CASE PRESENTATION
A 53-year-old woman presented to the emergency department with pain and swelling in the left ring finger for three months that had worsened after she accidentally hit her finger against the edge of a table. She had no constitutional symptoms and no significant medical history except for diabetes mellitus. Clinical examination revealed localised swelling and tenderness over the proximal phalanx of the left ring finger. Initial laboratory results showed a total white blood cell count of 8.3 (normal range [NR] 4.0–10.0) × 103/mL, C-reactive protein level of 0.4 (NR < 3.0 mg/L), serum phosphate level of 1.27 (NR 0.65–1.65 mmol/L) and serum calcium level of 2.34 (NR 2.1–2.6 mmol/L). Plain radiography of the left ring finger was performed at the initial presentation at the emergency department (
Fig. 1
Posteroanterior radiographs of the left ring finger at (a) the time of presentation and (b) follow-up one month later.
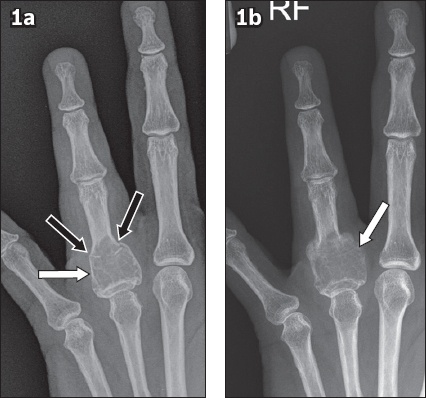
Fig. 2
(a) Coronal turbo inversion recovery magnitude, (b) coronal gradient recovery echo, (c) sagittal proton density, and (d) contrast-enhanced fat-suppressed axial T1-weighted MR images of the left ring finger.
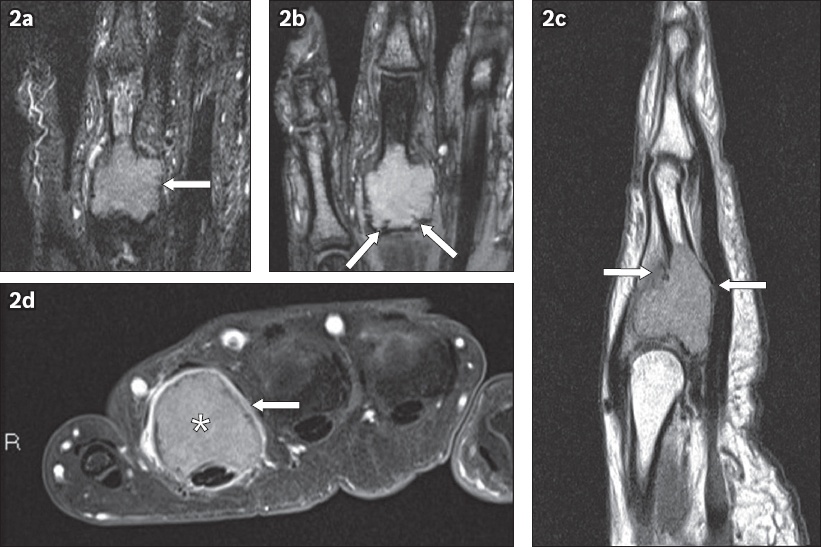
IMAGE INTERPRETATION
The plain radiograph obtained at the initial presentation (
The follow-up radiograph obtained a month later (
Overall, the radiograph and MR findings favoured an aggressive primary bone tumour, in particular a GCT of the proximal phalanx. An aggressive chondroid tumour was considered less likely due to the absence of typical chondroid matrix mineralisation on radiographs and lower-than-expected T2-weighted signal return from the lesion on MR imaging.
DIAGNOSIS
Giant cell tumour of the left ring finger proximal phalanx.
CLINICAL COURSE
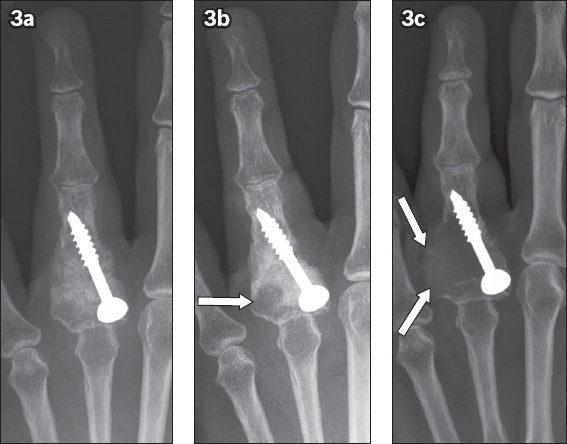
The patient underwent whole-body 99m-technetium bone scintigraphy and computed tomography (CT) of the chest, abdomen and pelvis. Bone scintigraphy revealed increased radiotracer uptake at the site of the known lesion. There was no synchronous bony lesion or evidence of pulmonary metastasis. The patient was surgically treated with open biopsy, curettage, bone grafting, and partially threaded cancellous screw fixation of the left ring finger proximal phalanx. Biopsy showed lesional tissue composed of sheets of cells, including epithelioid histiocyte-like stromal cells, spindled stromal cells and numerous giant cells compatible with a GCT. Follow-up radiography performed within six months following the initial surgery showed a recurrent lytic lesion with a progressive increase in size and cortical destruction (
Fig. 3
Follow-up posteroanterior radiographs obtained in the (a) immediate postoperative period following curettage, bone grafting and partially threaded cancellous screw fixation, as well as at (b) three months and (c) six months following the initial surgery show a progressive increase in the size of a lytic lesion at the base of the little finger proximal phalanx with cortical destruction (arrows) suggestive of tumour recurrence.
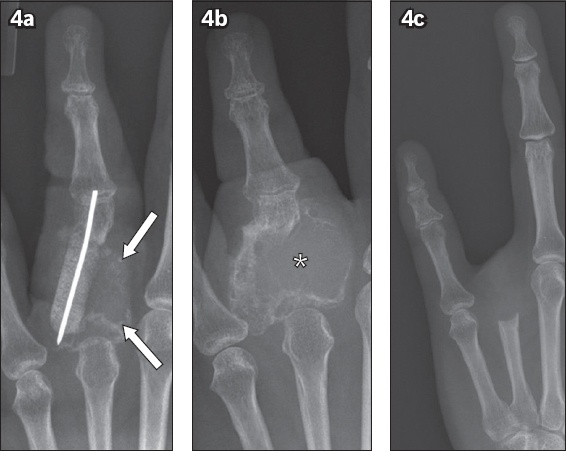
The patient subsequently underwent extensive curettage and bone grafting with K-wire fixation of the left ring finger proximal phalanx. Intraoperative findings showed recurrent GCT involving > 80% of the native proximal phalanx. Repeated recurrence of the tumour within a year of the second resection was diagnosed on subsequent follow-up radiography, and the patient eventually underwent left ring finger amputation (
Fig. 4
Follow-up posteroanterior radiographs: (a) following removal of the partially threaded cancellous screw, extensive curettage, bone grafting and K-wire fixation show recurrent lytic lesion (arrows); (b) six months following the removal of the K-wire show an increase in the size of the recurrent lytic lesion (asterisk); and (c) following amputation of the left ring finger.
DISCUSSION
GCT of the bone is a benign but locally aggressive tumour accounting for 5% of all primary bone tumours and 20% of benign bone tumours. The tumour is composed of numerous osteoclast-type giant cells seen on a background of uniform mononuclear stromal cells.(1) Previously known as osteoclastoma, the term GCT was first coined by Sir Astley Paston Cooper in 1818 and has remained as the accepted nomenclature. Approximately 80% of cases occur between the ages of 20 and 50 years, with a slight female predilection.(1)
GCT most commonly occurs around the knee joint, affecting either the distal femur or proximal tibia. The distal radius is the second most common site. In the spine, the sacrum is commonly involved, representing 8% of cases. Other infrequent sites are flat bones such as the ribs as well as bones of the hands and feet.(1) The tumour usually begins in the metaphysis and extends into the subarticular region. It can be completely metaphyseal in location, although this is rare and is seen in only 1% of cases.
GCT of the hand is rare, with a reported incidence of approximately 2%. The unique clinical features of this tumour in the hands are that it behaves more aggressively and has a higher rate of tumour recurrence in comparison to GCT at other sites, with reported tumour recurrence usually occurring within a year of the initial diagnosis.(2) Commonly reported sites in the hand include the metacarpals, followed by the phalanges of the digits and, rarely, the thumb (
Fig. 5
Giant cell tumour in a 20-year-old man. (a) Posteroanterior radiograph shows a lytic lesion with internal septations in the distal aspect of the thumb proximal phalanx (arrow). (b) Coronal turbo inversion recovery magnitude MR image shows a heterogeneous, intermediate signal intensity appearance of the tumour with thin linear hypointense internal septation (arrow). (c) Sagittal proton density MR image of the tumour (asterisk) shows extraosseous soft tissue extension with involvement of the thumb interphalangeal joint (white arrow), overlying extensor tendon slip (black arrow) and bulging of the underlying flexor pollicis longus tendon (arrowheads). Axial (d) pre- and (e) post-contrast-enhanced T1-weighted MR images show avid post-contrast enhancement of the tumour (arrows).
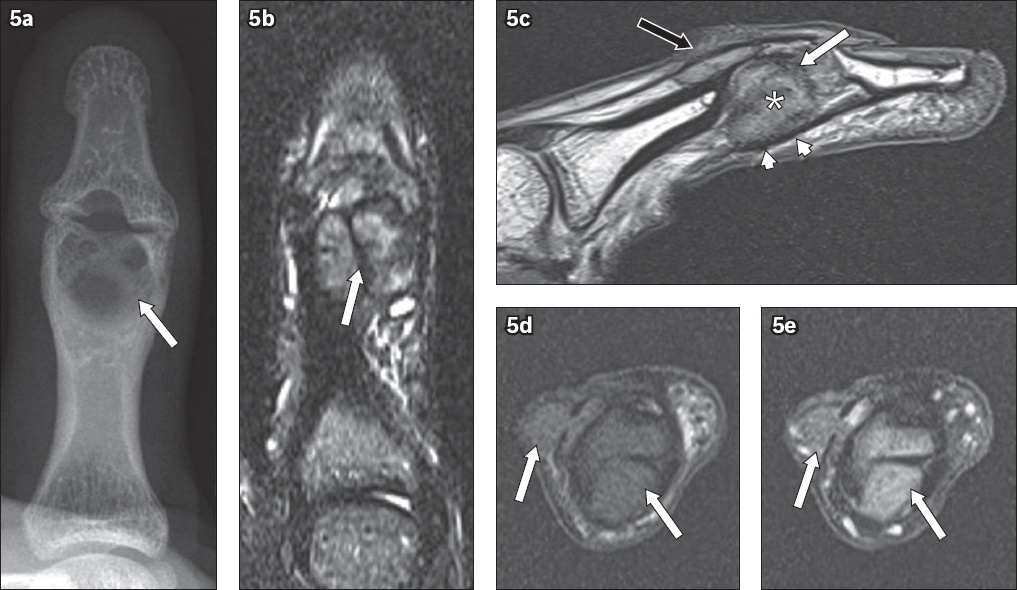
The imaging findings of GCT in the hand are similar to those of GCT in the long bones. The typical radiographic features are an expansile, geographic lytic lesion in the subarticular or epi-metaphyseal region, associated with cortical thinning or erosion, and non-sclerotic margins. Internal septations within the lesion give rise to the characteristic ‘soap bubble’ appearance.(1,5) There is typically no significant periosteal reaction. These tumours tend to grow rapidly with invasion into adjacent soft tissues. CT is useful for assessing the tumour margins and the presence of a pathological fracture, which may be occult on radiography.(5) MR imaging is superior in delineating the extent of the tumour as well as in determining the presence of an extraosseous soft tissue component or adjacent joint involvement. The solid component of GCT is usually of intermediate signal intensity on T1-weighted images and of low signal intensity on T2-weighted images due to haemosiderin deposition within the tumour.(6) While not exclusive, the low signal intensity of GCT on T2-weighted images is, however, useful in differentiating this tumour from the majority of other tumours of the digits, which usually show high signal intensity on T2-weighted images.(6) GCT typically demonstrates post-contrast heterogeneous enhancement, although homogeneous enhancement may be observed in smaller lesions. The finding of cystic areas containing fluid-fluid levels in a GCT raises the possibility of secondary aneurysmal bone cyst (ABC) formation.(1,6) Bone scintigraphy usually demonstrates diffusely increased radiotracer uptake by the lesion or peripherally increased radiotracer uptake with central photopenia (‘donut’ sign).(5)
GCT can be multicentric in less than 1% of patients, and this tends to occur more often in the small bones of the hands and feet.(1) GCT metastases to the lungs are uncommon (1%–6% of cases) and have been reported in cases of GCT involving the hand.(1,7) As such, it is imperative that all patients diagnosed with GCT undergo a bone scan and chest CT as part of the diagnostic workup.
Treatment options for GCT of the hand include curettage, curettage with bone grafting, wide resection with reconstruction and amputation. Relatively high recurrence rates have been observed following curettage (with or without bone grafting) for GCT of the hand.(8) Denosumab, a chemotherapeutic drug, has shown promising results as an adjuvant treatment to reduce the recurrence rate.(1)
The differential diagnoses for a lytic lesion in the small bones of the hand include benign lesions such as enchondroma, ABC, brown tumour of hyperparathyroidism and giant cell reparative granuloma. Primary malignant lesions and bony metastases of the hand are infrequently encountered. Other differential diagnoses include infection and crystal deposition disease, such as gout.(9)
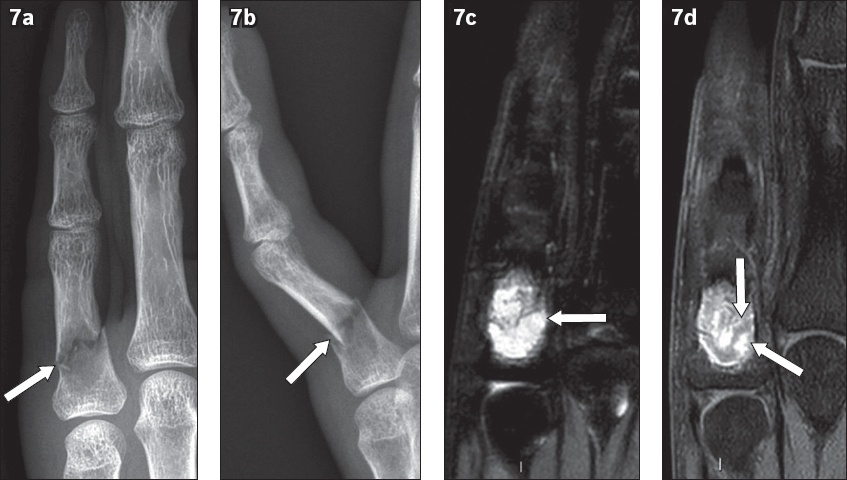
GCT of the hand can be easily misdiagnosed as enchondroma, which represents the most common benign bone tumour of the hands. Enchondroma is a benign cartilaginous tumour that is typically seen as a centrally placed, well-defined expansile lytic lesion with endosteal scalloping or cortical thinning, as well as ‘stippled’ (dot-like) or ‘ring and arc’ matrix calcification in the majority of cases (
Fig. 6
(a) Frontal radiograph of an enchondroma in the right thumb proximal phalanx of a 24-year-old with ‘dot-like’ or ‘stippled’ matrix calcifications (arrows). (b) Frontal radiograph of an enchondroma in the left middle finger proximal phalanx of a 52-year-old man with ‘ring’ (black arrow) and ‘arc’ (white arrows) matrix calcifications.
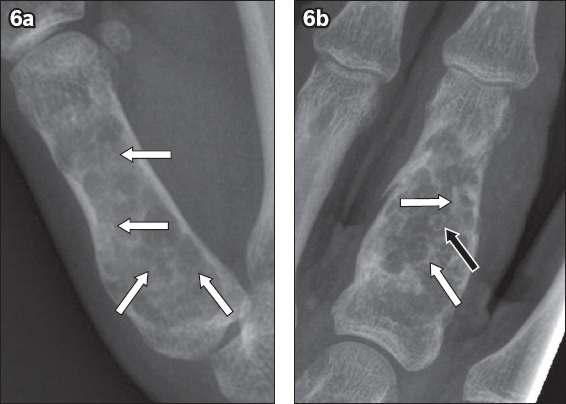
Fig. 7
Enchondroma in a 31-year-old man. (a) Frontal and (b) lateral radiographs show a well-defined lytic lesion in the left little finger proximal phalanx complicated by a pathological fracture (arrows). (c) Coronal turbo inversion recovery magnitude (TIRM) and (d) contrast-enhanced fat-suppressed T1-weighted MR images of the little finger show a marked TIRM (heavily T2-weighted) hyperintense lesion (arrow in
An ABC of the hand, a benign but locally aggressive lesion consisting of blood-filled spaces, represents approximately 5% of benign bone tumours of the hand. These tumours may occur in patients at any age but are typically discovered in patients younger than 30 years of age. ABC usually arises as an expansile lucent lesion in the metaphysis and commonly invades the epiphysis if closure of the physis has occurred. Thin internal septations may be present, giving rise to a ‘soap bubble’ appearance, but there is no mineralised matrix. MR imaging demonstrates intralesional fluid-fluid levels that are consistent with, but not exclusive to, ABCs.(9,11)
A giant cell reparative granuloma (GCRG) is a reactive process of unknown aetiology, although it is postulated to be the sequela of trauma or intratumoral haemorrhage. It is clinically and histologically distinct from GCT. The most common site in the hand for this lesion is the metaphysis or diaphysis of the phalanges. The appearance of GCRG on radiography is an expansile, lytic lesion with expansile remodelling and cortical thinning. Intralesional septation is also typical, but the presence of matrix mineralisation is unusual.(11,12)
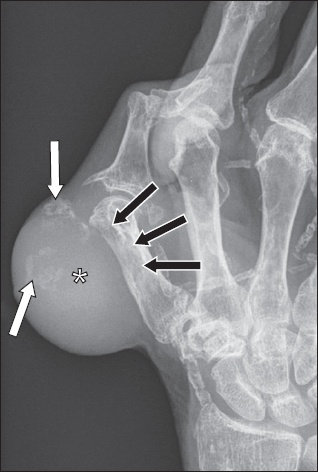
Chondrosarcoma is the most common primary malignant tumour of the hand. The proximal phalanges of the hand are the preferred sites of occurrence. It usually presents as a large, expansile and locally aggressive tumour with cortical destruction, extraosseous soft tissue component and chondroid matrix mineralisation (
Fig. 8
Chondrosarcoma in an 84-year-old man. Posteroanterior radiograph shows an aggressive osteolytic lesion (black arrows) arising from the first metacarpal, which is associated with a large extraosseous soft tissue component (asterisk) and matrix chondroid calcifications (white arrows).
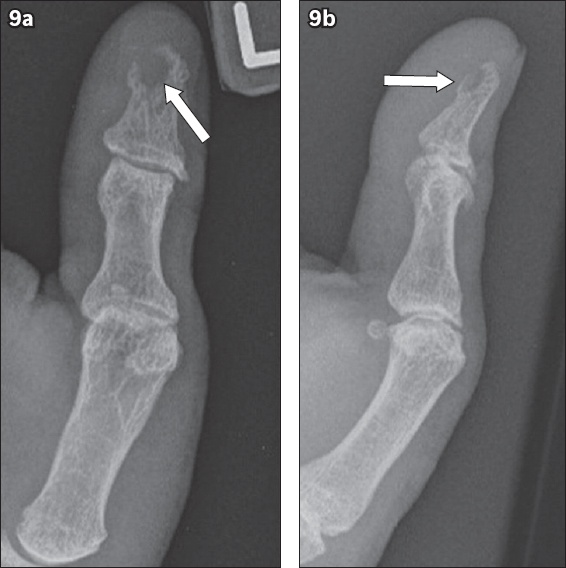
Bone metastases to the hands are quite rare and most commonly originate from primary bronchogenic, renal and breast carcinomas (
Fig. 9
Bony metastasis in a 61-year-old man with known metastatic bronchogenic carcinoma. (a) Posteroanterior and (b) oblique radiographs of the left thumb show a lytic lesion (arrows) with cortical destruction at the volar aspect of the distal phalangeal tuft. The diagnosis was confirmed histologically.
Brown tumour resulting from hyperparathyroidism, either primary or secondary, occurs due to excessive osteoclastic activity, which results in the formation of destructive bony lesions composed of osteoclasts, multinucleated giant cells and haemorrhage. They appear as expansile, lytic or mixed lytic-sclerotic lesions,(13) and if present in the hand, are more commonly seen in the phalanges and may be multiple. The presence of classical radiographic features of hyperparathyroidism in the hand, such as subperiosteal bone resorption along the radial margins of the proximal and middle phalanges of the index and middle fingers, may aid in the diagnosis of these tumours.
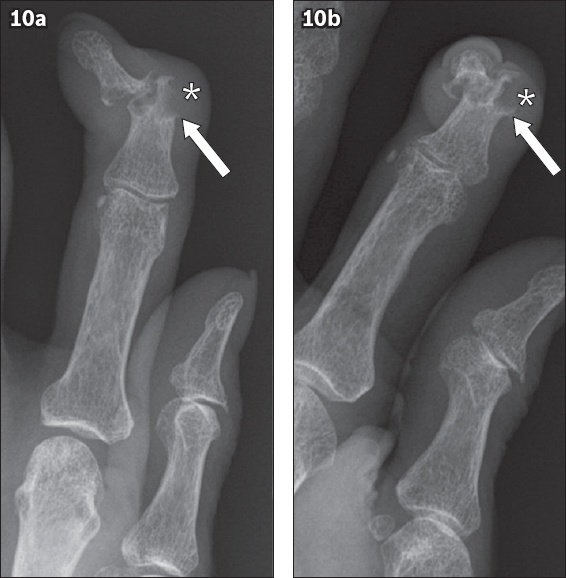
Tophaceous gout typically causes well-circumscribed, punched out lytic lesions in the juxta-articular region with classic overhanging bony margins (
Fig. 10
Chronic tophaceous gout in a 76-year-old woman. (a) Posteroanterior and (b) oblique radiographs of the left index finger show a juxta-articular erosion at the middle phalanx with sclerotic and distinctive overhanging margins (arrows), as well as adjacent soft tissue swelling due to a gouty tophus (asterisks).
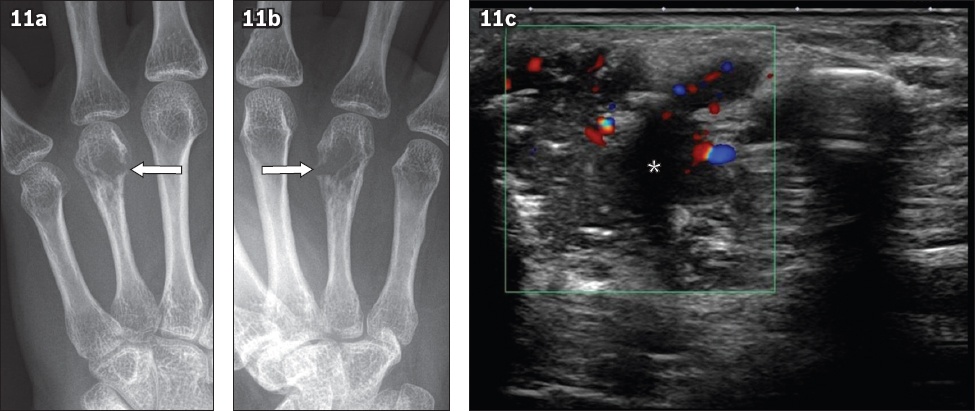
Occasionally, infections can produce aggressive osteolytic lesions in the hand (
Fig. 11
Tuberculous dactylitis in a 39-year-old woman. Radiographs in the (a) frontal and (b) ball catcher’s view of the left middle finger show an ill-defined osteolytic lesion in the fourth metacarpal head and neck with cortical destruction (arrows). (c) Targeted US image of this site in the transverse plane shows a heterogeneous hypoechoic mass with internal vascularity (asterisk). Histological and microbiological analyses were used to confirm the diagnosis.
To conclude, GCT of the hands is a rare, benign but locally aggressive tumour with a higher rate of tumour recurrence in comparison to GCT at other sites. Imaging plays an essential role in the accurate diagnosis and management of this tumour. Knowledge of the differential diagnoses of GCT of the hand would be useful to the reporting radiologist and referring clinician in the diagnostic workup of such patients.
SMJ-62-81.pdf


