Abstract
A 56-year-old man presented to the emergency department with acute upper abdominal pain and mild leucocytosis. The pain was not relieved by intravenous analgesia. Computed tomography of the abdomen and pelvis demonstrated a focal area of fat stranding with a thin peripheral rim of high attenuation and a punctate central hyperdense dot in the vicinity of the falciform ligament. The diagnosis of focal infarction of the falciform ligament fatty appendage was made based on the imaging findings. The patient responded well to conservative management and was discharged for outpatient follow-up. Focal infarction of the falciform ligament fatty appendage is extremely rare and can mimic various causes of acute abdomen that require emergency surgery. Hence, correct radiological diagnosis is essential to avoid unnecessary surgical intervention. We herein discuss the similarities and differences with other common companion cases such as epiploic appendagitis and omental infarction.
CASE PRESENTATION
A 56-year-old man presented to the emergency department (ED) with a three-day history of pain in the epigastric and right hypochondrial regions of the abdomen. The pain was aggravated by deep inspiration and movement. There was no nausea, vomiting or associated gastrointestinal symptom. Physical examination revealed tenderness in the same regions as reported. There was no guarding or rebound tenderness. The patient had normal vital signs. Laboratory tests revealed mild leucocytosis of 11.33 × 109/L (normal range 3.82–9.91 × 109/L). Liver function test and serum amylase and renal panel showed normal results. An erect chest radiograph showed no subphrenic free air. Intravenous tramadol was administered for pain relief, but the pain persisted despite a period of observation. Computed tomography (CT) of the abdomen and pelvis (
Fig. 1
(a) Sagittal and (b) axial contrast-enhanced CT image of the abdomen and pelvis.
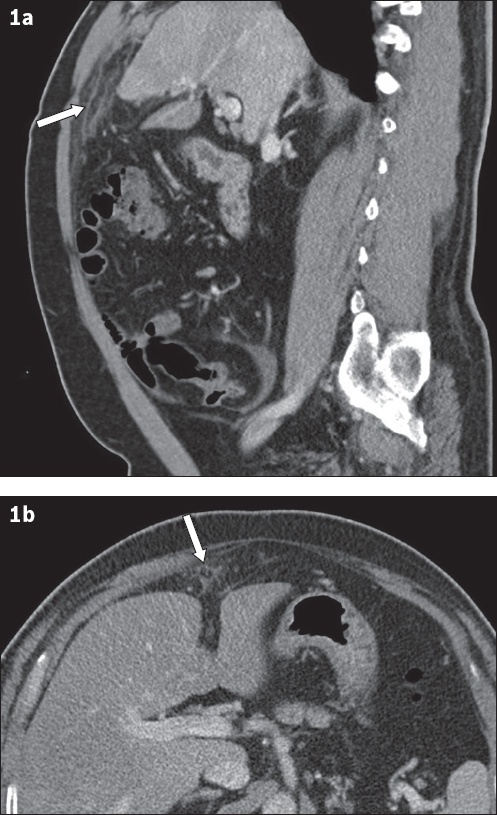
IMAGE INTERPRETATION
The sagittal contrast-enhanced CT image of the abdomen and pelvis (
DIAGNOSIS
Focal infarction of the falciform ligament fatty appendage.
CLINICAL COURSE
The patient was managed conservatively. He was prescribed oral etoricoxib, a nonsteroidal anti-inflammatory drug (NSAID). The pain improved after NSAID administration and his vital signs remained normal. He was subsequently discharged with a prescription of a different oral NSAID, diclofenac, and was followed up in the outpatient surgery clinic.
DISCUSSION
Intraperitoneal focal fat infarction (IFFI) has been used to describe focal lipomatous tissue necrosis in various anatomical locations.(1-3) The more common causes of IFFI include epiploic appendagitis and omental infarction. These conditions have been extensively reported in the literature. However, focal infarction of the fatty appendage of the falciform ligament is extremely rare, with less than 20 cases reported to date.(1) IFFI is usually self-limiting and resolves spontaneously. Most patients improve with conservative management and surgical intervention is not required.(2)
The falciform ligament is a double-layered peritoneal fold that attaches the anterior part of the liver to the ventral abdominal wall and inferior diaphragmatic surface. It is a useful anatomical landmark separating the left lobe of the liver into lateral and medial segments. It contains the ligamentum teres, obliterated umbilical vein and extraperitoneal fat (or fatty appendages). The arterial supply to the falciform ligament is via a vessel originating from the left inferior phrenic artery and middle segmental artery of the liver.(4) The veins of the falciform ligament drain into the left inferior phrenic vein.(4)
Focal infarction of the falciform ligament fatty appendage was first described on imaging in 2001.(5) It is attributed to torsion of the fat appendage of the falciform ligament and thrombosis of its central vein, leading to fat necrosis and infarction.(5) Patients commonly present with acute abdominal pain that either localises to the epigastrium or right upper quadrant of the abdomen. These symptoms closely mimic other causes of acute abdomen, such as acute cholecystitis. Despite severe abdominal pain, laboratory tests are usually normal or reveal mild inflammatory changes.
An unambiguous diagnosis of focal infarction of the falciform ligament fatty appendage can be made with CT. CT images typically demonstrate a focal area of fat stranding with a thin peripheral rim of high attenuation (the aforementioned ‘hyperattenuating rim’ sign) in the vicinity of the falciform ligament. This is explained by torsion of the fatty appendage, contributing to fat necrosis manifesting as fat inflammation. The presence of a high-attenuated central focus (the ‘central dot’ sign) that corresponds to the thrombosed vessel can be helpful to the diagnosis.(2)
The diagnosis of focal infarction of the falciform ligament fatty appendage can potentially be missed by inexperienced radiologists if only axial CT images are interpreted, because the abnormal findings may be subtle, as depicted in this case. However, the imaging features are often distinct in the sagittal plane. Hence, multiplanar reconstruction and interpretation are recommended if subtle abnormalities are seen around the anterior perihepatic space in the axial CT images.(1)
Ultrasonography investigation of focal infarction of the falciform ligament fatty appendage usually demonstrates a hyperechoic, non-compressible, slightly heterogeneous mass at the site of tenderness.(6) There is usually absence of vascular flow on colour Doppler interrogation, which is a helpful feature to differentiate it from other infective or inflammatory conditions such as abscess and phlegmon.(2) Bedside ultrasonography is useful as the first-line investigation to exclude alternative diagnoses such as gallstones and acute cholecystitis.
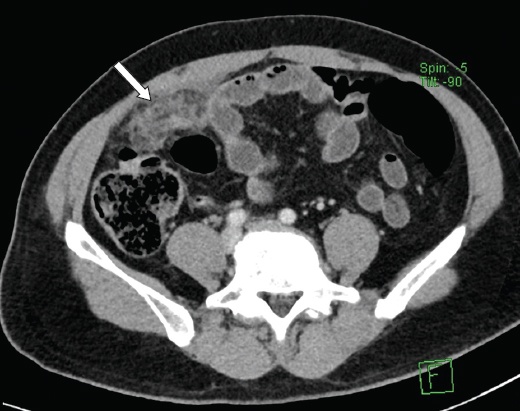
Epiploic appendages are small outpouchings of the visceral peritoneum that contain adipose tissues and small blood vessels, and are attached to the serosal surface of the colon via a vascular stalk. They measure from 0.5 cm to 5 cm in length. Depending on the location of the involved appendages, the clinical presentation can mimic appendicitis and cholecystitis (if located around the right hemicolon) or diverticulitis (if located around the left hemicolon). The CT features of epiploic appendagitis are identical to those of focal infarction of the falciform ligament fatty appendage – encapsulated fat inflammation with a central dot representing a thrombosed vessel. The difference is that for epiploic appendagitis, the site of abnormalities is in close proximity to the colon and more often involves the descending colon(7) (
Fig. 2
Axial contrast-enhanced CT image of the abdomen and pelvis in a patient shows an ovoid-encapsulated fat inflammation, surrounding inflammatory changes and the ‘central dot’ sign anterior to the descending colon (arrow), in keeping with epiploic appendagitis.

Omental infarction typically presents on the right side of the abdomen. It is hypothesised that the right lower portion of the omentum has an anomalous and fragile blood supply, which is consequently susceptible to infarction.(8) Clinically, omental infarction can mimic surgical conditions such as acute cholecystitis or appendicitis. On CT, omental infarction is seen as a solitary non-enhancing encapsulated fatty mass (usually > 5 cm) with heterogeneous attenuation, often located in the lower right quadrant of the abdomen. It usually lacks the feature of a high-attenuating rim, as commonly seen in epiploic appendagitis and focal fat infarction involving the appendages of the falciform ligament (
Fig. 3
Axial contrast-enhanced CT image of the abdomen and pelvis in a patient shows focal mass-like fat stranding at the greater omentum in the right lower abdomen (arrow), in keeping with omental infarction.
In conclusion, focal infarction of the falciform ligament fatty appendage can mimic a variety of conditions that warrant surgical intervention in patients presenting to the ED with acute abdomen. However, radiological diagnosis with CT is often unequivocal. Improved awareness of this condition among radiologists and referring clinicians can serve to avoid unnecessary investigations and surgery.
SMJ-61-18.pdf


