Abstract
A 47-year-old woman who underwent resection of known spinal meningioma at the T1 level returned for postoperative magnetic resonance imaging of the cervical spine. Incidentally, thin-walled structures with signal intensities that are similar to those of cerebrospinal fluid were found to be present in the left neural exit canal at the C7–T1 level and bilateral neural exit canals at the C6–7 level. Imaging findings were in keeping with perineural cysts. Cervical spine perineural cysts are likely underreported, as most of them are asymptomatic. The imaging features and differential diagnoses of perineural cysts are discussed in this article.
CASE PRESENTATION
A 47-year-old woman underwent elective surgery to resect a known intradural tumour at the T1 level. Histology confirmed the diagnosis of spinal meningioma. On follow-up, the patient was well and magnetic resonance (MR) imaging of the cervical spine was performed. What do the images show? What is the diagnosis?
IMAGE INTERPRETATION
The thin-walled structure (black arrows in
Fig. 1
Left parasagittal MR images of the cervical spine on the same plane: (a) precontrast T1-W; (b) postcontrast T1-W; (c) T2-W; and (d) turbo inversion recovery magnitude (TIRM) sequences.
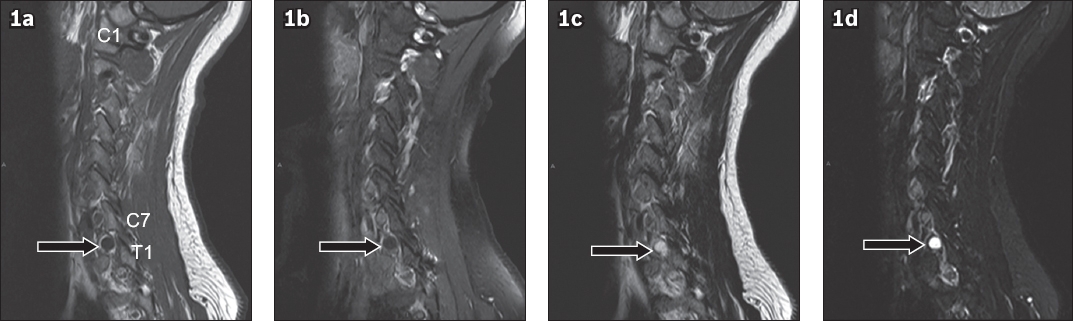
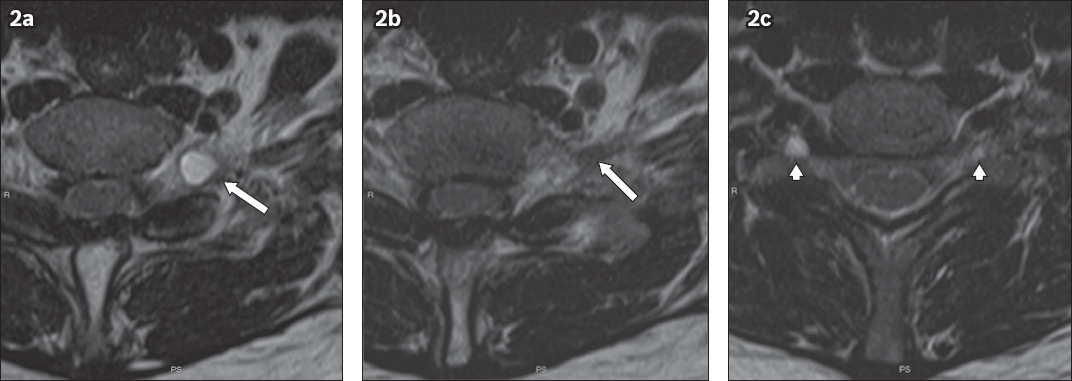
Fig. 2
Contiguous axial T2-W MR images at the level of (a & b) C7–T1 and (c) C6–7.
DIAGNOSIS
Cervical spine perineural cysts.
CLINICAL COURSE
In keeping with the most common presentation of perineural cysts, those found in the patient were asymptomatic and unlikely to be related to prior spinal surgery. They were incidentally detected and remained stable in size, morphology and signal intensities in subsequent surveillance MR imaging studies.
DISCUSSION
Meningeal dilatation of the posterior spinal nerve root sheaths gives rise to perineural cysts, which contain cerebrospinal fluid (CSF) and nerve fibres. When occurring in the lumbosacral spine, they are colloquially known as Tarlov cysts, after Isadore Tarlov, who first described them during a cadaveric study of 30 specimens of filum terminale in 1938.(1) The aetiology of these lesions remains contentious. Some believe that they are congenital in nature,(2,3) while others proposed prior surgery,(2,4) haemorrhage(4) and increased CSF hydrostatic pressure as the possible pathogenesis.(2,5)
It was estimated that 4.6%–9.0% of the adult population has perineural cysts.(5) They are most common in the lower lumbar and sacral segments, particularly the S2 and S3 nerve roots (Figs.
Fig. 3
Axial T2-W MR image of the sacrum shows a left S3 preforaminal perineural cyst, with the S3 nerve root on the cyst wall (white arrow), a distinctive MR imaging feature of a perineural cyst. The perineural cyst enlarges and remodels the left side of the sacral canal (white arrowheads). It is also exerting mass effect by pushing the adjacent S2 nerve root (black arrow) against the borders of the left second sacral foramen.
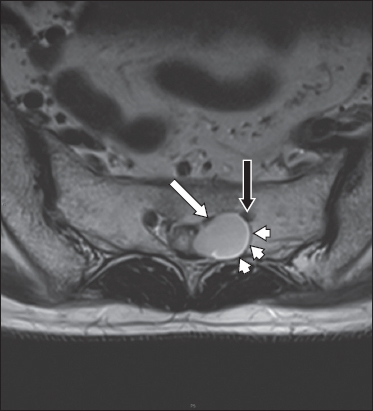
Fig. 4
(a) Sagittal and (b–d) axial T2-W MR images of the lumbosacral spine show perineural cysts that are multiple and bilateral, and involve the S2 and S3 nerve roots. S2 (white arrows) and S3 (black arrows) perineural cysts demonstrate traversing nerve roots within the cysts – another distinctive MR imaging feature of perineural cysts. These are preforaminal in location. Similar to the lesion demonstrated in
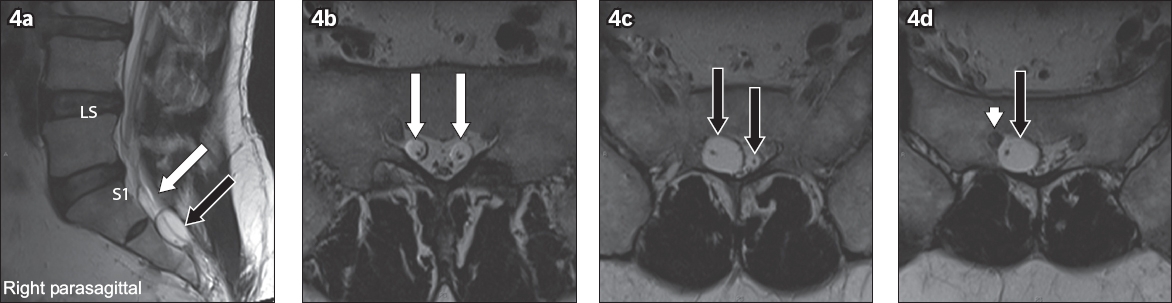
Fig. 5
(a) Coronal TIRM and (b) sagittal T2-W MR images of the lumbosacral spine show a left S1 postforaminal perineural cyst that is multilobulated in appearance. It is entirely within the pelvic cavity and seen close to the uterus (*). The traversing nerve root is better appreciated on the sagittal image (white arrow).
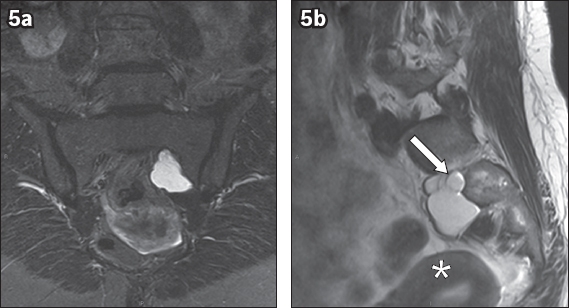
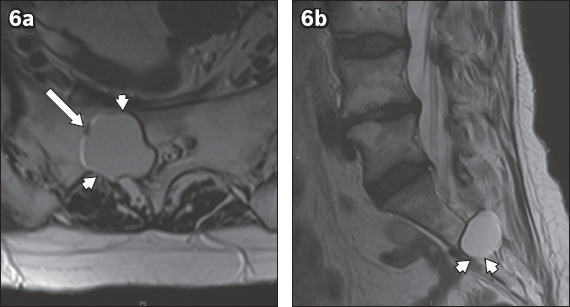
Fig. 6
(a) Axial and (b) sagittal T2-W MR images of the sacrum show a large right S2 transforaminal perineural cyst, with the nerve root seen on the cyst wall (white arrow). Remodelling of the right S2 sacral foramen is demonstrated (white arrowheads). Detection of nerve roots on the cyst wall is understandably more difficult when compared with detection of nerve roots within the cyst (see
Cervical spine perineural cysts were thought to be rare; a literature search found only three case reports on symptomatic lesions(8-10) and one of a cervical spine perineural cyst masquerading as a tumour.(11) There is likely to be underreporting of such cases, as most cervical spine perineural cysts are asymptomatic. We postulate that the development of perineural cysts in our patient may be related to her underlying spinal meningioma. The presence of the meningioma may have hindered CSF flow, possibly resulting in increased CSF hydrostatic pressure, which is one of the proposed pathogeneses mentioned earlier. Due to the lack of cervical spondylosis, these are unlikely to be juxtafacet synovial cysts. Another differential diagnosis is pseudomeningocoele formation from iatrogenic dural tear. However, the multiplicity of lesions seen at different levels makes this differential diagnosis less likely. The main differential diagnoses of perineural cysts are juxtafacet synovial cysts (
Fig. 7
(a & b) Contiguous axial T2-W MR images at the L3–4 level of a 67-year-old man with lower back pain and right-sided radiculopathy. Findings that are related to degeneration are seen, including diffuse disc bulge (broken lines), bilateral facet arthropathy (black arrows) and bilateral thickening of the ligamentum flavum (*). A cystic structure (white arrowhead) with raised T2 signal occupies the right lateral recess, and is likely to impinge on the right descending L4 nerve root. This could explain the patient’s symptoms. In rare instances, communication with the synovial fluid of the facet joint is demonstrated (white arrow), allowing for the diagnosis of juxtafacet synovial cyst to be made with confidence.
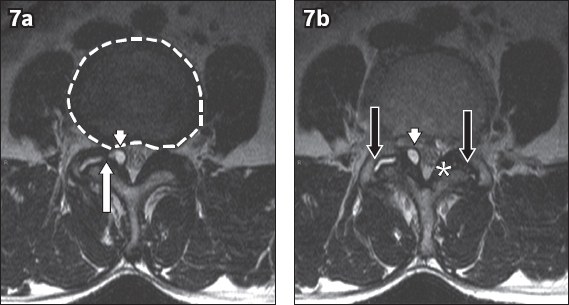
Fig. 8
(a–c) Contiguous postcontrast axial T1-W images at the L1–2 level show a heterogeneously enhancing extradural lesion that occupies the left lateral recess (* in a & d). The lesion returns a mildly raised signal on (d) precontrast T1-W and (e) T2-W images. It extends into the thecal sac (white arrowhead in e), suggesting a neural origin. Laterally, the lesion extends into the left neural exit canal at the L1–2 level (white arrow in c & f). The MR imaging features favour a tumour of neural origin, such as a peripheral nerve sheath tumour (neurofibroma or schwannoma). In some instances, a cystic schwannoma may show a raised T2 signal, which is greater than that demonstrated in this case, simulating the appearance of a cyst. Contrast enhancement is an important distinguishing imaging feature, as both perineural cysts and juxtafacet synovial cysts do not show enhancement.
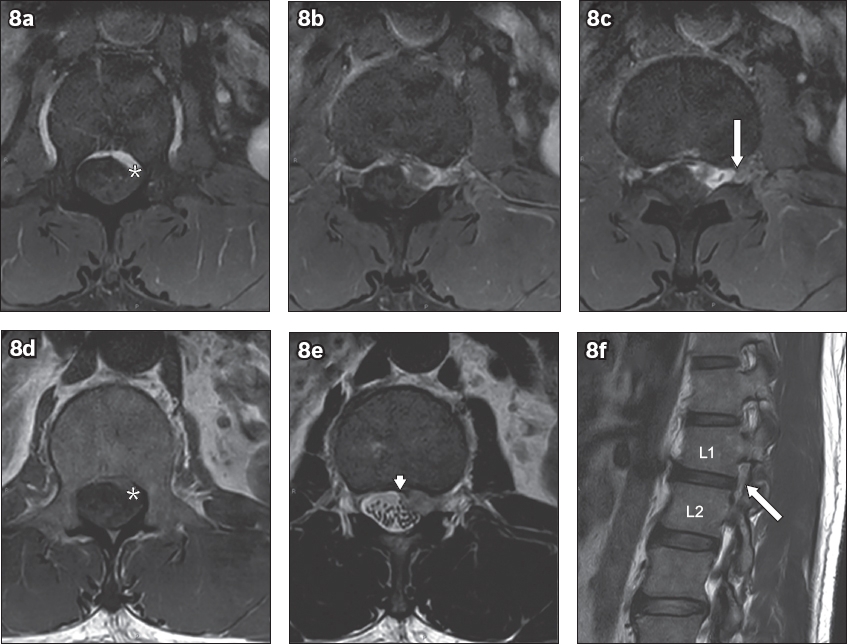
Fig. 9
A 23-year-old motorcyclist involved in a road traffic accident sustained multiple injuries and fractures (including to the bilateral humeri and right distal radius). The patient described diminished sensation, numbness and weakness in the right upper limb. (a & b) Contiguous coronal T2-W images of the right brachial plexus reveal cerebrospinal fluid-containing pouches along the right neural foramina at the C5–6, C6–7 and C7–T1 levels with no exiting nerve root seen within them. This contrasts with the contralateral side, which shows normal exiting nerve roots (arrowheads in a). MR imaging findings are suggestive of post-traumatic pseudomeningocoele with nerve root avulsion. In this setting, MR imaging is also useful to assess for cord abnormality (oedema, haemorrhage, myelomalacia) and associated muscle atrophy or oedema.
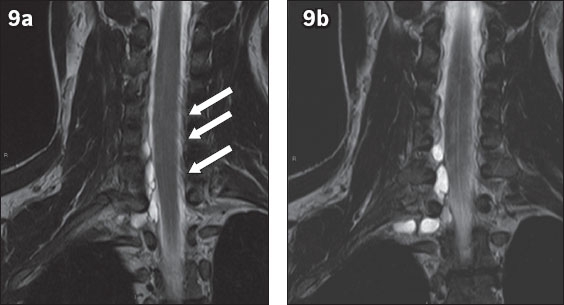
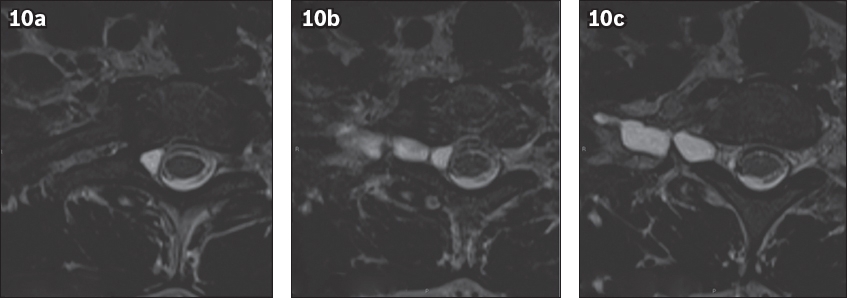
Fig. 10
(a–c) Contiguous axial T2-W images at the C7–T1 level show the pseudomeningocoele along the expected course of the right C8 nerve root. Note that the appearance of
Synovial cysts mimic perineural cysts and vice versa. It is widely accepted that the development of synovial cysts is associated with spondylosis and segmental instability.(12) This is supported by the fact that synovial cysts most frequently occur at the L4–5 level (the site of highest biomechanical spinal motion) followed by the L5–S1 and L3–4 levels, with decreasing frequency.(12) As expected, no synovial cyst has been described in the sacrum,(12) which allows the diagnosis of sacral perineural cysts to be made with confidence. Not surprisingly, synovial cysts are most often seen in the older population (mean age > 60 years).(12) Arising from the facet joint, synovial cysts are seen close to degenerated facet joints, but may extend in any direction.(13) The MR signal intensity of synovial cysts is similar to that of perineural cysts, unless there is proteinaceous or haemorrhagic content present. Infrequently, synovial cysts may calcify and appear hypointense on T1-weighted and T2-weighted images.(14)
Spinal peripheral nerve sheath tumours (PNST) include schwannomas and neurofibromas, which may be benign or malignant. Although schwannomas are more likely to undergo cystic degeneration than neurofibromas, this appearance is rarely seen in the spinal cohort.(15) Nonetheless, the cystic appearance may simulate the imaging appearance of synovial or perineural cysts.(15) Arising from the dorsal sensory roots, the majority of these lesions (70%–75%) are intradural-extramedullary in location, 15% are purely extradural, and a further 15% have both intradural and extradural components – the classic ‘dumbbell’ lesions.(16) In this instance, the administration of MR contrast allows PNST to be distinguished from synovial and perineural cysts. Varying degrees of enhancement have been described, ranging from uniform or heterogeneous to rim enhancement.
The majority (80%) of patients with perineural cysts are asymptomatic.(17) These cysts are often incidentally diagnosed on MR imaging. Commonly encountered symptoms of perineural cysts include sciatica, and bowel and bladder dysfunction.(18) A rare case of sacral insufficiency fracture due to pronounced bone remodelling/thinning has been described by Peh and Evans.(19) Unfortunately, there is no established imaging criterion at present for identifying cysts that are likely to be symptomatic, although some authors opine that larger cysts are more likely to cause symptoms due to stretching of the nerve root filaments or compression against adjacent bone or nerve roots.(2) For symptomatic cases, there is currently no consensus regarding optimal treatment. However, Voyadzis et al observed that patients with perineural cysts that are larger than 1.5 cm and have associated radiculopathy or cauda equina syndrome are likely to benefit the most from surgery.(18)
CONCLUSION
Perineural cysts are incidental findings that are commonly seen in the lumbar and sacral spine. Juxtafacet synovial cysts, the main differential diagnosis, are associated with degenerative facet joints. Care must be taken to distinguish between synovial and perineural cysts, as management of these would differ. The other differential diagnosis is PNST. If this is suspected, the administration of MR contrast is helpful.
SMJ-58-641.pdf


