Abstract
A 21-year-old man presented with left knee pain and instability that persisted three months after a road traffic accident. Physical examination revealed a positive posterior drawer test. Anterior drawer and pivot tests were negative. Magnetic resonance imaging of the knee demonstrated a complete tear of the posterior cruciate ligament (PCL). Recognition of the normal and injured appearances of the PCL is useful to aid the reader in the detection and characterisation of PCL injuries. Isolated acute PCL tears are usually managed conservatively. However, an active search for associated injuries is essential, as their presence may upstage the patients for surgical management.
CASE PRESENTATION
A 21-year-old man presented with left knee pain and instability from an injury sustained in a road traffic accident three months prior. He had been riding a motorcycle when he self-skidded, landing on the left side of his body. Besides the left knee injury, he had also sustained fractures of the left little and middle fingers (not elaborated here). Physical examination of the left knee revealed a positive posterior drawer test. Anterior drawer and pivot tests were negative. Magnetic resonance (MR) imaging of the left knee was performed. What do the serial medial-to-lateral sagittal images of the knee (
Fig. 1
(a–d) Contiguous sagittal non-fat-suppressed proton density MR images of the left knee.
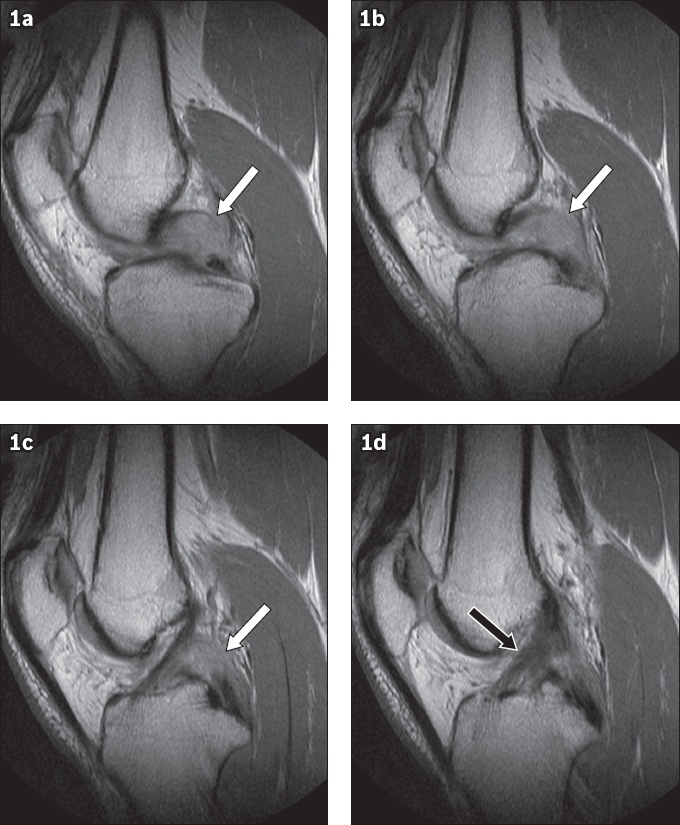
IMAGE INTERPRETATION
Contiguous sagittal non-fat-suppressed proton density (PD) MR images of the knee show complete disruption of the posterior cruciate ligament (PCL) at the mid portion (white arrows, Figs.
DIAGNOSIS
Complete PCL tear.
CLINICAL COURSE
The patient subsequently underwent PCL reconstruction with an allograft. Postoperatively, he was compliant with extensor muscle-strengthening physiotherapy. Mild pain was experienced over the medial aspect of the knee joint, likely from the site of allograft harvesting, and was managed with oral analgesia.
DISCUSSION
The PCL is a dense, fibrous collagen band that originates from the lateral aspect of the medial femoral condyle to insert into the posterior intercondyloid (of PCL) fossa just inferior to the joint line. It is composed of two bundles, the anterolateral and posteromedial bundles, that are tightly bound together, giving it a uniformly low signal intensity on all MR pulse sequences.(1) The PCL is nourished by the middle geniculate artery and innervated by branches of the tibial nerve.(2)
The PCL functions to restrict posterior translation of the tibia in relation to the femur. It also contributes to the restraint of internal rotation (with the knee in flexion of 90° or more).(2) In about 49% of knees, the anterior (Humphrey) and posterior (Wrisberg) meniscofemoral ligaments may be seen, both of which have been reported to contribute to posterior stability in PCL-deficient knees.(3) Along with the anterior cruciate and medial and lateral collateral ligaments, the PCL contributes to overall knee stability and kinematics.(4)
Compared to injuries of the anterior cruciate ligament (ACL), injuries afflicting the PCL are relatively uncommon. About 200,000 cases of ACL injuries are reported per year in the United States, while only approximately 3% of the injured knees have PCL tears.(5) Three common mechanisms of injuries have been proposed: (a) posterior tibial translational force in a flexed knee, (b) exaggerated forceful hyperextension of the knee, or (c) knee rotation in combination with varus or valgus force. The two most common causes are motor vehicle accidents and sports injuries, accounting for about 57% of cases in total.(2)
The PCL is rarely injured in isolation. Instead, a PCL tear is often associated with other ligamental, meniscal and bony injuries: the ACL is involved in about 46% of cases, the medial collateral ligament in 31% of cases and the posterolateral corner complex in 62% of cases.(6) Patterns of bone contusion may suggest the underlying mechanism of injury. For example, bone contusion in the anterior tibial plateau and posterior femoral condyle is commonly observed in dashboard injuries, while bone oedema in the anterior aspects of both the tibial plateau and femoral condyle is suggestive of a hyperextension injury.(7)
A PCL injury is suggested by a classic history, such as posterior knee pain or instability, or positive findings on physical examination such as a posterior sag sign, positive posterior drawer test or positive quadriceps active test.(2) However, the physical examination may be difficult or misleading due to pain, the presence of haemarthrosis, and other concurrent ligamentous injuries limiting assessment.(8) In addition, when the ACL is intact, the PCL can be difficult to evaluate arthroscopically from the anterior approach.(9) Thus, MR imaging can be valuable in bridging the diagnostic gap.
In the sagittal plane, a normal PCL is seen as a well-defined continuous band of low signal intensity (in all pulse sequences) in the intercondylar notch. It is lax and forms a gentle arc pointing posteroinferiorly with the knee being imaged in a position of partial extension. It measures no more than 7 mm in anteroposterior diameter in the sagittal images (
Fig. 2
(a–d) Contiguous sagittal non-fat suppressed proton density MR images of the knee show the normal appearance of the posterior cruciate ligament (white arrows), from a lateral to medial direction.
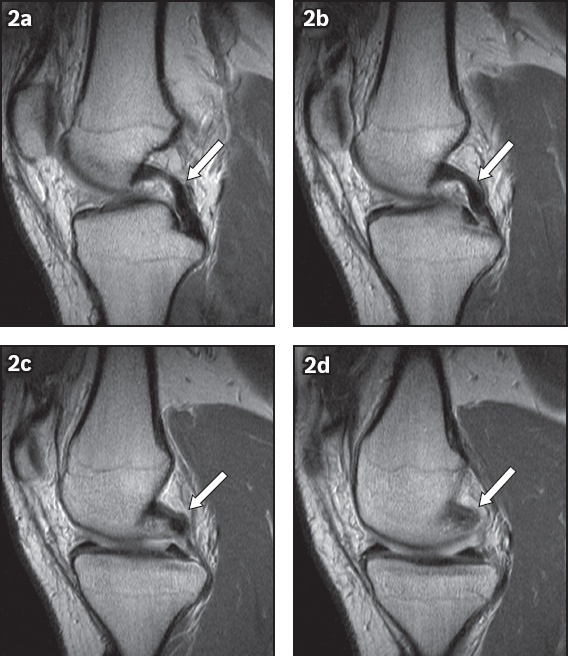
The PCL can be injured with varying degrees of severity, ranging from a sprain to a partial or complete tear. When the PCL measures 7 mm or greater, it is highly suggestive of a tear, with a reported sensitivity of 94% and specificity of 92%.(8) Posterior tibial translation may serve as a valuable secondary sign of PCL tear, especially when it measures more than +2.93 mm in the mid-medial compartment in relation to the mid-lateral compartment.(10) This finding was observed in our patient (
Fig. 3
Contiguous sagittal non-fat suppressed proton density MR images of the left knee of our patient shows the posterior tibial translation measuring about 4–5 mm more in the mid-medial compartment (vertical line in 3a) compared to the mid-lateral compartment (vertical line in 3b).
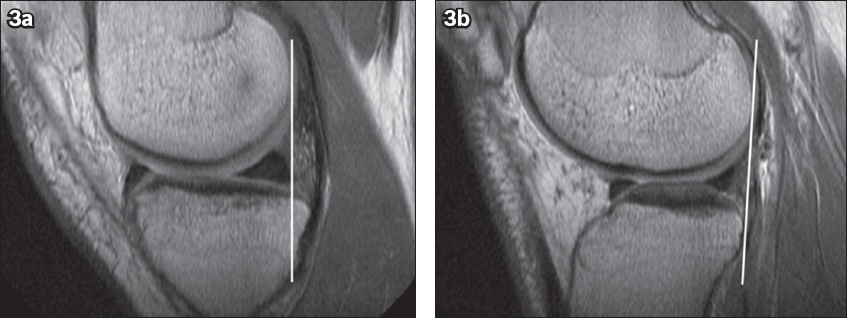
Fig. 4
(a–b) Contiguous sagittal proton density MR images through the intercondylar area show focal thickening and partial thickness fibre disruption in the distal portion of the posterior cruciate ligament (PCL) (arrows in a & b), in keeping with a partial tear. (c) Sagittal T2-W MR image shows corresponding increased intrasubstance signal intensity in the PCL (arrow).
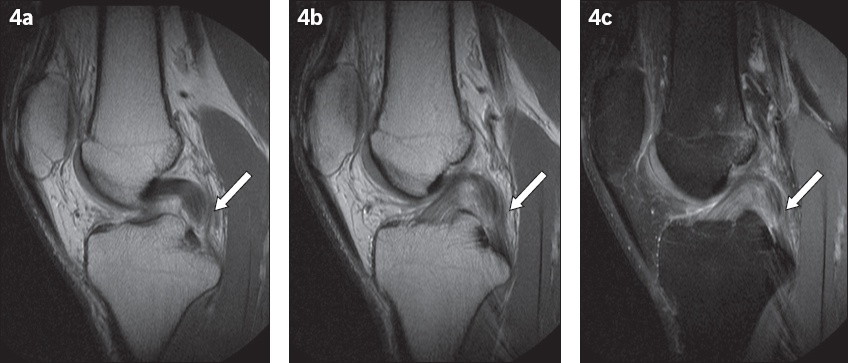
Fig. 5
(a) Sagittal fat-suppressed T2-W and (b) non-fat-suppressed proton density MR images show increased T2 signal intensity in the posterior cruciate ligament (PCL) (arrows), without obvious fibre interruption. The PCL measures less than 7 mm in anteroposterior diameter. Overall features suggest a sprained PCL.
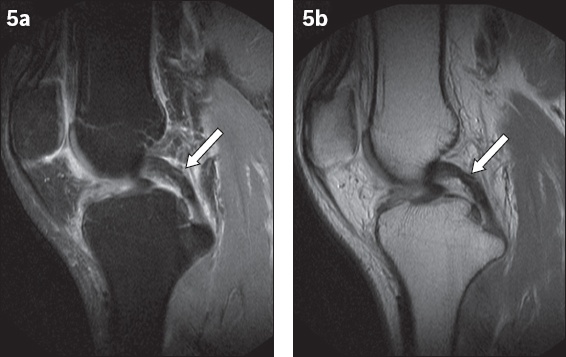
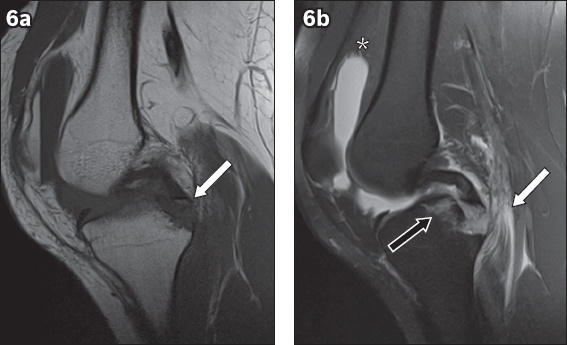
Fig. 6
(a) Sagittal T1-W MR image shows a small displaced bone fragment (arrow) with a signal intensity similar to that of bone marrow attached to the distal end of the posterior cruciate ligament (PCL), consistent with an avulsion fracture of the tibial attachment of the PCL. (b) Sagittal fat-suppressed T2-W MR image further demonstrates acute bone marrow oedema of the proximal tibia (black arrow) related to the aforementioned fracture, soft tissue oedema of the medial gastrocnemius muscle (white arrow) and moderate knee effusion with fat-fluid level in keeping with a lipohaemarthrosis (asterisk).
Details on the treatment of PCL tears is beyond the scope of this article. Nonetheless, the management of PCL tears is generally dependent on two factors: (a) whether they are isolated or combined injuries (together with other ligament or meniscal tears) and (b) whether they are acute or chronic.(2) An isolated PCL tear is usually managed conservatively, as it has an intrinsic ability to heal. The healing process usually occurs with the ligament in a lax position, hence the knee should be immobilised in full extension (for about 2–4 weeks), with bracing applied (to counteract the posterior tibial sagging) and subsequent quadriceps muscle strengthening exercises (to enhance the muscles that compensate for the posterior tibial translation).(2)
Other concomitant ligamentous or meniscal injuries, as well as persistent instability of the knee, are often an indication for surgical treatment. In the case of our patient, although he did not suffer other ligamentous or meniscal injuries, PCL reconstruction was performed in view of his persistent complaint of instability despite conservative treatment. Most techniques involve arthroscopy with either single- or double-bundle reconstruction, using autografts or allografts. Other fixation methods include the use of a trans-tibial tunnel or the tibial inlay technique. In brief, the single-bundle option aims to replace the anterolateral bundle, while double-bundle reconstruction attempts to restore normal knee kinematics by replacing both bundles. Autografts are harvested from the patellar (bone-patellar tendon-bone) or hamstring tendon, while allografts are often retrieved from the Achilles or quadriceps tendons.(2)
CONCLUSION
Recognition of the normal appearance of the PCL and spectrum of PCL injuries is useful for improved diagnosis of a PCL tear. Isolated acute PCL tears are usually managed conservatively. However, the active search for associated injuries should be emphasised, as their presence may upstage the patients for surgical management.
SMJ-60-290.pdf


