Dear Sir,
We herein describe a novel way to prevent hydrothorax relapse in a peritoneal dialysis (PD) patient with the use of inclination, and therefore the force of gravity, to prevent peritoneal fluid from entering the thorax.
A 28-year-old woman who had been receiving automated peritoneal dialysis (APD) for two years contacted our institution’s PD clinic with complaints of cough and dyspnoea. Her past medical history was significant for mental retardation, congenital upper limb impairment, end-stage renal disease due to glomerulonephritis of unknown origin, hypertension and hyperuricaemia. Clinical examination revealed oedema of the lower extremities and reduced auscultation sounds in the right lower lung that were suggestive of pleural effusion. Residual diuresis (about 1,000 mL/day) was present. Chest radiography confirmed right pleural effusion (
Fig. 1
(a) Initial chest radiograph shows right pleural effusion in a 28-year-old female patient who was receiving automated peritoneal dialysis (APD). (b) First follow-up chest radiograph four days after APD interruption shows reduction of pleural effusion. (c) Second follow-up chest radiograph one month later shows complete resolution of pleural effusion during the time when the patient was performing APD in a sitting position.
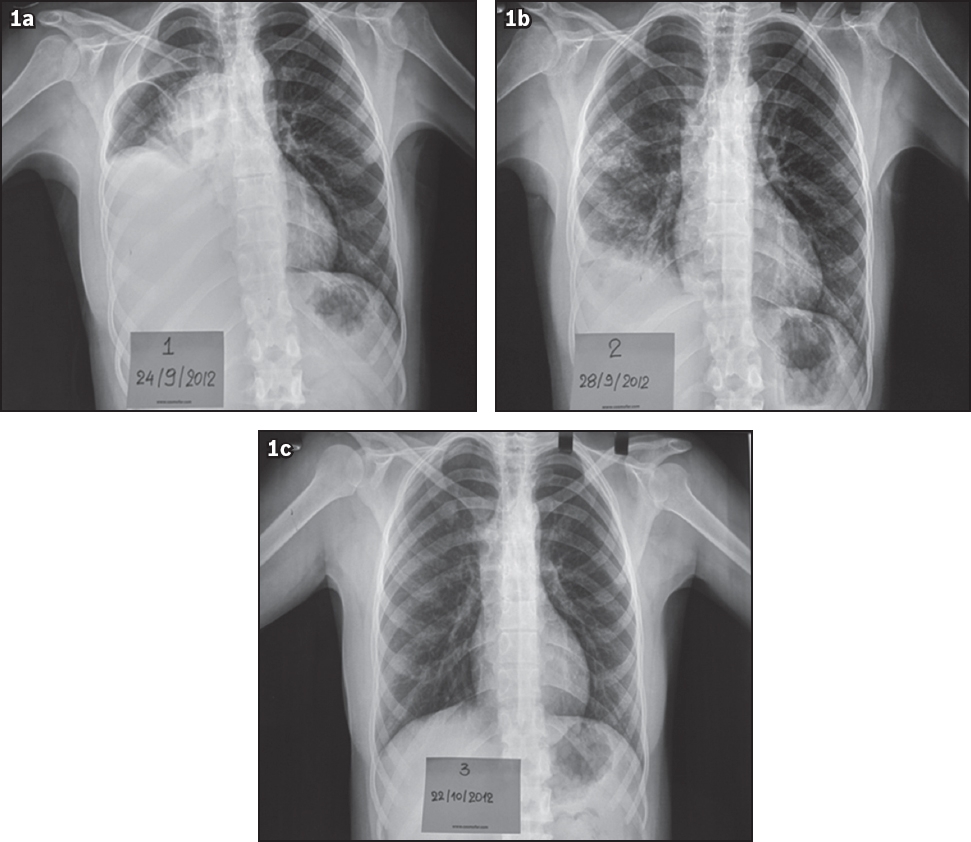
As no further diagnostic procedures were performed, the patient’s regular PD regimen, consisting of two exchanges overnight of 1.36% and 2.27% glucose dialysates in two 2.5 L bags, was discontinued and the patient was closely monitored. Four days after the PD regimen was discontinued, the peritoneal cavity remained free and reduction of pleural fluid was noted (
Unfortunately, we were unable to document whether the patient’s hydrothorax was the ‘sweet’ hydrothorax of PD, because the patient did not consent to further diagnostic or therapeutic interventions. Technetium-99m peritoneal scintigraphy would have been an appropriate modality to document this condition,(1) but it was not applied. In our case, the patient’s pleural effusion was attributed to fluid movement from the peritoneal cavity into the thorax due to transient increased intra-abdominal pressure. Performing PD in an initial sitting position and then in an inclined position was the best option for preventing dialysate reinsertion into the thorax, provided that adequate PD was maintained.
Open or laparoscopic surgery(2) is the common practice for repairing the diaphragmatic defect once pleuroperitoneal communication is confirmed. However, surgical techniques are known to lead to high PD dropout rates and consequent transfers to haemodialysis,(3) and our patient was not in favour of changing to another renal replacement therapy. In a series of children with hydrothorax, no surgical intervention was applied in the context of PD.(3) Similar to our case, PD was performed either in a seated position or while the patient was propped upright, but with initial low volume exchanges.
In conclusion, we have described a case of PD hydrothorax that was effectively managed by interrupting the initial PD and then resuming the same PD prescription with the patient in a seated and recumbent position. Acute hydrothorax should not be a sufficient reason to discontinue PD. We recommend that other, non-surgical interventions should be attempted first.
Yours sincerely,


