification. The symptoms persisted after six months and surgical therapy was offered. The patient underwent excision of the Haglund’s deformity and retrocalcaneal bursa, as well as debridement of the inflamed Achilles tendon. She recovered well after surgery, without recurrence of symptoms.
DISCUSSION
Haglund’s deformity, a condition that was first described by Patrik Haglund in 1928, consists of a triad of retrocalcaneal bursitis, Achilles tendinosis and a posterosuperior calcaneal prominence.(1) Although the disease occurs in both genders, it has a female preponderance.(2) It usually affects younger patients, particularly those in their 20s and 30s.(3)
The posterosuperior calcaneal bony prominence, also called Haglund’s disease, is due to an exostosis. Repetitive impingement between this prominence and the deep surface of the Achilles tendon, just above the level of its calcaneal insertion, incites inflammatory change in the tendon. A swollen and inflamed retrocalcaneal bursa that lies between the Achilles tendon and the posterior calcaneus contributes to the pain. Persistent and repetitive irritation leads to the formation and inflammation of an adventitial bursa superficial to the Achilles tendon, which is also called the superficial retrocalcaneal bursa or retro-Achilles bursa (Figs.
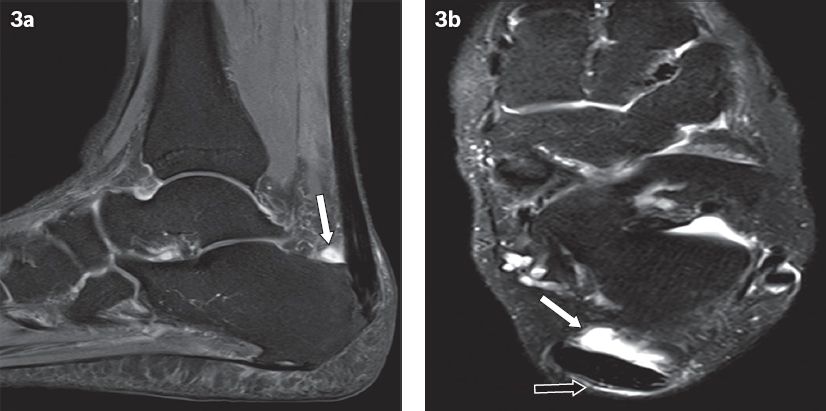
Fig. 3
(a) Sagittal and (b) axial inversion-recovery MR images of the right ankle in a 36-year-old woman with Achilles tendinopathy show prominent retrocalcaneal bursal fluid (white arrows). (b) The presence of adventitial/superficial bursa fluid is also seen posterior to the Achilles tendon (black arrow).
Most patients with posterior heel pain present with localised, painful swelling of soft tissue; some patients may present with a concurrent posterosuperior calcaneal prominence. They may report pain associated with uphill walking and chronic strenuous activity such as long-distance running. Such activities are often aggravated by pressure due to a tight heel counter from ill-fitting footwear or pumps, resulting in ‘pump bumps’. Pain can also arise due to new or worn-out shoes, recent footwear adjustments, and/or an intensification in physical activity or workload.(2) On physical examination, patients may have a tender and erythematous posterosuperolateral heel prominence, usually from retrocalcaneal or sometimes adventitial bursitis. Passive dorsiflexion of the foot may elicit tenderness localised to the bursa or bony prominence. To detect the presence of concomitant tendinopathy, palpation should be performed to localise any area(s) of tenderness along the Achilles tendon; it also helps to confirm the presence of surrounding soft-tissue swelling. An enlarged and inflamed fluid-filled retrocalcaneal bursa can, at times, be felt by simultaneously palpating medially and laterally anterior to the Achilles tendon. More importantly, a ‘squeeze test’ should be carried out in patients with posterior heel pain to examine for the possibility of calcaneal stress fracture. This is done by applying moderate compression, using both palms, to the calcaneal tuberosity.(4) A stress fracture should be suspected when significant tenderness is elicited during this manoeuvre.
Haglund’s deformity is generally thought to be a developmental condition and postulated to be associated with chronic calcaneal apophysitis experienced in childhood.(5) Structural factors implicated in its aetiology include, but are not limited to, a high-arched cavus foot and the presence of a varus heel.(6) A combination of these factors can affect foot dorsiflexion, make the heel more prominent and cause it to be more susceptible to increased pressure from shoe counters and tendons.(4)
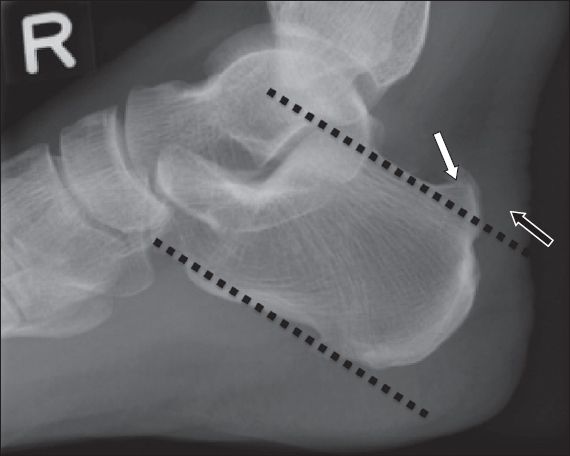
Radiologically, the condition is often initially assessed on plain radiography. Many radiographic parameters such as lines, angles and soft-tissue measurements have been developed to evaluate the relationship among the calcaneal bony prominence, Achilles tendon and retrocalcaneal bursa, and to determine their correlation with Haglund’s disease. These parameters, which are measured on weight-bearing lateral ankle radiography, include the parallel pitch lines, Steffensen and Evensen angle, Fowler-Philip angle (FP angle), calcaneal pitch angle (CP angle) and Chauveaux-Liet angle (CL angle). While no single measurement is completely predictive of the condition, a combination of measurements can increase its diagnostic probability. Singh et al suggested that both parallel pitch lines (
Fig. 4
Right ankle lateral radiograph of a 56-year-old man with hind foot pain shows parallel pitch lines (dotted lines). The bony projection (white arrow) above this line is considered abnormal. Thickening of the distal Achilles tendon is also seen (black arrow).
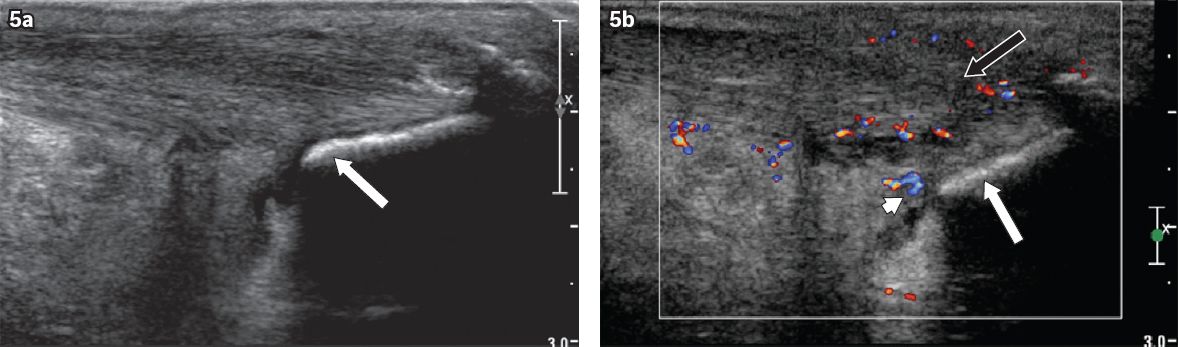
Ultrasonography (US) is another useful modality in the evaluation of Haglund’s disease. It is fast, cheap, free from ionising radiation, and allows dynamic, real-time patient evaluation. A linear, high-frequency (e.g. 13-MHz) transducer is typically employed for examination of the retrocalcaneal area. US can show localised inflammatory changes in the overlying skin and subcutaneous tissues, demonstrate fluid within the retrocalcaneal bursa, and evaluate pathologic abnormalities of the distal Achilles tendon (
Fig. 5
(a) Grey-scale and (b) colour Doppler US images of the left ankle (in longitudinal view) in a symptomatic 55-year-old woman with Haglund’s deformity shows a prominent posterosuperior ‘bump’ represented by thick echogenic line (white arrows). There is thickening, decreased echogenicity and increased vascularity of the distal Achilles tendon, in keeping with tendinopathy (black arrow). The inflamed retrocalcaneal bursa is also demonstrated (arrowhead).
MR imaging is superior in demonstrating the anatomical relationship between the inflamed retrocalcaneal bursa and adjacent Achilles tendon. The retrocalcaneal bursa may be visualised on MR imaging of the normal ankle. However, it is only considered abnormal when its dimensions exceed 6 mm (superior-to-inferior), 3 mm (transverse) and 2 mm (anteroposterior), as suggested by Bottger et al.(10) Although some asymptomatic individuals have a prominent bursa, it has been proven that patients with increased bursal fluid are more likely to be symptomatic.(10) The advantage of MR imaging is the ability to confirm the presence of marrow oedema associated with a prominent posterosuperior calcaneal process in symptomatic patients (
Fig. 6
Sagittal inversion-recovery MR image of the right ankle in a symptomatic 62-year-old man with Haglund’s deformity shows Achilles tendinopathy (arrowhead), a distended fluid-filled retrocalcaneal bursa and prominent posterosuperior calcaneal exostosis with increased marrow signal intensity indicative of oedema (white arrow). There is inflammation of Kager’s fat pad (black arrow).
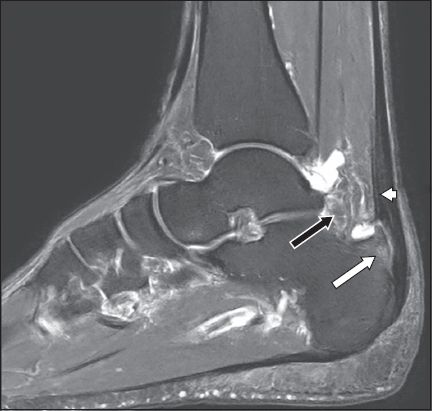
Fig. 7
(a) Sagittal proton density (PD)-weighted, fat-saturated, T1-W and (b) axial PD-weighted, fat-saturated MR images of the left ankle in a 48-year-old man with longitudinal tears of the Achilles tendon on a background of severe non-insertional Achilles tendinopathy. There is thickening and loss of the normal hypointense signal of the tendon. The longitudinal hyperintense signal seen within the mid-tendon substance is in keeping with longitudinal partial tears (white arrows).
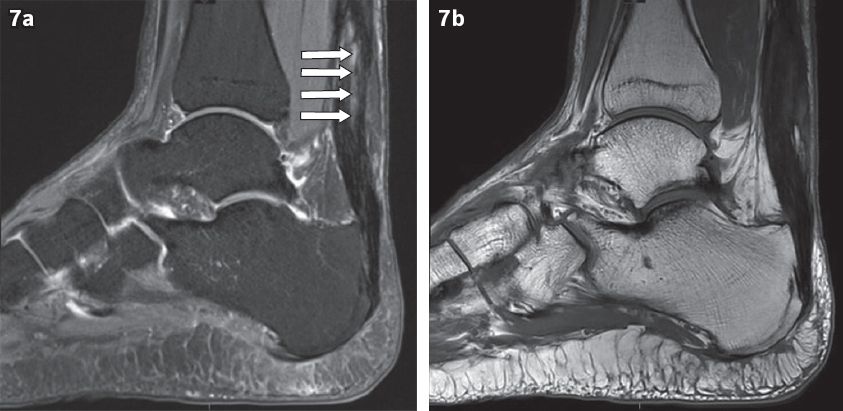
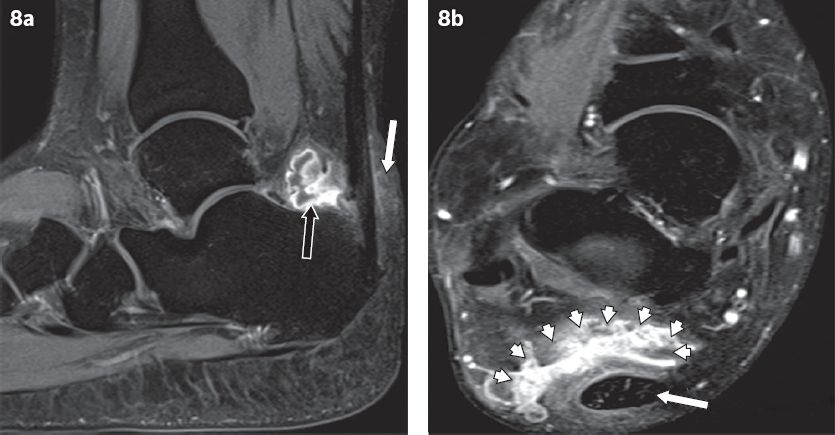
Fig. 8
(a) Sagittal and (b) axial contrast-enhanced, T1-W MR images of the right ankle in a 33-year-old woman show an enlarged retrocalcaneal bursa complicated by abscess formation. A rim-enhancing collection is arising from the retrocalcaneal bursa (black arrow in a). Adjacent Achilles tendinopathy and thickening, reactive enhancement of the soft tissue posterior to the Achilles tendon (white arrow in a) are seen. The retrocalcaneal rim-enhancing collection (arrowheads in b) lies anterior to the Achilles tendon (white arrow in b).
The causes of posterior heel or hind foot pain, which should also be considered in the differential diagnosis, include isolated Achilles tendinopathy and isolated retrocalcaneal bursitis. Other conditions such as rheumatoid arthritis; seronegative spondyloarthropathies, including reactive arthritis (Reiter’s disease) and ankylosing spondylosis causing enthesopathies or marrow oedema; and referred pain from lumbosacral radiculitis are possible differentials, although there is usually known pre-existing disease in such cases. Mimics of Haglund’s disease that were previously reported in the literature include tuberculous infections of the posterior heel and tumours such as osteochondromas.(11,12)
Conservative management is the mainstay of treatment, while surgery may be offered in difficult or complex cases, and those that are refractory to conservative treatment. The main aims of non-surgical management are to reduce underlying inflammatory bursitis and relieve tension in the Achilles tendon. Treatments include modifications to reduce friction between the patient’s footwear and the inflamed retrocalcaneal bursa, using heel lifts and heel pads to reduce pressure on the heel when walking, and performing daily calf-stretching exercises to relieve tension from the Achilles tendon. Non-steroidal anti-inflammatory drugs may be beneficial in reducing pain from underlying inflammatory changes in the posterior heel or Achilles tendinopathy. Percutaneous injection of steroids around the Achilles tendon may also relieve discomfort, but is generally not recommended due to the risk of tendon rupture. Direct injection of steroids into the retrocalcaneal bursa, however, has been reported to relieve symptoms. Sofka et al reported complete relief of symptoms in a patient after a direct US-guided injection of a steroid/anaesthetic mixture into the retrocalcaneal bursa.(9) In most patients, conservative management has a positive outcome, particularly for those without retrocalcaneal bursitis and/or problems associated with the Achilles tendon.(5)
Surgery for Haglund’s disease is indicated when conservative management fails. Depending on the severity of the condition, surgical treatment aims at resection of the posterosuperior calcaneal prominence, excision of the inflamed retrocalcaneal bursa and/or repair of the Achilles tendon, in cases of significant tendinopathy. Many open and arthroscopic-guided techniques have been described, with varying outcomes. Good-to-excellent outcomes have been reported in 73%–97% of heels that underwent open operative procedures.(13) Arthroscopic-guided surgery for Haglund’s disease is usually performed using two or three portal techniques, and good outcomes have been reported in the literature. In one study using a two-portal arthroscopic surgical technique, patients experienced a reduction in time to return to normal activity, low surgical morbidity and high satisfaction rates.(14) For patients, the option of either open or arthroscope-guided surgery is usually dependent on the surgeon’s experience.
In conclusion, while a combination of thorough history-taking and careful clinical examination is required to diagnose Haglund’s disease, imaging is especially helpful in increasing the diagnostic probability of the condition. In particular, advanced imaging modalities such as MR imaging can be used to confidently diagnose and aid in solving difficult or complex clinical problems, including helping to guide surgical management when it is indicated, as well as excluding other disorders that may have a similar presentation. This is important to allow accurate, timely patient management and achieve a desirable clinical outcome.
SMJ-57-522.pdf


