Abstract
A 14-year-old boy presented with left anterior knee pain, which was aggravated by exercise and relieved by rest. On clinical examination, there was tenderness at the tibial tuberosity with reproducible pain on resisted active extension of the knee. Radiographs showed heterotopic ossification of the patellar tendon with irregularity and fragmentation of the tibial tubercle. Clinical and radiological findings were consistent with Osgood-Schlatter disease, which is a traction apophysitis of the tibial tubercle commonly occurring in adolescents. The clinical presentation and imaging features are discussed.
CASE PRESENTATION
A 14-year-old boy presented with anterior left knee pain of two weeks’ duration with no history of trauma. The knee pain was aggravated by exercise and relieved by rest. On physical examination, there was focal tenderness at the left tibial tuberosity, and the pain was reproducible on forced extension of the knee. The rest of the knee examination did not reveal any joint instability. Radiography of the knee was performed (
Fig. 1
(a) Lateral radiograph; (b) sagittal proton density-weighted turbo spin echo sequence; and (c) sagittal proton density-weighted turbo spin echo fat-saturated sequence of the left knee.
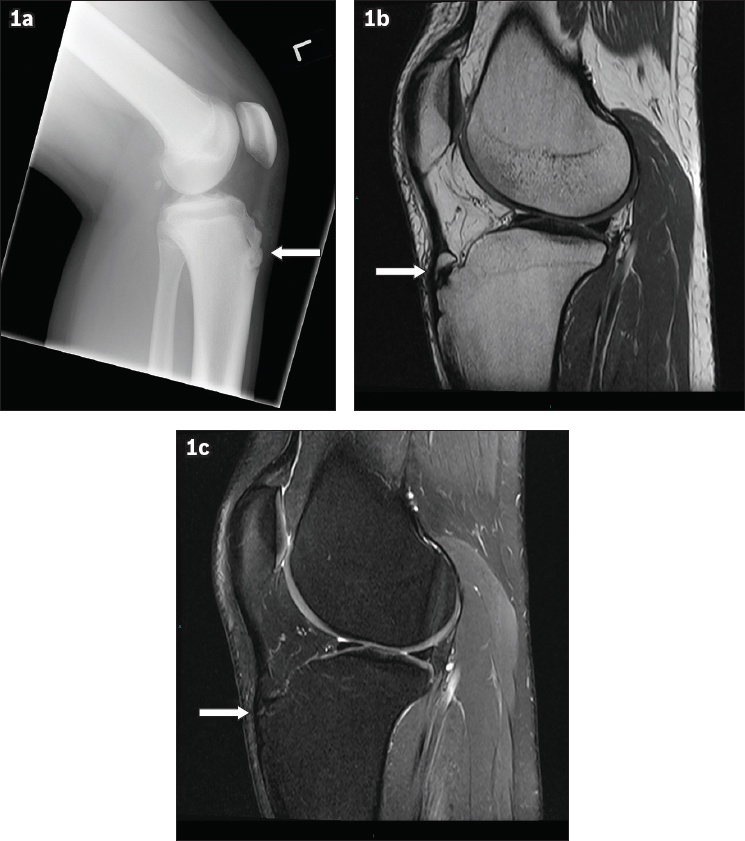
IMAGE INTERPRETATION
Radiograph of the left knee (
Subsequent MR imaging of the knee demonstrates a small ossicle in the distal pre-insertional part of the left patellar tendon, which shows well-defined corticated margins and no identifiable marrow oedema (
DIAGNOSIS
Osgood-Schlatter disease (OSD).
CLINICAL COURSE
The patient was treated conservatively with administration of a short course of oral analgesics along with rest and modification of exercise. The symptoms subsequently resolved with no further functional impairment or pain.
DISCUSSION
OSD is a form of traction osteochondritis involving the tibial tubercle. It was first described in 1903 by Dr Robert Osgood and Dr Carl Schlatter separately, within the same year.(1,2) OSD is characterised clinically by the presence of pain and swelling of the tibial tuberosity in the adolescent patient.(3) It is widely accepted as a traction apophysitis involving the tibial tubercle and the distal aspect of the patellar tendon. There is chronic and repetitive injury to the distal patellar tendon and avulsions of the cartilaginous attachment of the patellar tendon to the secondary ossification centre of the tibial tubercle. Foci of heterotopic ossification may occur when the avulsed cartilage fragments ossify.(3)
OSD typically occurs in the adolescent due to recurrent avulsion and microtrauma of the developing tibial tuberosity. It occurs more commonly in males aged 12–15 years and earlier in females aged 8–12 years due to the earlier onset of the pubertal growth spurt, and may manifest bilaterally in 20%–30% of patients.(4) Higher incidences of OSD are observed in those who are active in sports compared to those who are inactive, at 21% and 4.5%, respectively.(3) A review of 794 published cases in the literature revealed that 72% of all cases of OSD are male.(5) The male predominance has been attributed to greater participation in sports and faster skeletal growth in the male adolescent.
Patients with OSD usually present with pain over the anterior aspect of the knee and tenderness with application of pressure on the tibial tubercle. Any activity requiring contraction of the quadriceps mechanism aggravates the pain, which improves with rest. There may be enlargement of the tibial tuberosity, thickening of the patellar tendon or joint swelling. On physical examination, tenderness is elicited on palpation or application of pressure on the tibial tubercle and patellar tendon. As in our patient, pain is reproducible by resisted active extension of the knee.(3)
The diagnosis of OSD is based on clinical examination, with additional radiographic investigations to exclude fractures or bony tumours.(3) Radiographs of the knee may demonstrate fragmentation, increased density, irregularity or enlargement of the tibial tubercle (
Fig. 2
A 16-year-old boy presented with progressively worsening pain over the left tibial tuberosity. Lateral radiograph of his left knee shows a well-defined ossific fragment at the distal attachment of the patellar (arrow), which is suggestive of Osgood-Schlatter disease.

On MR imaging, the normal patellar tendon should be homogeneously low signal on T1-, T2- and proton densityweighted images. The normal thickness of the patellar tendon increases proximally to distally, but should not exceed 7 mm in thickness.(6) The presence of either focal or diffuse thickening and/or intermediate T1-weighted and T2-weighted signal may represent pathology.(7) MR imaging in the sagittal plane in patients with OSD may reveal enlargement of distal aspects of the patellar tendon, low signal intensity foci of heterotopic ossification, and irregularity or enlargement of the tibial tuberosity. Distention of the deep infrapatellar bursa may be due to the presence of fluid between the deep surface of the patellar tendon and anterior cortex of the tibia. There may be increased signal on T2-weighted images demonstrating oedema at the tibial tuberosity and tibial epiphysis (
Fig. 3
MR imaging of the left knee was performed for a patient with known Osgood-Schlatter disease. (a) Sagittal proton density-weighted turbo spin echo sequence shows bony fragmentation at the tibial tuberosity adjacent to the distal insertion site of the patellar ligament (arrow). (b) Sagittal proton density-weighted turbo spin echo fat-saturated sequence shows bone oedema and cyst formation at the tibial tuberosity (arrow). (c) Sagittal proton density-weighted turbo spin echo fat-saturated sequence done two years later shows resolution of marrow oedema but interval development of intraosseous cystic changes within a bony fragment (arrow) adjacent to the tibial tuberosity.

Ultrasonography may also demonstrate abnormalities surrounding the patellar tendon attachment such as reactive bursitis, patellar tendon lesions, cartilage swelling and neovascularisation at the tibial tuberosity.(8)
Differential diagnoses of OSD include: (a) Sinding-Larsen-Johansson (SJS) disease; (b) Hoffa’s fat pad impingement syndrome; (c) fracture of the tibial tuberosity; (d) infrapatellar bursitis; and (e) patellar tendonitis.
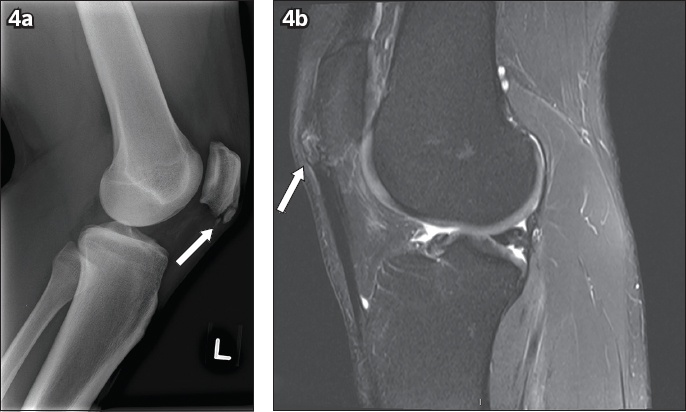
SJS disease is a common cause of anterior knee pain in active adolescents aged 10–13 years. On physical examination, point tenderness can be elicited by direct pressure over the inferior pole of the patella. Symptoms may also be aggravated by jumping. Like OSD, SJS disease is diagnosed clinically, although radiography should be performed to exclude other pathologies. On imaging, there may be ossific fragments within the proximal patellar tendon or at the inferior pole of the patella, which may show oedema, as evidenced by high signal on fluid-sensitive MR sequences (
Fig. 4
Radiography and MR imaging were performed for a patient with Sinding-Larsen-Johansson disease. (a) Lateral radiograph shows ossification within the proximal patellar tendon adjacent to the inferior pole of the patella (arrow). No donor site is seen at the inferior pole of the patella. (b) Sagittal proton density-weighted turbo fat-saturated sequence of the same patient shows ossific fragments at the inferior pole of the patella (arrow). Minimal oedema is noted within the ossific fragments and adjacent patella.
Hoffa’s fat pad impingement syndrome involves impingement of the infrapatellar fat pad. An initial injury or repetitive trauma to the infrapatellar fat pad results in haemorrhage. This leads to inflammation and hypertrophy, predisposing the fat pad to impingement between the femur and tibia (
Fig. 5
A patient presented with anterior knee pain. MR image shows subtle hypertrophy of the Hoffa’s fat pad (arrow), which predisposes it to impingement between the femur and tibia. In the appropriate clinical setting, this may be related to impingement of Hoffa’s fat pad.
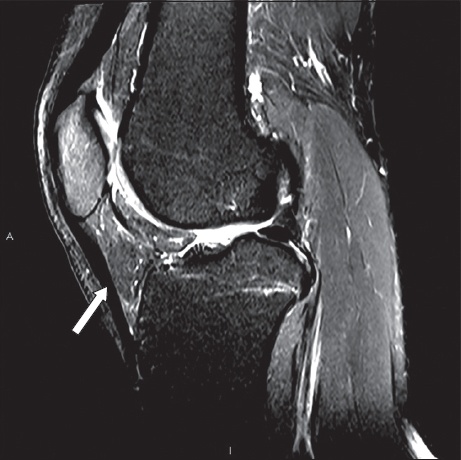
Fig. 6
A patient presented with a history of trauma and anterior knee pain. Lateral knee radiograph shows displaced fracture fragments (arrow) at the anterior aspect of the knee with a donor site in the proximal tibia at the expected site of the tibial tuberosity.

Clinically, it is difficult to differentiate infrapatellar bursitis from OSD, as the pain localises to or near the patellar tendon attachment to the tibial tuberosity. On MR imaging, the tibial tuberosity is normal in appearance but may show an infrapatellar fluid collection.(11) Large collections may be visible as increased soft tissue density on plain radiographs (
Fig. 7
A patient with infrapatellar bursitis presented with localised knee pain anterior to the tibial tubercle. The lateral radiograph shows increased soft tissue density in the infrapatellar region (arrow), likely representing an inflamed/distended infrapatellar bursa.

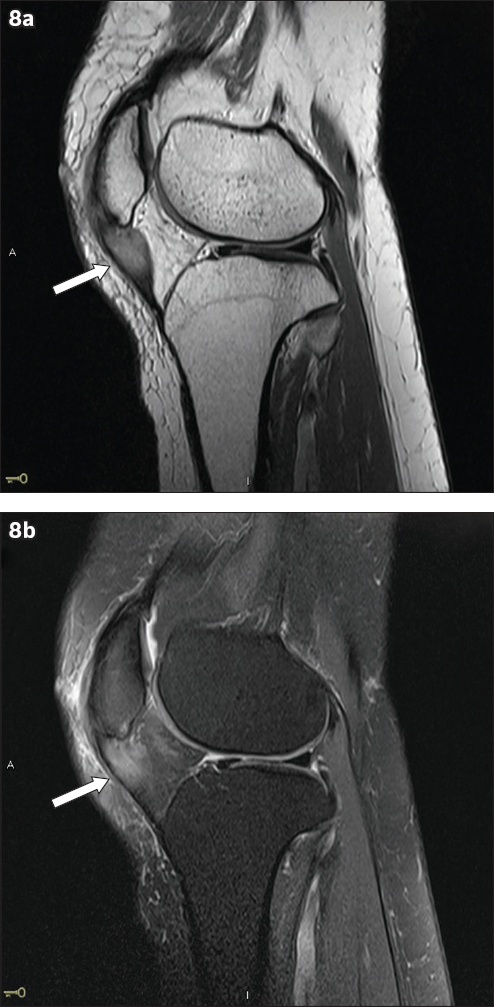
Patellar tendonitis may occur as a complication of OSD. Radiographs may be normal or show soft tissue swelling. On MR imaging, the tibial tuberosity appears normal and there may be increased signal in the patellar tendon (
Fig. 8
A patient presented with anterior knee pain after minor trauma. (a) Sagittal proton density-weighted turbo spin echo sequence shows thickening and increased signal (arrow) in the proximal patellar tendon. (b) Sagittal proton density-weighted turbo spin echo fat-saturated sequence of the same patient shows increased signal (arrow) in the proximal patellar tendon and surrounding infrapatellar fat pad, representing oedema.
Conservative measures consisting of local application of ice packs and oral administration of analgesics comprise the mainstay of therapy. Modification of exercise is suggested with avoidance of strenuous activities. Strengthening and stretching exercises may also help. Protective pads that are worn over the tibial tubercle may help to avoid direct trauma to the tibia tubercle, although cast immobilisation is not advised, as wasting of the quadriceps muscle may occur. Surgical management may be considered in patients when conservative measures have failed and after fusion of the tibial growth plate.(3) Surgical management is rarely required for unresolved OSD. In cases where there are persistent symptoms after skeletal maturity, surgical treatment may be advocated with good outcomes and without long-term deleterious effects.(12) One study showed promising results for hyperosmolar dextrose injection together with lidocaine over the apophysis and patellar tendon origin, demonstrating subsequent improvement of symptoms, although more research is needed before this procedure can be routinely recommended.(13) In general, OSD tends to be self-limiting with resolution of symptoms in more than 90% of patients and good overall prognosis with non-operative treatment.
SMJ-60-615.pdf


