Abstract
INTRODUCTION
This study aimed to determine and compare the effects of garlic tablets (Garcin®) and fluconazole on Candida vaginitis in women who presented to a health centre in Koohdasht, Iran, from August 2011 to March 2012.
METHODS
The clinical trial was conducted on 110 married women (aged 18–44 years) who had complaints of itching or a burning sensation in the vaginal area. Candida vaginitis was diagnosed by pH measurement of vaginal secretions, direct microscopic evaluation and Sabouraud dextrose agar cultures of the vaginal discharge. On confirmation of diagnosis, the patients were randomly divided into two groups (n = 55). One group received 1,500 mg of Garcin tablets daily and the other received fluconazole tablets 150 mg daily, over a period of seven days. Four to seven days after the completion of treatment, patients were examined for treatment response and possible side effects.
RESULTS
Complaints related to the disease improved by about 44% in the Garcin group and 63.5% in the fluconazole group (p < 0.05). The overall symptoms of the disease (i.e. redness of vulva and vagina, cheesy discharge, pustulopapular lesions and abnormal cervix) improved by about 60% in the Garcin group and 71.2% in the fluconazole group (p > 0.05). Results of microscopic evaluation and vaginal discharge culture showed significant differences before and after intervention in both groups (p < 0.05).
CONCLUSION
The present study shows that Garcin tablets could be a suitable alternative to fluconazole for the treatment of Candida vaginitis.
INTRODUCTION
Genital tract infection is a global health problem among women, particularly in East Asia.(1) While Candida albicans (C. albicans) is responsible for 90% of vaginal fungal infections (i.e. Candida vaginitis), non-albicans species are the main cause of recurrence and chronicity.(2) C. albicans is a fungus with two varieties, namely a yeast-like blastospore or mycelial hyphae, which exist symbiotically in the genital tract.(3)
Compared to C. glabrata, C. krusei and C. tropicalis, C. albicans has the strongest binding ability.(4) Aspartyl protease and phosphorylase enzymes are the two main agents required for tissue invasion in the pathogenesis of the disease. Investigations have revealed that the prevalence of Candida vaginitis varies according to geographical location. Its prevalence also depends on hygiene practices, cultural and social factors, as well as the diagnostic methods used. The reported disease prevalence is 12.2% in Brazil, 18.7% in Israel, 12.1% in Athens, 17.4% in Turkey, 20.4% in India and 6.5% in China.(5-10) Cunningham et al reported that C. albicans can be identified in the vaginal discharge cultures of 25% of pregnant women.(11)
The most prominent symptom of the disease is itching. The vaginal discharge of women with the condition varies from watery to a thick homogeneous consistency (typically cheese-like). These signs usually appear a week before the menstrual cycle begins.(4,12,13) As the signs and symptoms of the disease are nonspecific, it would be impossible to diagnose the disease based on clinical history and clinical manifestation alone. Microscopic evaluation and secretion culture are necessary for diagnosis.(12,14) Currently, there are no reliable serology tests available for the diagnosis of Candida vaginitis.
Topical azoles are most commonly used to treat Candida vaginitis.(13) However, the prophylactic and therapeutic use of antifungal drugs has caused increased drug resistance, resulting in treatment failure. Complementary therapies, which have fewer side effects, better tolerability and lower costs, have been shown to result in better patient compliance.(15) Common alternative treatments include vaginal vinegar shower, povidone iodine, boric acid, tea tree oil, lactobacilli recolonisation and garlic.(16)
Garlic contains 33 sulfur compounds, various enzymes and trace elements such as selenium. When garlic is cut or crushed, alliin is converted into allicin, following activation of the enzyme alliinase. Once metabolised, allicin produces various compounds such as diallyltrisulfide, diallyldisulfide, diallylsulfide, ajoene and vinyldithiines.(17) The antibiotic activity of 1 mg of allicin is reported to be equivalent to that of 15 units of penicillin.(18) Studies have postulated different mechanisms for the anti-Candida effects of garlic. These include: (a) inhibition of SIR2 gene expression in C. albicans;(3) (b) antioxidant activity of the sulfur components of garlic;(19) (c) increase of strong antioxidants such as glutathione;(20) (d) inhibition of Candida RNA synthesis;(20) (e) decrease in tumour necrosis factor alpha (TNF-α) and increase in interferon gamma (IFN-γ);(20) (f) peroxidation of plasma membrane phospholipid and disruption in the uniformity of fungal cell membrane;(21) and (g) inhibition of phosphatidyl choline synthesis in a lipid bilayered fungal membrane by ajoene and induced oxidative stress response in C. albicans by allyl alcohol (a metabolic product of garlic).(3)
Due to the increasing drug resistance of C. albicans to azole compounds, it is important to explore the use of alternative treatments for Candida vaginitis.(22) Garlic shows good potential as an alternative treatment, but it is crucial to ascertain effective and well-tolerated doses for the treatment of the disease. The present study was conducted to determine the effective dose of garlic tablets (Garcin®) for the treatment of Candida vaginitis, as well as to compare its effects with those of fluconazole.
METHODS
A randomised clinical trial involving two groups of patients was conducted before and after treatment. Between August 2011 and March 2012, married women aged 18–44 years who presented to Prophet Muhammed Health Centre in Koohdasht, Iran, with the primary complaint of vulval and/or vaginal itching and burning were eligible for participation in the study. Patients were included if they met the following criteria: not pregnant; not breastfeeding; not using hypoglycaemic drugs, immunosuppressive agents or salicylic acids; had not used antibiotics or vaginal medications for the past 14 days; had not participated in other studies in the past four weeks; did not have multiple sexual partners; no concurrent vaginal infections; no underlying medical illness and/or mental retardation; no sensitivity to garlic; and not having menses or likely to have menses until seven days after treatment completion. If the patients had to be administered antibiotics, displayed intolerance to any form of medication or became pregnant during the course of treatment, they were excluded from the study. The ethics committee of the Shahid Beheshti University of Medical Sciences and Health Services, Tehran, Iran, approved this study.
A questionnaire was used to obtain the patients’ demographic details, underlying medical conditions and treatment history. The questionnaire consisted of four sections: (a) demographic details; (b) pregnancy and menstrual history; (c) medication and disease history; and (d) health information, including a patient complaint and clinical observation checklist from the first and second sessions, and laboratory results. The list of complaints included itching, irritation of vulva and/or vagina, dysuria, dyspareunia and vaginal discharge. The list of symptoms included vaginal/vulval erythema, cottage cheese-like discharge, pustulopapular lesions and abnormal cervix.
Content validity of the questionnaire was assessed by gynaecologists and laboratory specialists, who respectively confirmed the researchers’ observations of the patients’ clinical signs and microscopic evaluations. Items used for the evaluation included: pH paper (Merck, Darmstadt, Germany), Motic 2820 microscope (Motic, Barcelona, Spain), single-door 55 lit aluminium incubator (Shimaz, Tehran, Iran), simple slide and 18 mm × 18 mm lamella, 16 mm × 160 mm glass tube and cotton swabs (NeginTeb, Lorestan, Iran). To ensure the reliability of the complaint and clinical observation checklist, ten patients were simultaneously evaluated by one of the researchers and another colleague. Microscopic evaluation of samples by the laboratory technician was validated through simultaneous evaluation by the researcher. The culture results of five coded samples (obtained from each patient) were validated by laboratory testing, while the pH test was repeated five times to ensure validity of the results. Kappa coefficient of agreement was calculated for all cases (minimum agreement coefficient was 0.8).
Prior to the start of the study, informed consent was obtained from the patients. The researcher completed the complaint and clinical observation checklist after reviewing the patients’ history and demographic data. To obtain samples and make clinical observations, the patients were positioned in the lithotomic position. Their vulva and groin were checked for redness, irritation and pustulopapular lesions. A sterile speculum was placed in the vagina without lubrication, and the vagina and cervix were observed for inflammation, redness and abnormalities. The form, colour, consistency and odour of vaginal discharge were observed, and the acidity was measured and recorded. Acidity was measured using a piece of pH paper placed on the lateral vaginal walls to avoid contact with the alkaline secretion of the cervix. As a pH level of 4.0–4.5 indicates a Candida infection, patients whose vaginal discharge was outside this pH range were excluded from the present study. A sample of lateral wall secretion from the upper vagina was collected and swiped onto two slides using sterile cotton swabs. A drop of 10% potassium hydroxide was added to the first slide and a drop of saline to the second slide. The samples were observed under a microscope at a magnification of × 40. The presence of mycelium and blastospores on the first slide indicated positivity for Candida infection. A patient was excluded from the study if her vaginal discharge was pH > 4.5 (which is likely caused by mixed infections) or if Gardnerella vaginitis was diagnosed (due to the presence of amine odour). The observation of flagellant parasites (i.e. trichomonas) or key cells (i.e. bacterial vaginosis) in the second slide would also exclude a patient from the study. Vaginal swabs were sent to the laboratory to obtain the final diagnosis and the 24- to 48-hour results were used.
Following the final diagnosis of Candida vaginitis (via Sabouruad dextrose agar cultures of the vaginal discharge), patients were randomly divided into two groups of 55 patients each (using random allocation software). For a period of seven days, one group received a single dose of fluconazole 150 mg (AveCinna Company, Tehran, Iran) daily, while the other group received 1,500 mg of Garcin® tablets (GolDaru, Isfahan, Iran) daily (500 mg three times a day). A leaflet containing information about the possible complications associated with the treatment, guidelines on sexual intercourse and the use of vaginal showers or antibiotics during the study period, and the researchers’ telephone numbers were provided to the patients. Four to seven days following the completion of treatment, both groups of patients were re-examined for treatment response. The complaint and clinical observation checklist as well as pH testing, microscopic evaluations and the Sabouruad dextrose agar culture of vaginal discharge were repeated, and the results recorded. Medication complications were noted for all samples. Treatment response was evaluated based on improvements in the patients’ complaints and symptoms (two main complaints/symptoms and overall complaints/symptoms), as well as microscopic evaluations and culture results.
Data was analysed using SPSS Statistics version 17.0 (SPSS Inc, Chicago, IL, USA). Descriptive statistics (mean and standard deviation) and inferential statistics (t-test, chi-square test, Mann-Whitney U test, McNemar test and Fisher’s exact test) were used. A p-value < 0.05 indicated statistical significance.
RESULTS
A total of 450 patients presented with the two main complaints associated with Candida vaginitis – itching and a burning sensation at the vulvar and vaginal areas. Among these 450 patients, 110 met the study inclusion criteria. During the course of the study, five patients from the Garcin group and three patients from the fluconazole group were further excluded. Thus, the samples from only 102 patients were used for statistical analysis.
The mean age of the 102 participants was 32.38 (range 19–44) years and their mean duration of marriage was 12.38 years. A majority of the women (96.1%) were housewives, with little or no education. The main form of contraception was either the birth control pill or intrauterine device. In terms of confounding factors (i.e. use of synthetic fibre underwear and/or tight/wet underwear) and underlying factors (i.e. number of pregnancies; live births; Caesarean sections and natural births; number of genitourinary infections in the past year; and frequency of sexual intercourse in the week prior to treatment), there was no significant difference between the Garcin group and the fluconazole group (
Table I
Presence of underlying factors for Candida vaginitis in the two groups.
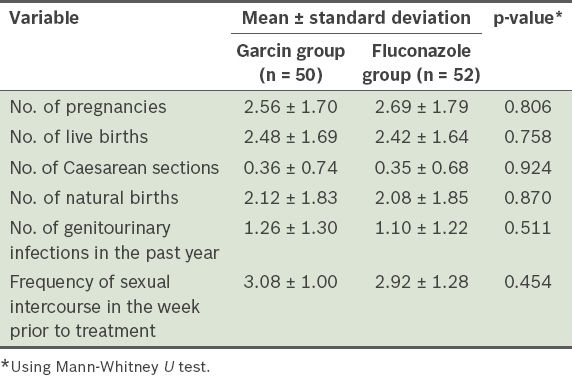
Table II
Frequency of complaints, observed symptoms and positive test results in the two groups before and after treatment.
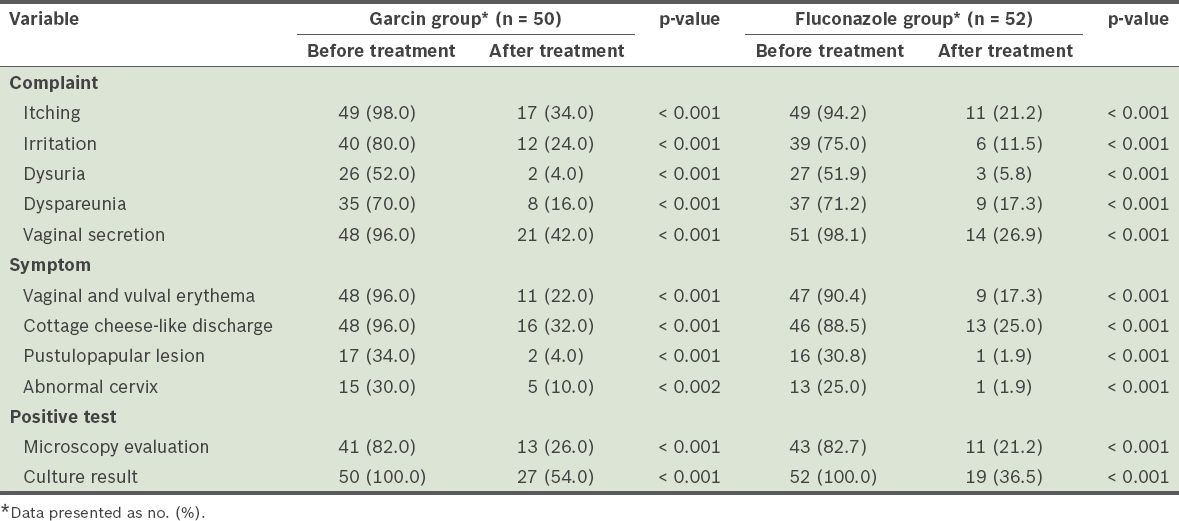
Most of the patients in the Garcin (82.0%) and fluconazole (82.7%) groups tested positive for fungal germination and mycelium on direct microscopic evaluation of the vaginal discharge. After treatment, the number of positive microscopy evaluations was significantly lower than that before treatment in both groups (McNemar test, p < 0.05), although no significant difference was found between the two groups before and after treatment (chi-square test, p > 0.05;
The two main complaints – itching and irritation (i.e. burning sensation at the vulva and/or vagina) – improved by 60.0% in the Garcin group and 73.1% in the fluconazole group. Chi-square test did not reveal any significant difference between the improvements observed in both groups, suggesting that both drugs had similar effects on these two main complaints. Overall, improvement in all complaints associated with the disease (i.e. itching, irritation of vulva and/or vagina, dysuria, dyspareunia and vaginal discharge) was 44.0% in the Garcin group and 63.5% in the fluconazole group. A significant difference in improvement of all complaints between the two groups (chi-square test, p < 0.05) was observed, with fluconazole being the more effective of the two drugs (
Table III
Frequency of complaints and symptoms (two main and overall) after treatment in the two groups.
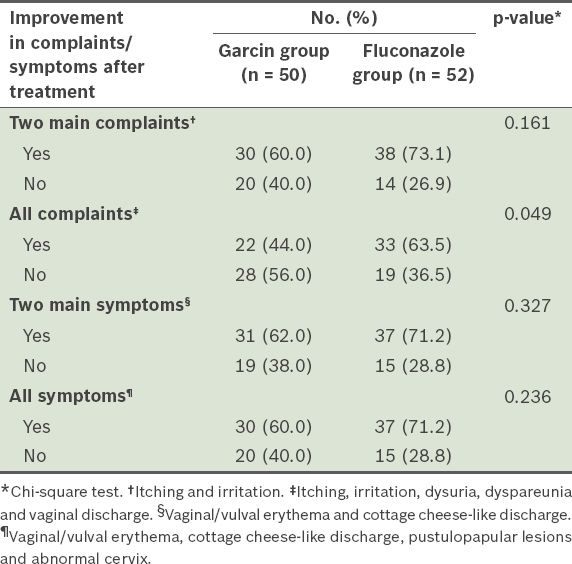
The two main symptoms – vaginal/vulval erythema and cottage cheese-like discharge – improved by 62.0% in the Garcin group and 71.2% in the fluconazole group. There was no significant difference between the two groups (chi-square test), thus suggesting that both drugs had a similar level of effectiveness in improving these two main symptoms. Overall, improvement in all symptoms (i.e. vaginal/vulval erythema, cottage cheese-like discharge, pustulopapular lesions and abnormal cervix) was 60.0% in the Garcin group and 71.2% in the fluconazole group. Chi-square test showed no significant difference between the two groups, suggesting that both drugs had a similar level of effectiveness in improving overall symptoms (
DISCUSSION
In the present study, a main complaint of Candida vaginitis was vaginal itching and a common symptom was vaginal discharge. Similarly, Grigoriou et al’s study(7) reported that itching (85.9%) was the most frequent complaint among patients with Candida vaginitis, with abnormal discharge found in 66.1% of patients. However, in Ahmad and Khan’s study of 215 women with Candida vaginitis,(9) 80% complained about itching but only 20% had vaginal discharge. This observed variation in frequency of complaints and symptoms may be due to differences in microbiology (e.g. species of fungus) and culture (particularly with regard to sexual behaviour) as a result of differences in the studies’ region of origin.
In the present study, the two most prevalent symptoms observed during clinical examination were redness of the vulva and vagina (i.e. vaginal and vulval erythema) and cottage cheese-like secretions. In the study by Ahmad and Khan,(9) redness and irritation of the vagina was the symptom with the highest frequency among women with positive discharge cultures. Likewise, Stovall et al(12) considered redness and irritation of the vulva and vagina, pustulopapular lesions and chunky white secretions to be symptoms of the disease.
In the present study, direct evaluation of wet slides was used to confirm the diagnosis of Candida vaginitis; 82.0% and 82.7% of women in the Garcin and fluconazole groups, respectively, tested positive (in terms of fungal germination or mycelial hyphae). In a study by Martinez et al,(23) diagnosis based on wet slides showed positive results in 96.6% of the probiotic fluconazole group and 88.5% of the placebo fluconazole group. In Ahmad and Khan’s study,(9) 167 (77.6%) of the 215 women with a positive vaginal culture had a positive direct microscopic evaluation of the secretions. Novak and Berek(13) stated that fungal elements (i.e. yeast-like blastospore or mycelial hyphae) are observed in 80% of cases following a microscopic evaluation of the secretions. This is in agreement with the results of the present study.
In vitro studies have confirmed the anti-Candida effects of garlic and its components. For instance, Khodavandi et al(22) confirmed the synergistic effects of allicin with azoles against the Candida spp. In a study by An et al,(21) analyses of the 50% and 90% minimal inhibitory concentration confirmed the synergistic effects of allicin with amphotericin B on 34 Candida spp. (i.e. 85% of all Candida spp.) and 40 Candida spp. (i.e. 100% of all Candida spp.), respectively. Low et al(3) confirmed the ability of garlic and its components to inhibit the production of hyphae; garlic extract was found to downregulate expression of the SIR2 gene in Candida, thus confirming the efficacy of garlic in suppressing hyphal formation from Candida cells. Islam et al(20) showed that garlic could be used to treat vaginitis (an inflammatory disease that causes increased TFN-α level and decreased IFN-γ and glutathione levels) due to the ability of allicin in improving the inflammatory and anti-oxidant response to vulvovaginal candidiasis, thus potentially mitigating the disease process. Corroborating the aforementioned in vitro studies, the results of the present study showed that Garcin and fluconazole are equally effective in reducing the number of complaints and symptoms associated with Candida vaginitis, and improving the results of microscopic evaluations and secretion culture.
To the best of our knowledge, no clinical study, prior to the present study, has been conducted to examine the efficacy of garlic (or garlic-containing drugs) in reducing both the complaints and symptoms associated with Candida vaginitis. Other studies(15,24) have examined its effects on symptoms of Candida vaginitis. For instance, Bahadoran et al’s study(15) found no significant difference in the frequency of clinical symptoms (i.e. vaginal discharge, vulval erythema and oedema) between two groups of patients (vaginal cream containing garlic and oregano vs. clotrimazole) before and after treatment. A study by Kordi et al(24) showed no significant difference between treatment with garlic extract vaginal shower (51% response) and clotrimazole vaginal cream (66.7% response). These studies supported the use of garlic products in the treatment of Candida vaginitis.
In the present study, findings of the microscopy evaluations showed that the number of positive results in the Garcin group reduced from 82.0% to 26.0% following treatment; a similar decrease (i.e. 82.7% to 21.2%) was observed in the fluconazole group following treatment. We also observed a reduction in the proportion of positive secretion culture in both the Garcin group (from 100.0% to 54.0%) and the fluconazole group (from 100.0% to 36.5%) following treatment. Therefore, both Garcin and fluconazole were equally effective treatments. In Kordi et al’s study,(24) the treatment response based on culture results was 40.8% in the group treated with garlic extract vaginal shower and 60.8% in the group treated with clotrimazole vaginal cream, with a significant difference between the groups.
In a study conducted by Sekhavat et al,(25) the authors found that the use of 150 mg single-dose fluconazole therapy improved mycology results by 83.3%. Sobel et al(26) reported similar results – 14 days after a single dose of 150 mg fluconazole, mycology results improved by 77%. In Martinez et al’s study,(23) the frequency of a positive Candida culture in the probiotic fluconazole group (150 mg, single dose) and the placebo fluconazole group (150 mg, single dose) after treatment was 10.3% and 38.5%, respectively. The secretion culture results after fluconazole treatment may vary because these studies were conducted in regions with different drug resistance profiles and/or varieties of C. albicans and non-albicans species. In a 2005 study by Richter et al,(27) 27 of the 429 women with Candida vaginitis had combination infections, mostly C. albicans and C. glabrata. As non-albicans species are resistant to antifungal drugs, treatment failure or recurrence may be attributed to the high survival rates of these drug-resistant species. In such cases, patient follow-up, identification of fungus species and drug sensitivity assessments are required.
In conclusion, the present study has shown that Garcin tablets are able to effectively reduce the number of complaints and improve the clinical symptoms associated with Candida vaginitis. Furthermore, Garcin tablets and fluconazole appear to show similar effects in both microscopy and culture evaluations in the present study. Given that there are fewer complications associated with the use of garlic and as there may be potentially greater acceptance among the target population for encapsulated garlic, as a health or herbal supplement rather than a drug, the use of garlic tablets may be able to replace current azoles in the treatment of Candida vaginitis. However, more evidence supporting the use of garlic is necessary to confirm this.
ACKNOWLEDGEMENTS
This article was the result of a Master’s degree dissertation in Midwifery from the Shahid Beheshti University of Medical Sciences, Tehran, Iran. We sincerely thank the Head and Deputy of Research, Department of Midwifery and Reproductive Health, Shahid Beheshti University of Medical Sciences, Tehran, Iran, as well as all participants in the study.


