Abstract
A 39-year-old man presented with acute left knee pain and swelling. There was limitation of movement of the knee joint. His past medical history was significant for gout. Computed radiography showed bony erosions that were not typical of chronic tophaceous gout. Magnetic resonance (MR) imaging showed focal deposits within the knee joint, which demonstrated isointense signal to muscle on T1-weighted sequence and intermediate signal on proton density (PD) and PD fat-saturated sequences. There was extensive, similar signal abnormality in the cruciate ligaments, popliteus tendon and lateral meniscus. These findings were in keeping with an intra-articular manifestation of chronic tophaceous gout. The clinical presentation and imaging features are herein discussed, with an emphasis on MR imaging.
CASE PRESENTATION
A 39-year-old Malay man presented with acute left knee pain and swelling. There was no history of trauma or fever. On examination, the left knee was warm, swollen and tender. Left knee flexion was limited to 20°. Pain was localised to the medial joint line and there was a small suprapatellar effusion. Lachman’s sign was mildly positive. The collateral ligaments were tested and deemed stable. The rest of the physical examination was unremarkable. No subcutaneous tophus was noted. Serum uric acid levels and erythrocyte sedimentation rate were elevated at 679 µmol/L (normal range 218–578 µmol/L) and 32 mm/hr (normal range 1–10 mm/hr), respectively. His serum white blood cell count was mildly elevated at 10.41 × 109/L (normal range 4.0–10.0 × 109/L).
The patient had an eight-year history of gout, which was previously diagnosed in both knees with joint aspiration demonstrating negatively birefringent needle-shaped crystals. This was in keeping with monosodium urate monohydrate deposition, and was managed with nonsteroidal anti-inflammatory drugs (NSAIDs), colchicine and diet modification. Since then, he had had intermittent acute flares of gout in both knees and was subsequently started on allopurinol. The patient had no history of renal impairment, or clinical or imaging features of hyperparathyroidism.
A clinical diagnosis of acute on chronic gout flare of the left knee was made based on the patient’s presentation. Plain radiographs of the left knee were acquired. Although magnetic resonance (MR) imaging is not considered routine for evaluation of gouty arthritis, given the progressively worsening knee joint movement in our patient, MR imaging was performed to assess for the extent of soft tissue involvement and evaluate for other internal derangements of the joint. What do the radiograph (
Fig. 1
(a) Frontal radiograph of the left knee. (b) Coronal T1-W; (c) sagittal proton density-weighted; and (d) coronal proton density-weighted fat-saturated turbo spin echo MR images of the left knee.
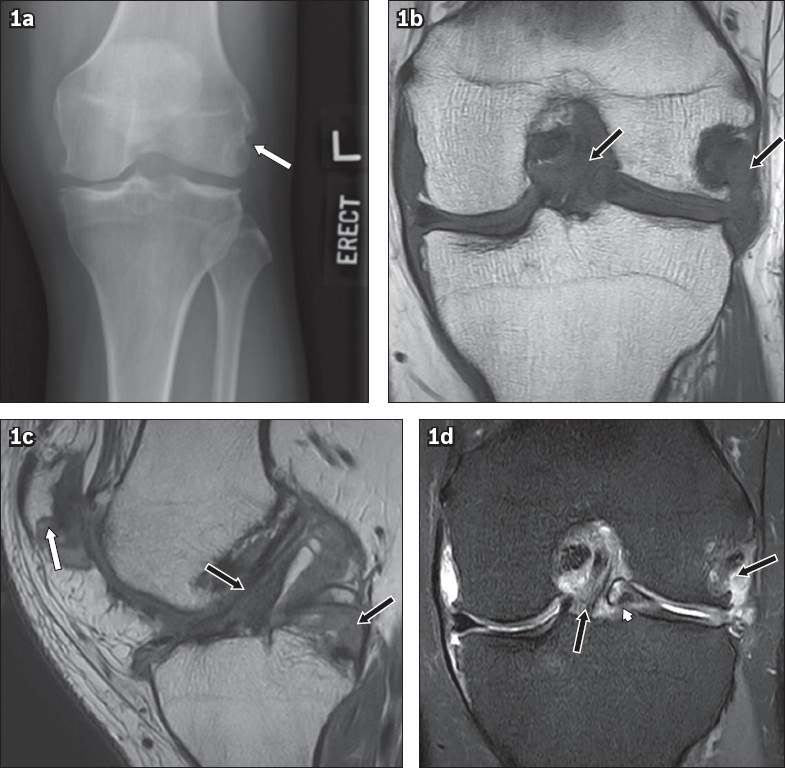
IMAGE INTERPRETATION
The radiograph of the left knee shows a juxta-articular bony erosion at the lateral femoral condyle without sclerotic borders and overhanging margins (arrow,
The MR images show multiple intra-articular gouty deposits demonstrating isointense signal to muscle on T1-weighted sequence (
DIAGNOSIS
Intra-articular chronic tophaceous gout of the knee.
CLINICAL COURSE
The patient was initially treated conservatively with colchicine and NSAIDs. However, as his knee joint still experienced significant limitation of mechanical movement, which greatly hampered his daily activities, arthroscopic debridement was offered to debulk the tophaceous deposits in the left knee. The patient was counselled preoperatively that limitations of knee extension may not fully resolve following surgery. Three months after surgery, the patient remained pain free with no acute flares.
DISCUSSION
Gout is a metabolic disease characterised by chronic elevation of serum uric acid levels. When the concentration of uric acid rises above the physiological saturation limit (approximately 380 µmol/L or 6.4 mg/dL), monosodium urate monohydrate crystals precipitate and are deposited mainly around joints.(1,2) Four clinical stages of gout are recognised: asymptomatic hyperuricaemia, acute gouty arthritis, intercritical gout and chronic tophaceous gout.
A tophus is a pathognomonic lesion of chronic tophaceous gout. Many patients have a history of gout of 10–12 years before these lesions become visible clinically or radiographically.(3,4) The tophus is a focus of precipitated urate that is surrounded by hypervascularised tissue and an intense inflammatory reaction of macrophages, lymphocytes, fibroblasts and foreign body giant cells. Most tophi are located subcutaneously, commonly in the pinna of the ear, olecranon bursa and first metatarsophalangeal joints, and are diagnosed clinically without the need for imaging. However, tophi can also be located predominantly intra-articularly, within tendons, ligaments, bursae, synovial spaces, cartilage and bone.(5,6) Clinical diagnosis is difficult when: there is no clinical stigmata of gout, the patient presents atypically, the patient presents early before radiographic changes have occurred, serum uric acid levels are normal, or when there is a pre-existing significant past medical history necessitating exclusion. Intra-articular gout can mimic infection or neoplasms.(7)
Patients with acute gouty arthritis typically present with monoarticular arthropathy involving acute pain, swelling, and erythema of the affected joint. Such patients are typically evaluated with computed radiography (CR) in the first instance, which may show non-specific soft tissue swelling or joint effusions with no bony changes.(8) In chronic tophaceous gout, typical tophi are deposited in a juxta-articular location. Over time, there is remodelling of the adjacent bone, giving rise to the classical CR findings of well-defined, ‘punched-out’ juxta-articular bony erosions with sclerotic margins and overhanging edges. Soft tissue tophi typically have an asymmetric distribution. The bony erosions are typically extra-articular, but may be intra-articular or para-articular.(8) Tophi are not inherently radio-opaque but may, rarely, calcify when calcium also precipitates within it. There is a lack of periarticular osteopenia and the joint space is typically preserved until late in the disease. These CR findings have 93% specificity for gout.(9)
Although not routine, ultrasonography (US) is increasingly being used in the evaluation of gout or may incidentally detect features of gout. Some US features that are seen in gout include the double contour sign, tophi, bony erosions seen in two planes and a ‘snow storm’ appearance of the synovial fluid. These findings are, however, not specific for gout. The double contour sign refers to a hyperechoic irregular band over articular cartilage that is due to urate crystal deposition. Tophi have been described to be circumscribed, inhomogeneous, hypoechoic or hyperechoic nodular deposits that may be surrounded by a small anechoic rim.(10,11)
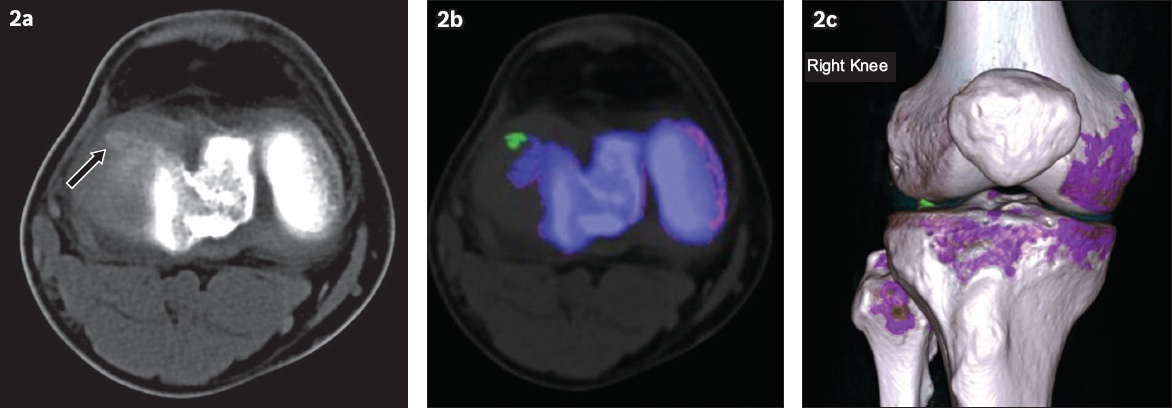
Computed tomography (CT) has been described to be able to detect tophi as hyperdense lesions with an average attenuation of 160 Hounsfield units.(12) CT can also identify bone erosions in gout. The use of dual-energy CT (DECT) in the detection of urate crystals, as described recently, has been shown to be highly sensitive and specific. Using this technique, differences in attenuation can be identified and colour coded, allowing material rich in urate crystals to be differentiated from those rich in calcium. This allows urate crystals to be differentiated from bone or dystrophic calcifications (Figs.
Fig. 2
(a) CT of the right knee in the axial plane shows a faint radiodense focus at the anterolateral corner, likely within the anterior horn of the lateral meniscus (arrow). (b & c) Colour-coded, post-processed images done with dual-energy CT software using a specialised gout algorithm show monosodium urate crystal (green), cortical bone (blue) and trabecular bone (purple). Note the presence of a urate crystal deposit at the anterolateral joint space corresponding to the radiodense focus seen on CT.
MR imaging is not routinely used in the evaluation of chronic tophaceous gout. It may, however, be useful when patients present in an atypical manner or with an atypical joint. MR imaging can also be used as a good problem-solving tool to exclude mimics. A solitary tophus in the absence of articular disease or a tophus with a large intraosseous component may mimic a neoplasm.(13) In addition, the reactive inflammation caused by a tophus may mimic infection.(13) On MR imaging, tophi demonstrate homogeneous isointensity to muscle on T1-weighted sequences (
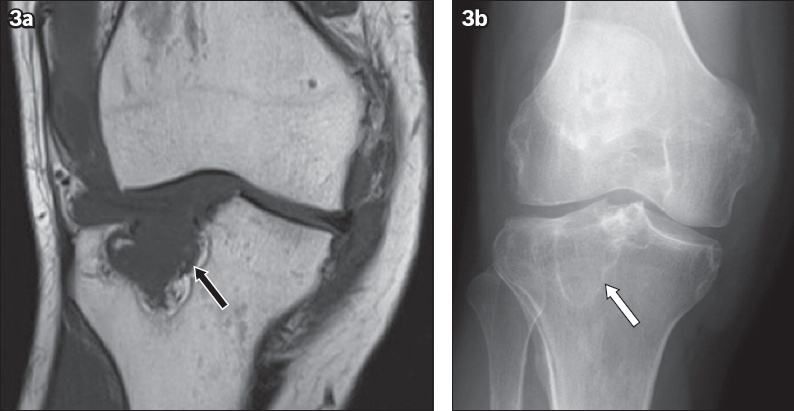
Fig. 3
A 37-year-old patient with end-stage renal failure presented with knee pain. (a) Coronal T1-W turbo spin echo MR image shows increased T1-W isointense soft tissue in the lateral joint space causing erosive deformity of the lateral tibial plateau, in keeping with intra-articular manifestation of chronic tophaceous gout (arrow). (b) Radiograph of the right knee shows a lucent lesion with a narrow zone of transition in the lateral tibial plateau (arrow). Diagnostic considerations include brown tumour or subchondral geode.
Gout typically presents in small peripheral joints and is classically described at the first metatarsophalangeal joint. It affects the knee infrequently. Subcutaneous tophi, a late manifestation of gout, are rarely visible around the knee. This makes clinical diagnosis of gout challenging in the absence of a known history of gout or normal serum uric acid levels. In the knee, gout may involve both periarticular and intra-articular structures. Intra-articular tophi may develop earlier than periarticular tophi, since urate deposition is presumed to precipitate acute gouty arthritis.(14) However, intra-articular tophi are typically occult on CR, thereby underestimating the extent of soft tissue or osseous involvement. Patients typically present with limitation in the range of motion around the knee. For the reasons above, the physical examination and CR findings may be attributed to osteoarthritic degeneration or other causes of internal derangement of the knee rather than intra-articular manifestation of gout. Intra-articular tophi in the knee may be found in the infrapatellar fat pad, anterior joint recess and intercondylar fossae.(14) Involvement of the anterior cruciate ligament and medial patellar plicae has also been described. Intra-articular large tophi causing pressure erosions can be present in the femoral condyles, tibial plateaus and patella (Figs.
Diagnostic considerations of intra-articular lesions in the knee include rheumatoid arthritis, pigmented villonodular synovitis (PVNS), chronic infection, synovial sarcoma and synovial osteochondromatosis.(13) Peripheral enhancement pattern is not typical in rheumatoid arthritis, PVNS or chronic infection. In addition, the susceptibility to haemosiderin deposition that is seen in PVNS differentiates it from intra-articular gout. Synovial sarcomas are typically more T2 hyperintense and may show internal areas of necrosis or cystic changes (Figs.
Fig. 4
(a) Axial T1-W fat-saturated post-contrast and (b) coronal short tau inversion recovery (STIR) sequences show an enhancing STIR hyperintense, slightly lobulated soft-tissue lesion lateral to the distal femur (arrows). No bony erosion was evident. The lesion was subsequently resected, and the histopathological findings revealed synovial sarcoma.
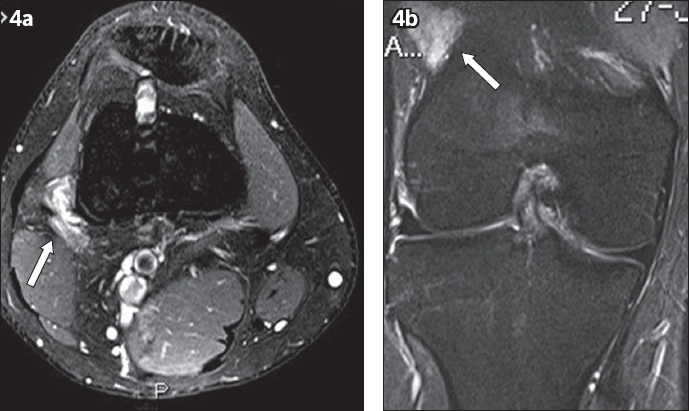
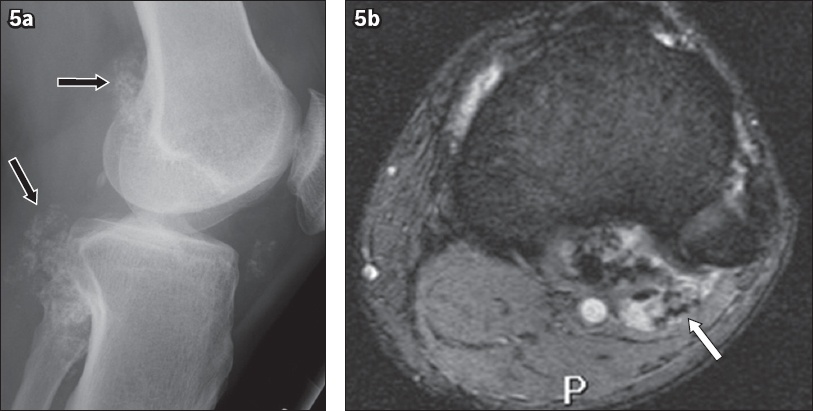
Fig. 5
(a) Lateral radiograph of the left knee shows multiple intra-articular ossified loose bodies (arrows). (b) Axial gradient-recalled echo sequence shows multiple foci of susceptibility, in keeping with synovial osteochondromatosis (arrow).
The mainstay of treatment for gouty tophi consists of diet modification, addressing the underlying cause and medical therapy. Allopurinol is a xanthine oxidase inhibitor that is typically prescribed as part of medical therapy, as it reduces uric acid production. In cases of significant limitation of joint motion or skin breakdown with risk of infection and neurovascular compromise, surgical options may be considered.(15)
In summary, the diagnosis of intra-articular gout is often overlooked and possibly underdiagnosed, especially in the knee. It also often mimics infection or neoplasm on CR or MR imaging. Radiologists who encounter MR findings of homogeneous focal T1 isointense and T2 hypo- to hyperintense deposits in the knee with a homogeneous or peripheral pattern of enhancement, especially in the presence of typical bony erosions, should consider intra-articular gout as a differential diagnosis in the appropriate clinical context. This is because intra-articular gout can develop earlier, before the typical CR changes are noted in chronic tophaceous gout. It would be prudent to suggest checking for correlations with serum uric acid levels and for the involvement of other joints that are typical of gout, as well as suggesting joint fluid aspiration in the first instance rather than recommending surgery.
SMJ-60-507.pdf


