CASE PRESENTATION
A 14-year-old girl with no significant past medical history presented to our institution’s sports medicine clinic for right groin pain following uphill running during a physical education class at school. Clinical examination revealed tenderness at the right anterior superior iliac spine (ASIS), anterior inferior iliac spine (AIIS) and pubic symphysis, with painful internal rotation.
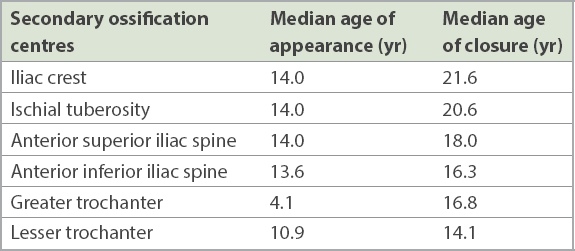
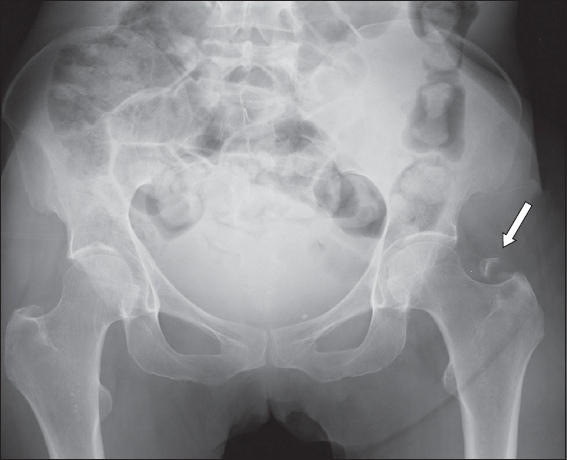
Pelvic radiography (
Fig. 1
Anteroposterior pelvic radiograph of a 14-year-old girl who complained of right hip pain following running in school.
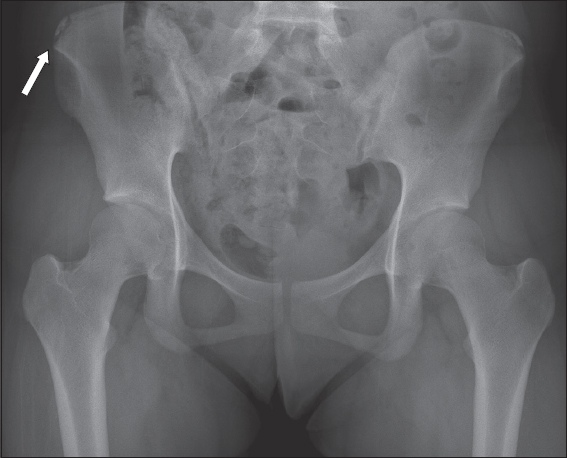
Fig. 2
(a) Coronal T2-W fat-suppressed (FS) MR image of the pelvis and (b) axial T2-W FS MR image of the right hemipelvis.
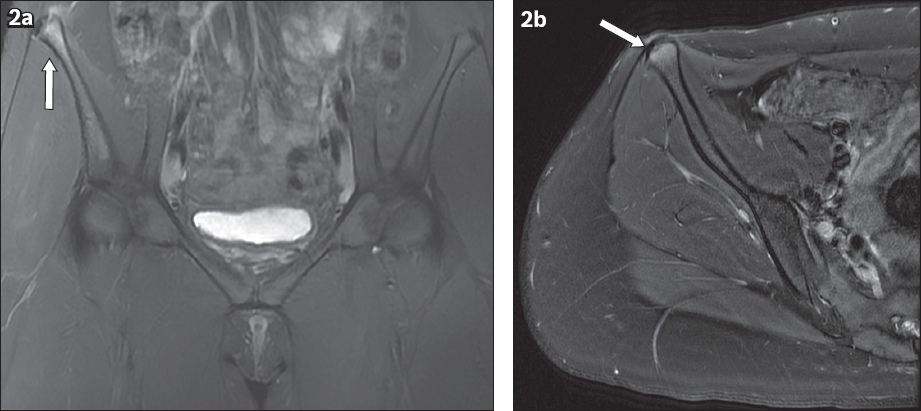
IMAGE INTERPRETATION
The anteroposterior pelvic radiograph (
The coronal (
DIAGNOSIS
Right iliac crest apophysitis.
CLINICAL COURSE
The patient was managed conservatively with analgesia and physiotherapy, and was advised to avoid running temporarily. Her symptoms subsequently improved, and she could gradually return to her baseline activities after 8–12 weeks.
Following physiotherapy and rehabilitation, the patient underwent repeat MR imaging of the pelvis (
Fig. 3
(a) Coronal T2-W short tau inversion recovery (STIR) and (b) axial T2-W FS MR images of the right hemipelvis show resolution of the oedema within the abdominal muscles (arrows), with minimal bone marrow oedema in the iliac crest.
DISCUSSION
The bony pelvis develops from three primary ossification centres, namely the ilium, ischium and pubis, which fuse at the triradiate cartilage at approximately 12–14 years of age.(1) The apophyses are sites of attachment or origin of muscles that function as secondary growth centres, contributing to the shape or size of the bone but not to its length.(2)
The apophyses in the pelvis include the iliac crest, ischium, ASIS, AIIS, pubic tubercle, angle of pubis and ischial spine. The iliac crest apophysis is the attachment site for the lateral abdominal muscles (internal and external obliques, and transverse abdominis), gluteus muscles and tensor fascia latae.
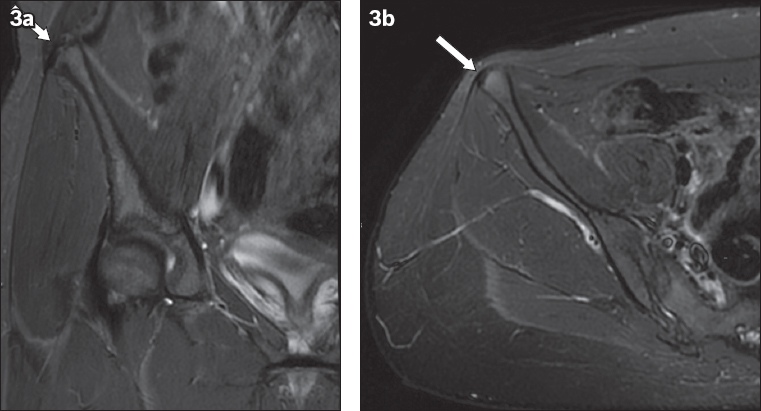
The timing at which the pelvic secondary centres of ossification appear and fuse is further illustrated in
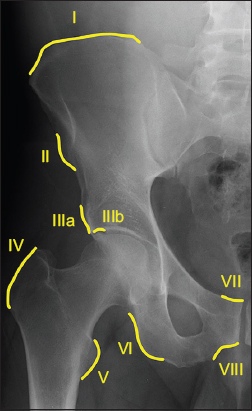
The anatomy of the muscle-tendon-bone complex differs between adults and children. In children or adolescents, the unossified apophysis remains weaker than the attaching musculotendinous unit, rendering it vulnerable to both acute avulsion fractures(5) and chronic stress injury or apophysitis.(6) The anatomical sites of pelvic apophyseal injury with their muscular or tendinous attachments are illustrated in the pelvic radiograph in
Fig. 4
Radiograph shows muscular origin/tendinous insertion sites: (I) iliac crest – abdominal muscles (internal and external obliques, and transverse abdominis), gluteus and tensor fascia latae; (II) anterior superior iliac spine – sartorius; (IIIa) anterior inferior iliac spine – long head of rectus femoris; (IIIb) superior lateral acetabulum – reflected head of rectus femoris; (IV) greater trochanter – gluteus medius, gluteus minimus, gemellus and piriformis; (V) lesser trochanter – iliopsoas; (VI) ischial tuberosity – common hamstring tendon origin; (VII) pubic crest – rectus abdominis muscle; and (VIII) inferior pubic ramus – adductor muscles.
Acute injuries with avulsion often occur owing to excessive unbalanced muscular contraction, resulting in excruciating pain with loss of function and weakness.(8,9) The mechanism for an acute iliac crest injury involves sudden contraction of the abdominal wall muscles during flexion and rotation of the torso.(9) It has been hypothesised that the abrupt violent contraction of the external oblique muscle probably leads to avulsion of the iliac crest apophyses, and the unopposed antagonistic traction of the gluteus medius and tensor fascia latae leads to the lateral and inferior displacement of the avulsed fragment.(10)
A retrospective review of 228 cases by Schuett et al showed that the most common site of pelvic avulsion fractures was the AIIS (49%), followed by the ASIS (30%), ischial tuberosity (11%) and iliac crest (10%).(7) Another series by Rossi and Dragoni, which included 203 cases, showed that the ischial tuberosity was the most common site of avulsion fracture (53.6%), followed by the AIIS (22.1%), ASIS (19.2%), superior corner of pubic symphysis (3.4%) and iliac crest (1.5%).(8)
Radiographs could identify up to 99% of all pelvic apophyseal avulsion fractures in Schuett et al’s series, with 1% requiring further evaluation with either computed tomography (CT) or MR imaging. As such, radiographs are often adequate for clinching a diagnosis, leaving more advanced imaging modalities for cases in which the radiographs are inconclusive and the diagnoses remain uncertain.(7)
Radiographs of an acute avulsion injury would confirm the presence of immature apophyses and may demonstrate a displaced fracture fragment adjacent to the site of muscular insertion.(11) Figs.
Fig. 5
Pelvic radiograph of an 11-year-old girl with recent sports injury at school shows an avulsion fracture of the right lesser trochanter with exuberant callus formation (arrow), which can be mistaken for an osseous tumour.
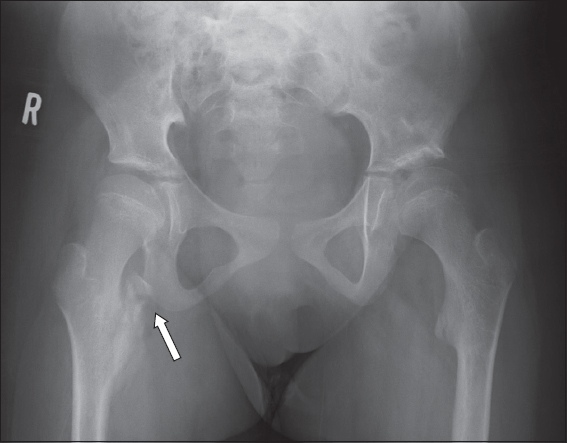
Fig. 6
Pelvic radiograph (performed with gonadal shielding) of a 14-year-old boy who was active in sports and presented with right hip pain shows an avulsion injury involving the right common hamstring muscle origin, with a displaced fracture fragment of the right ischial tuberosity (arrow).
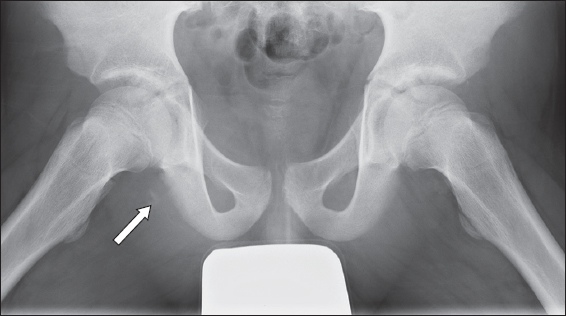
Fig. 7
Pelvic radiograph of a 16-year-old boy who presented with left hip pain following a football injury shows a left anterior inferior iliac spine avulsion fracture at the attachment site of the long head of the left rectus femoris (arrow).
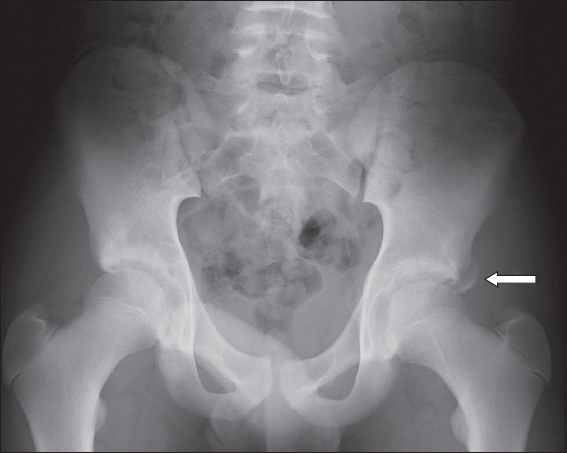
Fig. 8
Right hip radiograph of a 17-year-old boy with pain over the right iliac spine shows an avulsion fracture of the right anterior inferior iliac spine (arrow).

Fig. 9
Pelvic radiograph of a 25-year-old woman who presented with post-traumatic left hip pain shows left greater trochanter avulsion fracture at the gluteal tendon insertion site (arrow). This injury is very rarely encountered in the paediatric population. Although this is a radiograph of a skeletally mature patient, we would expect the radiographic image in a child to be similar in appearance.
However, the initial radiographs can appear falsely normal in the setting of an acute apophyseal injury when there is no significant displacement of the apophyses or when the abnormality is bilateral and symmetrical. Radiographs may not demonstrate the injury if the apophysis has yet to ossify, generally in the setting of the younger paediatric population (below 14 years of age).
MR imaging is, therefore, the preferred imaging modality in diagnosing apophyseal injury, as it depicts the extent of injury including the displacement of apophysis and is useful in assessing the chronicity of the injury. In addition, the associated soft tissue injury, such as the integrity of the surrounding musculotendinous structures, can easily be assessed on MR imaging.(12)
Chronic or healing apophyseal avulsion fractures may appear as an abundant periosteal formation adjacent to the apophyses on radiographs.(13) In some cases, the detached apophysis may lead to formation of irregular and exuberant callus, which may mimic a malignancy (
Apophysitis or chronic injury is more insidious in onset and varies in severity, generally with no inciting history of trauma and typically arising from repetitive microtrauma or overuse.(14,16) Iliac crest apophysitis is more prevalent in adolescents who participate in long-distance running.(7) The initial radiograph may show asymmetry of the iliac crest apophyses, with separation of the iliac crest from the iliac bone.(9) However, some iliac crest apophysitis may be unperceivable on radiograph or even CT, and MR imaging would be more sensitive in such cases. MR imaging features include physeal widening of 3–5 mm with increased signal intensity on water-sensitive sequences, bone marrow oedema within the iliac crest and oedema of the adjacent musculature. Displacement of the apophysis is generally absent in chronic injuries.(16)
Skeletal scintigraphy can be considered in certain cases.(13) Generally, scintigraphy reveals non-specific findings, including asymmetric increased radiotracer uptake on the blood pool and delayed images. Scintigraphy is mainly used with atypical clinical presentations and when other imaging modalities are inconclusive.(17) One potential disadvantage would be the risks of radiation to the patient.
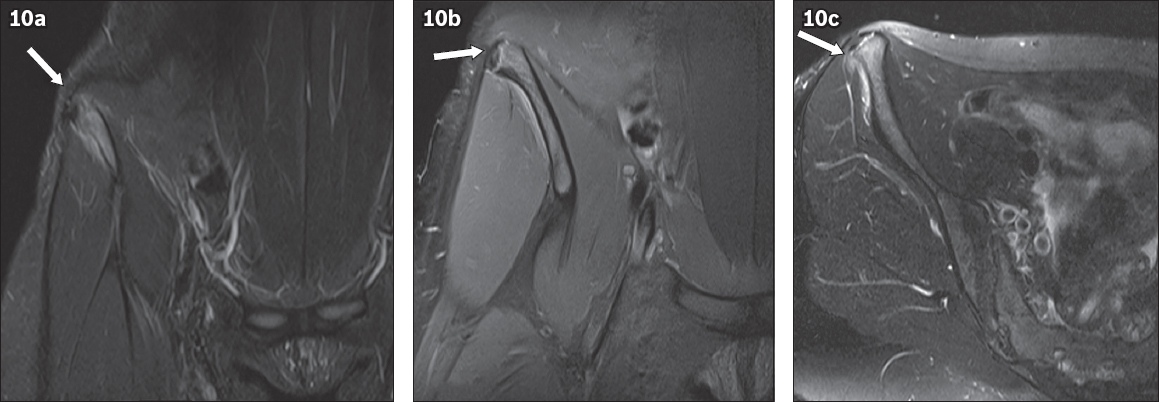
Coincidentally, our index patient had an elder sister, a 15-year-old athlete, who presented with a two-month history of right hip pain. She participated in running in school and frequently performed sprinting during training. She also underwent MR imaging of the pelvis (
Fig. 10
(a) Coronal T2-W turbo inversion recovery magnitude; (b) coronal FS proton density; and (c) axial T2-W FS pelvic MR images of our index patient’s 15-year-old elder sister, who presented with a two-month history of right hip pain following regular running, show high signal at the right iliac crest apophysis. There is mild widening of the iliac crest apophysis, with no significant displacement (arrows). Mild oedema is noted in the adjacent right gluteus and lateral abdominal muscles.
Apophyseal injuries in adolescents are rare(7) and are considered a challenge for the orthopaedic surgeon. In particular, iliac crest apophyseal injury accounts for only approximately 2% of pelvic fractures in adolescents.(8) Hence, an accurate diagnosis is essential, especially for demanding patients and professional athletes, so that the patients are able to return to sports in optimal condition as soon as possible. Potential consequences of missed pelvic avulsion fractures include impingement and irritation of the sciatic or lateral femoral cutaneous nerves, especially during prolonged sitting, and chronic muscle weakness due to shortening at the muscular origin, resulting in alterations in gait and inability to return to sports.(3)
Most cases of apophysitis and minimally displaced avulsion fractures involving the pelvic apophyses are treated with a period of altered weight bearing and slow return to activity, usually over a period of 6–12 weeks.(3) There is no well-established consensus for surgical management of these fractures in the literature. Generally, considerations for surgical management include the patient’s physical demands, greater fracture fragments and displacement.(12) A recent meta-analysis demonstrated that surgery has a better outcome than conservative management if the fracture fragment is larger than 15 mm.(19) Some authors favour surgical management if the fracture fragment is larger than 20 mm in its major axis and if the degree of dislocation exceeds 20 mm.(20) Other indications for surgery include chronic pain after conservative management or the presence of a large haematoma, which may compromise healing and require evacuation. Li et al showed that surgical management demonstrates good outcomes for patients, in that they are able to bear weight fully at two weeks and return to athletic activity at four weeks with no lower limb weakness.(21)
In summary, iliac crest apophysitis or avulsion is an uncommon injury.(7) First-line imaging is usually by radiography, and other modalities such as CT or MR imaging can be considered if the initial diagnosis remains inconclusive and there is a high index of suspicion. Prompt and accurate diagnosis is imperative for the best outcome among young patients. Iliac crest apophysitis and minimally displaced avulsion fractures are usually treated conservatively with rest and physiotherapy, leading to gradual return to sports. A subgroup of patients with more significantly displaced fracture fragments or those with higher functional demands, such as athletes, may benefit from surgical management.
Supplementary Material
SMJ-62-502.pdf