Abstract
A 23-year-old Indian man presented with shortness of breath and new-onset confusion along with a rash on his chest on Postoperative Day 2, following internal fixation of his femur fracture. Although computed tomography pulmonary angiography was negative for filling defects in the pulmonary vasculature, it showed mosaic attenuation changes with some interlobular septal thickening. Magnetic resonance imaging of the brain showed patchy signal abnormalities, predominantly in the grey-white matter junction region with extensive susceptibility artefacts, consistent with petechial haemorrhages. The laboratory work-up showed thrombocytopenia and anaemia. A diagnosis of fat embolism syndrome was established, based on the clinical presentation combined with laboratory and imaging findings. The clinical and imaging features of fat embolism syndrome are discussed.
CASE PRESENTATION
A 23-year-old Indian man presented to the emergency department following an injury to his right leg. Radiographs showed a fracture of the midshaft of the right femur, for which open reduction and internal fixation was subsequently performed. The patient developed shortness of breath on Postoperative Day 2, along with new-onset confusion and altered mental state. His lungs were clear on the clinical examination, but there was a new rash on the chest. The patient’s condition rapidly deteriorated over the next few hours with progressive worsening of the hypoxia, and he had to be intubated. He also experienced rapid neurological decline with a worsening score on the Glasgow Coma Scale (GCS) from 15 to 11. Blood tests demonstrated mild anaemia with thrombocytopenia. Computed tomography (CT) pulmonary angiography (
Fig. 1
Contrast-enhanced axial CT image (lung window).
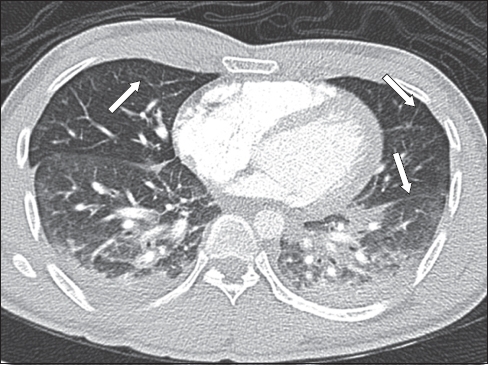
Fig. 2
Axial MR (a) fluid-attenuated inversion recovery (FLAIR) and (b) susceptibility-weighted (SW) images.
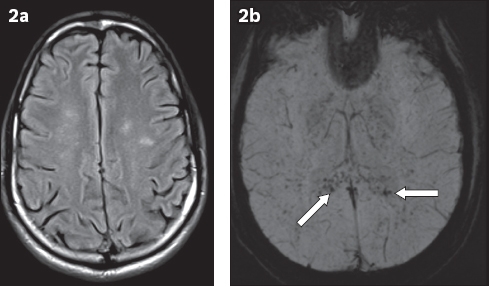
IMAGE INTERPRETATION
The CT axial image of the lung window (
DIAGNOSIS
Fat embolism syndrome (FES).
CLINICAL COURSE
A diagnosis of FES was established on the basis of a combination of the clinical, radiological and laboratory findings. Two-dimensional echocardiography was unremarkable. Cerebrospinal fluid (CSF) analysis and CSF virology were negative. There was gradual improvement in the patient’s condition over the next week, with improvement in the GCS score (from 11 to 15). The patient was successfully extubated and transferred to the general ward. His platelet count improved as well, with some thrombocytosis following surgery, which was attributed to reactive thrombocytosis. The patient was able to ambulate independently with the help of crutches and was subsequently discharged.
DISCUSSION
FES is a well-described syndrome that was first reported in 1962.(1) It is classically associated with fracture of the long bones and is most often seen within the first three days, after the injury.(2) FES is a combination of central nervous system (CNS), respiratory and cutaneous manifestations, with incidence rates ranging from 0.9% to 2.2%.(1) FES can vary in severity and, in some cases, even lead to death, with mortality rates of 13% to 87%.(3) Subclinical fat embolism, seen in almost all cases of fractured long bones, is asymptomatic, self-limiting and does not warrant any treatment.
FES occurs due to dissemination of fatty tissue from the bone marrow as a result of the long-bone fracture. This disseminated marrow fat tissue can get lodged in the pulmonary circulation, leading to respiratory symptoms, typically acute-onset shortness of breath, and hypoxia. The respiratory manifestations are the first to occur and may be followed by neurological and skin findings. The marrow fat emboli can escape to the systemic circulation in patients with right-to-left cardiac shunts. As most patients with FES have no demonstrable cardiac shunts, it has been proposed that small fat vacuoles (< 5 µm) can directly pass from the pulmonary to the systemic circulation.(1) Showers of fat emboli can occur in the brain and occlude small capillaries, causing ischaemia. Typical neurological complaints include headache, acute-onset confusion, disorientation, weakness, convulsions and even coma. Typical lesions of cerebral fat embolism (CFE) involve white matter with relative sparing of grey matter, as the grey matter is rich in vascularity. CNS lesions may be due to ischaemia or secondary to haemorrhages. The white matter lesions occur mainly due to venous sludging and oedema.(1)
There is usually a time lag between the pulmonary and CNS symptoms whose time duration depends on the filter effect (time taken for the passage of emboli from the pulmonary to the systemic circulation). The onset of neurological symptoms is therefore faster and much worse in patients with right-to-left shunts, such as in cases of patent foramen ovale. Neurological recovery depends on the severity of involvement, with some cases leading to brain atrophy and demyelinating changes. However, most neurological issues that occur are transient and often completely reversible. The cutaneous manifestations usually appear after 24 hours and usually disappear within a week. The classical skin manifestation is a petechial rash, typically appearing on the chest, neck, axilla or even the conjunctiva. The rash resolves spontaneously within a few days.
FES is a diagnostic challenge for the clinician. One set of commonly used criteria for diagnosis is by Gurd and Wilson, which states that the clinical diagnosis of FES can be made if at least two major or one major and at least four minor points are met.(4) Major criteria include petechial rash, respiratory insufficiency and cerebral involvement. Minor criteria include tachycardia, fever, retinal changes, jaundice, renal signs, thrombocytopenia, anaemia, fat macroglobulinaemia and high erythrocyte sedimentation rate.
Imaging plays an extremely important role in evaluating patients with suspected FES. Chest radiographs can be non-specific, ranging from the lack of obvious findings to patchy ground-glass opacities. Typical lesions on CT of the thorax include geographic ground-glass opacities, interlobular septal thickening or even nodular opacities.(5,6) Filling defects within the pulmonary arteries are rarely seen.(5) CT of the brain can often be negative or may show subtle hypodense foci, which are non-specific. MR imaging is the diagnostic modality of choice in evaluations of patients with CFE.(7) Findings include patchy or confluent oedema changes, sometimes with restricted diffusion and enhancement on postcontrast evaluation. The lesions usually involve the watershed zone, deep grey matter and white matter; less commonly, there is involvement of the corpus callosum, cerebral peduncles and posterior internal capsule. There may also be petechial haemorrhages in the white matter distribution, as identified on gradient-echo and SW images.(8,9) The patchy lesions in the watershed zone and the deep grey matter have also been described as a ‘starfield pattern’ in 2001, by Parizel et al.(10)
In summary, fat embolism syndrome is a challenging clinical diagnosis that is classically seen in patients following long-bone fractures. Although most cases are subclinical, some can lead to death, especially in the presence of neurological and respiratory complications. MR imaging findings can have overlapping features with other conditions such as hypoxic-ischaemic injury (
Fig. 3
A 42-year-old man found collapsed by the roadside received prolonged resuscitation and was rushed to the emergency department. (a & b) FLAIR MR images show extensive oedema changes, predominantly in the grey matter structures. (c) SW images show no haemorrhage. The imaging findings are consistent with hypoxic-ischaemic injury.
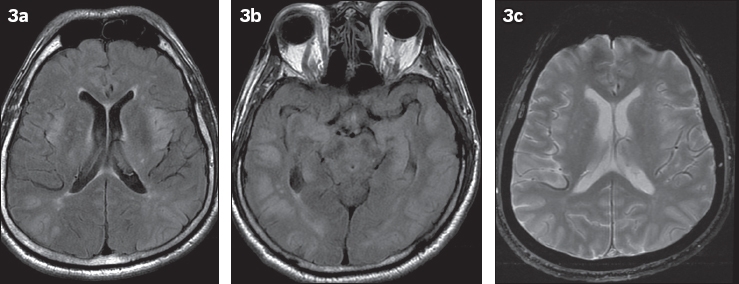
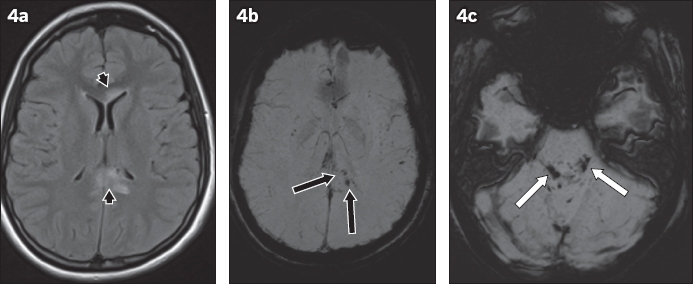
Fig. 4
A 27-year-old man presented at the emergency department with a low Glasgow Coma Scale score following a road traffic accident. Axial (a) FLAIR and (b & c) SW images show oedematous lesions (black arrowheads,
SMJ-59-162.pdf


