Abstract
INTRODUCTION
This study aimed to investigate the direct cost of outpatient care for patients with stroke, as well as the relationship between the aforementioned cost and the sociodemographic and stroke characteristics of the patients.
METHODS
This was a cross-sectional study involving patients with first-ever stroke who were attending outpatient stroke rehabilitation, and their family members. Participants were interviewed using a structured questionnaire designed to obtain information regarding the cost of outpatient care. Stroke severity was measured using the National Institute of Health Stroke Scale.
RESULTS
This study comprised 49 patients (28 men, 21 women) with a mean age of 60.2 (range 35–80) years. The mean total cost incurred was USD 547.10 (range USD 53.50–4,591.60), of which 36.6% was spent on attendant care, 25.5% on medical aids, 15.1% on travel expenses, 14.1% on medical fees and 8.5% on out-of-pocket expenses. Stroke severity, age > 70 years and haemorrhagic stroke were associated with increased cost. The mean cost of attending outpatient therapy per patient was USD 17.50 per session (range USD 6.60–30.60), with travelling expenses (41.8%) forming the bulk of the cost, followed by medical fees (38.1%) and out-of-pocket expenses (10.9%). Multiple regression analysis showed that stroke severity was the main determinant of post-stroke outpatient care cost (p < 0.001).
CONCLUSION
Post-stroke outpatient care costs are significantly influenced by stroke severity. The cost of attendant care was the main cost incurred during the first three months after hospital discharge, while travelling expenses was the main cost incurred when attending outpatient stroke rehabilitation therapy.
INTRODUCTION
About 15 million people worldwide suffer from a stroke annually, and of these, 5 million die, while another 5 million are left permanently disabled.(1) Globally, the stroke burden was 38 million disability-adjusted life years (DALYs) in 1990 and this number is projected to increase to 61 million DALYs in 2020.(1) As the prevalence of population ageing increases, so would the incidence of stroke, which would in turn increase expenditure on stroke-related healthcare.(2,3) In 2008, statistics compiled by the Health Informatics Centre Planning and Development Division of the Ministry of Health, Malaysia, showed that there were 24,056 new stroke cases and that the cerebrovascular disease (CVD) mortality rate was 15.01 per 100,000 people.(4) CVD is the fifth most common cause of mortality after ischaemic heart disease; CVD accounts for 7% of the total disease burden in persons aged 30–59 years and 12% of the total disease burden in persons aged ≥ 60 years.(5)
The economic burden of stroke has an impact on national healthcare expenditures.(6-9) A tertiary hospital in Malaysia reported that the mean direct medical cost of inpatient stroke care incurred by health providers was USD 1,192 per patient per admission (i.e. 16% of Malaysia’s gross domestic product [GDP] per capita in 2010).(10) Human resources formed the highest cost component (36.4%), followed by medication (23.5%) and laboratory services (9.2%).(10) Although studies on the cost of outpatient stroke rehabilitation have been published, most were conducted in developed countries and described the costs incurred by the health provider (e.g. staff costs and variable overhead costs).(11,12) Little attention has been paid to the costs borne by stroke patients and their families.(13,14) As most developing countries have a limited healthcare budget, research on the cost of healthcare service is imperative to ensure the cost-effectiveness of current healthcare policies.
University Malaya Medical Centre (UMMC) is a teaching hospital located in Kuala Lumpur, the capital of Malaysia. With a capacity of 895 beds, it is one of the largest public hospitals in Malaysia that provides specialised care. As the stroke rehabilitation service in UMMC is mainly an outpatient programme, the need for frequent hospital visits may result in significant financial burden on stroke patients. This is especially true as most patients with stroke are not independent and require a companion for the hospital visit. Furthermore, the need for a companion during hospital visits could mean a further loss in the productivity of the companion. As the method of healthcare delivery varies in different countries, it is not possible to estimate the costs of stroke for one country based on the findings made in other countries.(15) Thus, the primary objective of the present study was to investigate the costs of outpatient stroke care incurred by the patients and their families in the first three months after hospital discharge. The secondary objective was to determine the relationship between these costs and the patients’ sociodemographic and stroke characteristics.
METHODS
This cross-sectional study was conducted in UMMC. The UMMC Medical Ethics Committee approved the present study (reference no. 739.7). Written informed consent was obtained from all patients who participated in the present study, and the voluntary nature of the study was explained to both patients and their caregivers before the interviews were conducted. All patients admitted to the neurology ward of UMMC between August 2010 and April 2011 were screened for eligibility for inclusion in the present study by the primary investigator. Patients who were hospitalised within 72 hours of the onset of a first-ever stroke (ischaemic or haemorrhagic), as defined by the World Health Organization (WHO),(16) underwent outpatient rehabilitation in UMMC, and had a caregiver were eligible for inclusion in the present study. Patients were excluded from the study if they were pre-morbidly dependent and/or had subarachnoid haemorrhage, transient ischaemic attack, epilepsy, psychiatric illness or any terminal illness that could affect their daily function and activities. In the present study, we limited the study period to the first three months after hospital discharge because studies have shown that most of the recovery takes place during this period.(17)
We developed a questionnaire that consisted of three sections: (a) the patient’s sociodemographic data (i.e. age, gender, ethnicity, marital status, employment status, education level and income level), and the caregiver’s job, education level and income level; (b) stroke characteristics, including type of stroke (i.e. ischaemic or haemorrhagic), severity of stroke (measured using the National Institute of Health Stroke Scale [NIHSS]), length of hospital stay and stroke risk factors; and (c) stroke-related costs incurred by the patients. The family members of the patients were interviewed three times within the first three months following stroke, and the costs were averaged for analysis.
In the present study, costs were defined as those incurred by the patients and their families as a direct result of the stroke. The costs reported by the family members were collected and analysed. However, we did not verify the costs reported (e.g. by asking for medical bills or receipts). We considered only the direct cost of therapeutic goods and services, and the other resources that are usually, but not exclusively, provided after discharge from acute care, including attendant care. The costs were grouped into the following categories: (a) medical consultation and therapy fees; (b) attendant care; (c) travelling expenses (for hospital visits); (d) out-of-pocket expenses; and (e) cost of medical equipment. We also documented the cost of additional therapy from other resources, including alternative therapy (e.g. acupuncture, massage, herbal or traditional medicine). At the time of the study (i.e. in the year 2011), USD 1.0 equalled approximately MYR 3.1.
The total incurred cost and the cost spent for each hospital visit were calculated. The cost of each hospital visit was subsequently extrapolated to find the estimated cost of outpatient stroke therapy in the first three months. Pearson, Spearman and Kendall’s tau-b correlation tests were used to explore the correlation among variables. Mean costs were analysed and compared using independent sample t-tests. Mann-Whitney U-test, t-test or chi-square test were used, when appropriate, to compare variables between two groups. Prespecified variables were then entered into multiple regression analysis models to determine the relationship between the variable and the costs. A p-value < 0.05 was considered statistically significant.
RESULTS
Among patients with acute first-ever stroke who were admitted to the neurology ward of UMMC between August 2010 and April 2011, 52 met the inclusion criteria, and all agreed to participate in the present study. Of these 52 patients, 3 died and 49 (28 men, 21 women) completed the study.
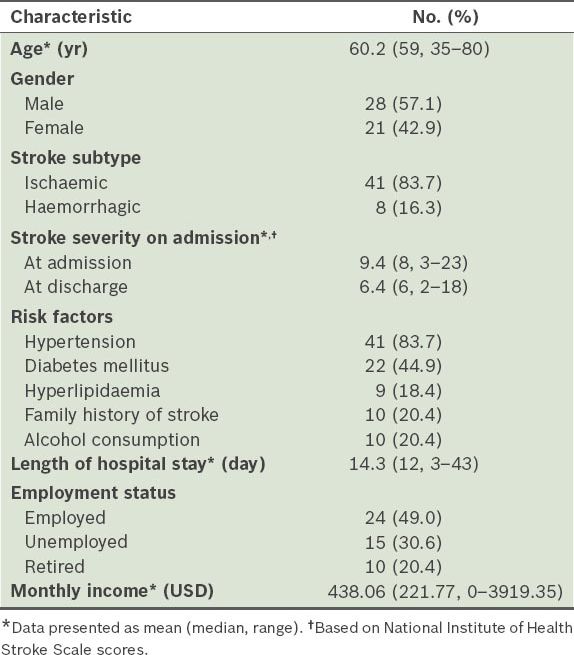
The sociodemographics and illness characteristics of the patients are shown in
Table I
Sociodemographics and stroke characteristics of patients (n = 49).
The distribution of the direct costs incurred by patients is shown in
Table II
Direct cost (in USD) of outpatient stroke care during the first three months after hospital discharge.
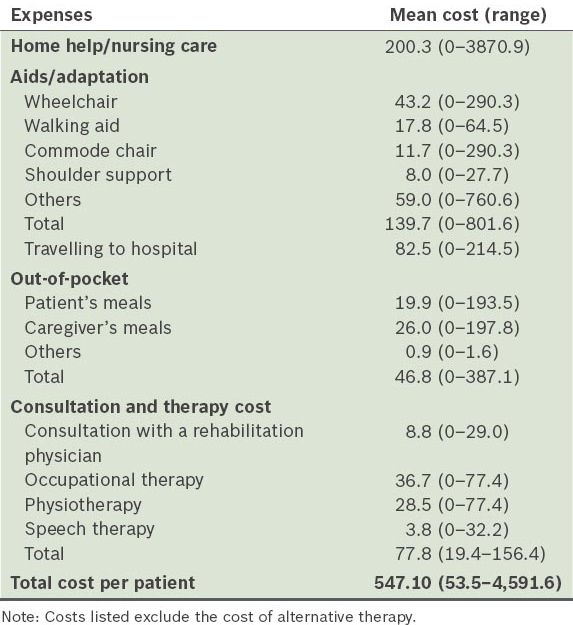
We found that patients aged < 70 years spent more on medical consultations and therapy sessions than those aged ≥ 70 years (USD 84.30 ± 36.70 vs. USD 50.30 ± 38.90). The cost incurred by patients with haemorrhagic stroke was significantly higher than the cost incurred by patients with ischaemic stroke (USD 1,032.50 vs. USD 451.90, p = 0.035). There was a positive relationship between stroke severity (measured using NIHSS) and cost. The mean total cost for patients with severe stroke was approximately 5 and 2.5 times that of patients with mild and moderate strokes, respectively. Multiple regression analysis established stroke severity as the main determinant of total cost (β = 0.362, p = 0.01), and stroke severity was found to be responsible for 27% of the total cost variance.
DISCUSSION
The present study gathered information on stroke-related costs incurred by patients from a developing country, adding valuable knowledge to current information on the known costs of stroke. To the best of our knowledge, the present study is the first to describe the direct costs incurred by stroke survivors and their families upon discharge from a hospital in Malaysia. Although several studies have established the effect of stroke severity on the cost of inpatient care,(19,20) the present study highlighted that stroke severity also influences the cost of outpatient care following a stroke. We found that patients who experienced more severe strokes required more medical aids and nursing help, attended outpatient therapy more frequently and were more likely to seek alternative therapies.
In the present study, patients spent approximately 60% of their total cost on attendant care and medical equipment purchases, while only 14% of the total cost was for expenses due to medical consultation and therapy services. This is a reflection of the healthcare financing system in Malaysia, where medical service fees are heavily subsidised in public hospitals as part of the government’s objective to provide affordable medical services and enhanced access to healthcare.(21,22) However, as the majority of the healthcare budget is directed toward curative medical care, patients and their families have to bear most of the costs related to disability and long-term care.(22) There is no mandatory national health insurance scheme in Malaysia and private medical insurance is purchased voluntarily. The coverage provided by private medical insurance companies varies greatly and there is no universal policy on the purchase of rehabilitation equipment, long-term care and home modifications. These aforementioned factors explain why we found that costs increased with increasing stroke severity.
In the present study, travelling to the hospital for therapy and consultation sessions formed the bulk of the costs that the patients and their family members had to bear. In fact, 23.6% of the incurred costs was related to travelling expenses (includes transportation, mileage, toll charges) and meals in the hospital. As transportation and meals constitute a substantial portion of the cost of each outpatient visit, they are likely to affect a patient’s ability to attend therapy regularly. This might also explain why most patients prefer to have therapy and consultation sessions on the same day. By scheduling therapy and consultation sessions on the same day, patients and their caregivers not only save money on transportation and meals in the hospital, but also reduce the number of days that the caregiver has to miss work. This helps reduce the negative effect of hospital sessions on the caregiver’s productivity. The findings of the present study suggest that attending regular therapy sessions can result in significant financial burden on patients and their family members. As such, home-based therapies may be an attractive alternative. In an earlier study, we found that home-based therapy using a video was as beneficial as conventional outpatient therapy and that it was not associated with increased stroke-related complications.(23)
In the present study, we also found that patients and their family members spent nearly 40% of their total income to finance outpatient stroke rehabilitation treatment. This percentage differs greatly from the usual Malaysian household expenditure on medical goods and services (i.e. 2.6%–3.5% of total income per month).(24) In other words, stroke-related costs impose an obvious economic burden on those affected. As Malaysia’s expenditure on healthcare (at less than 5%–6% of the annual GDP) is currently below that recommended by WHO,(5) allocating additional funds for healthcare, subsidising the costs of rehabilitation equipment and provision of long-term care could help reduce the financial burden on stroke patients and their family members.(25,26)
The present study was not without limitations. One limitation was the short time period used for the cost estimation of post-stroke care. Although post-stroke recovery plateaus after three months, previous studies have evaluated the costs for up to 12 months following the stroke incident.(27-29) Secondly, the costs calculated in the present study were based on the self-reports of the family members of the stroke patients. These reports could have been inaccurate. Future research should consider verifying the amount reported by comparing against medical bills and receipts. Thirdly, as the present study was a single hospital-based analysis with a small sample size, the findings may not be representative of the data and costs of all stroke patients throughout Malaysia. Furthermore, the healthcare delivery and charges of UMMC differs from that of a government hospital. Nevertheless, the analyses conducted in the present study generated data that could be useful for the future planning of health services that aim to meet the needs of patients and families affected by stroke. Future research should examine the stroke-related costs incurred by the government, as well as the indirect costs of stroke. The addition of a quality-of-life component to cost-related research should also be considered.
In conclusion, the costs of outpatient stroke care were found to be significantly influenced by the severity of the stroke. The cost of attendant care was the main cost incurred by patients during the first three months after hospital discharge, while the cost of travelling to the hospital was the main cost incurred when attending outpatient stroke rehabilitation therapy.


