INTRODUCTION
The flexible reinforced laryngeal mask airway (f-LMA) is useful in various head and neck, ophthalmic, and oral surgeries, as its flexometallic tube resists compression and kinking and does not interfere with the surgical field. However, it is also more difficult to insert than the classic LMA.(1,2)
The ideal position of the f-LMA is especially important so as to allow movement of the stem or the patient’s head without dislodging the f-LMA intraoperatively. The most important feature of an LMA placed in an ideal position is the percentage of the epiglottis that is covered. In this regard, previous studies have reported that direct laryngoscope- or videolaryngoscope (VL)-assisted insertion is superior to the conventional blind insertion technique.(3-5) To date, no study has evaluated a VL-assisted technique for f-LMA insertion. We hypothesised that McGrath VL (McGrath MAC, Medtronic, Minneapolis, MN, USA)-assisted insertion provides better positioning of the f-LMA by lifting the epiglottis and securing the laryngeal view during f-LMA insertion. This study aimed to investigate the efficacy of the McGrath VL-assisted insertion of the f-LMA in comparison to that of the standard method of blind insertion technique with regard to oropharyngeal leak pressure (OLP) and the ideal anatomical positioning in anaesthetised adult patients.
METHODS
This single-centre, prospective, open-labelled, randomised control study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Institutional Review Board of Ajou University Hospital (AJIRB DEV-OBS-16-444) and was registered at ClinicalTrials.gov (NCT03510299). Written informed consent to participate was obtained from all patients. In total, 100 patients of American Society of Anesthesiologists physical status I or II who were scheduled to receive elective general anaesthesia with the use of LMA were included. Patients were randomly allocated to the control group (n = 50) or the McGrath group (n = 50) by an investigator blinded to this study, using a computer-generated randomisation table. The group and patient identification were assigned to the investigator who would perform the procedure only before f-LMA (Teleflex Medical, Westmeath, Ireland) insertion.
Upon arrival in the operating room, all patients were monitored and placed under routine general anaesthesia. The f-LMA was inserted according to the patient’s group by a single investigator (JY Yoo). In the control group, f-LMA was inserted using blind insertion technique involving classical digital manipulation. In the McGrath group, f-LMA was inserted using McGrath VL-assisted technique. Instead of using the hand, McGrath VL was inserted before f-LMA insertion to view the epiglottis. Then, the f-LMA was inserted along the blade of McGrath VL in the midline of the palate until the investigator confirmed that the f-LMA was positioned properly, using video guidance. In both groups, successful insertion of the f-LMA was confirmed by the absence of any air leakage with manual ventilation and by observing chest expansion with square wave form end-tidal CO2 curve during manual ventilation. Failure to successfully insert the f-LMA after three insertion attempts was defined as insertion failure.
Another investigator blinded to the f-LMA insertion technique evaluated the following parameters at neutral position with sniffing posture after confirming successful insertion: OLP, peak inspiratory pressure and fibreoptic laryngeal score (FLS). The primary outcome measure was OLP, which was evaluated as the airway pressure when the expiratory valve of the circle system was closed at a fixed gas flow of 3 L/min and the dial on the aneroid manometer reached equilibrium.(6) OLP and peak inspiratory pressure were evaluated after a two-minute adjustment. The FLS was evaluated using a fibreoptic bronchoscope following a four-point fibreoptic laryngeal scoring system.(7) Haemodynamic variables were recorded at three time points. The sample size was calculated based on a pilot study. All analyses were performed using IBM SPSS Statistics for Windows version 20.0 (IBM Corp, Armonk, NY, USA).
RESULTS
There were no significant differences in patient characteristics, type of surgery (urologic surgery and orthopaedic surgery), size difference of f-LMA and pre-anaesthetic airway assessment between the two groups.
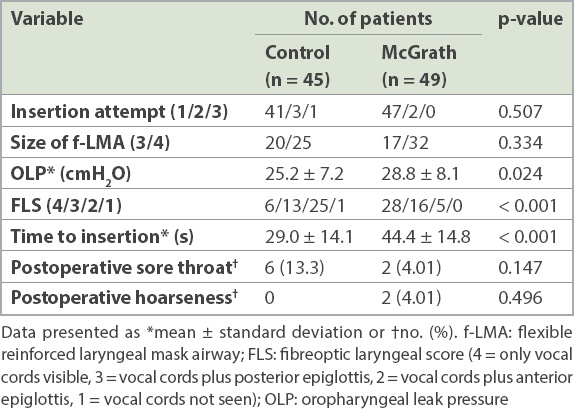
f-LMA failure occurred in 1 (2%) patient in the McGrath group and 5 (10%) patients in the control group (p = 0.204). The analysis between the two groups was conducted only in cases of successful intubation. The insertion characteristics of successful f-LMA insertion are listed in
Table I
Characteristics of successful f-LMA insertion.
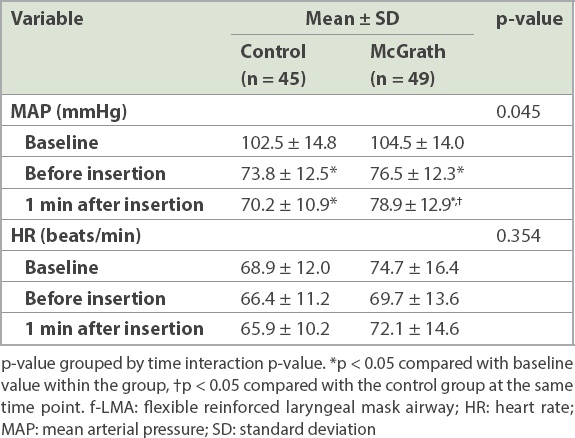
The haemodynamic variables are presented in
Table II
Haemodynamic changes during successful f-LMA insertion.
DISCUSSION
This study investigated the efficacy of McGrath VL-assisted insertion of the f-LMA in comparison to that of the standard method of blind insertion technique with regard to OLP and the ideal anatomical positioning in anaesthetised adult patients. The results demonstrated that the McGrath VL-assisted technique for f-LMA insertion was associated with higher OLP and a higher rate of ideal position than the blind insertion technique. However, it prolonged the time needed for successful f-LMA insertion and was also associated with more haemodynamic changes.
The ideal placement of f-LMA means proper sealing of the laryngeal inlet without aspiration and airway obstruction. In clinical practice, the OLP is an important index for proper sealing, because higher OLP is correlated with the tight fitting of LMA in the proper oropharyngeal inlet and could ensure better conditions during positive pressure ventilation.(3,8,9) Considering that the f-LMA could be used for surgery requiring multiple head and neck manipulations, a higher OLP may be important for adequate ventilation. In addition, some studies suggested that higher OLP might represent proper sealing in clinical, rather than anatomical, LMA position.(3,10,11) Several studies evaluated ventilation conditions and OLP in various positions of the head and neck and found that the OLP tended to be the lowest in the extended neck position.(6,8,9) Although the amount of decrease differed depending on the study and type of LMA, the higher OLP in neutral position could indicate better ventilation during head and neck movement, including extension. The reported OLPs of f-LMA, standard LMA, ProSeal LMA and Cobra perilaryngeal airway were 22 cmH2O, 21 cmH2O, 26.5 cmH2O and 28.7 cmH2O, respectively, in the neutral position.(9,12) In this study, the mean OLP was 25.2 cmH2O in the control group and 28.8 cmH2O in the McGrath group in the sniffing position. One of the reasons for these differences may be the differences in the head and neck positions in different studies, as well as the cuff positions.
Airway obstruction could be directly evaluated using the fibreoptic bronchoscope by determining the laryngeal inlet area covered by the epiglottis. The fibreoptic laryngeal score system defines FLS 4 as an ideal anatomical placement for the LMA; that is, the opening of the LMA clearly fitted the laryngeal inlet, thus ensuring good airflow without obstruction. In this study, the rate of ideal anatomical placement of the f-LMA was also significantly higher in the McGrath group than in the control group. Campbell et al(13) reported the usefulness of direct laryngoscopy for classic LMA insertion. The laryngoscope-assisted technique lifts the epiglottis during insertion to position the f-LMA more correctly, thus overcoming the limitation of the blind insertion technique. Campbell et al showed that the ideal positioning rate improved from 42% in the blind insertion group to 91.5% in the laryngoscopy-assisted group.(13) This result also applied to insertion of the f-LMA. Choo et al(14) prospectively compared two insertion techniques of the f-LMA in 108 patients and found that the rate of ideal position (FLS = 4) increased by 22% from 37% in the blind-insertion technique group to 59% in the direct laryngoscopy-assisted group. We hypothesised that McGrath VL would have similar or superior effects for the ideal positioning of the f-LMA because it could not only lift the epiglottis but also ensure that the f-LMA is positioned properly. In this study, the rate of ideal positioning (FLS = 4) increased by 44%, from 12% in the control group to 56% in the McGrath group.
However, we also found a drawback in the McGrath VL-assisted technique in that it prolonged the time to insertion of the f-LMA. This result is consistent with previous studies that compared blind insertion and the direct laryngoscope or VL for insertion of LMA.(3,15) This might be related to the additional time needed for laryngoscope manipulation and interruption of the insertion of the f-LMA into the oral space owing to the blade of McGrath VL occupying the oral space. However, it is interesting to note that once f-LMA entered the oral space, the blade of McGrath VL guided the passing of the f-LMA to the oropharyngeal area. The prolonged time of insertion might have minor clinical significance, because no patient experienced a hypoxic or desaturation event during anaesthesia induction.
The mean arterial pressure at one minute after insertion was higher in the McGrath group. A previous study reported that compared to the blind insertion technique, the direct laryngoscopy-assisted technique for f-LMA insertion did not increase the mean arterial pressure and heart rate.(14) This difference in the result of the current study might be because in direct laryngoscopy, the direct view of the epiglottis is sufficient to facilitate LMA insertion.(13) Meanwhile, we needed full laryngoscopy to confirm the correct position of the LMA when using McGrath VL. However, no patient needed antihypertensive treatment during anaesthesia induction, indicating that the higher mean arterial pressure might have little clinical significance.
In conclusion, the McGrath VL-assisted insertion technique could provide higher OLP and better anatomical placement of the f-LMA compared with the standard method, the blind insertion technique.


