Abstract
INTRODUCTION
Reflective learning is the cognitive process whereby information from new experiences is integrated into existing knowledge structures and mental models. In our complex healthcare system, reflective learning (specifically ‘reflection on action’) is important for postgraduate learners. We observed that our anaesthesiology residents were not building on their competence through deliberate experiential and reflective practice. This qualitative study explored the current state and challenges of reflective learning in anaesthesia training in Singapore.
METHODS
This study was conducted at KK Women’s and Children’s Hospital, Singapore, from 1 January 2018 to 31 October 2018. A semi-structured interview format was used in focus groups. Information collection continued until data saturation was reached. The interviews were coded and analysed, and themes were identified. Seven focus group interviews involving 19 participants were conducted.
RESULTS
Reflective learning was found to be poor. It was of concern that the stimuli for reflection and reflective learning emerged from medical errors, critical incidents and poor patient outcomes. Challenges identified were: (a) lack of an experiential learning framework; (b) need for reflective training; (c) quality of experiential triggers; (d) clinical pressures; and (e) poor learner articulation and feedback. We described some strategies to frame, teach and stimulate reflective learning.
CONCLUSION
This study described the state and challenges of reflective learning in anaesthesia training. We advocate the implementation of reflective training strategies in postgraduate training programmes in Singapore. Research is warranted to integrate patient feedback and outcomes into reflective practice.
INTRODUCTION
Reflection is a cognitive process whereby an individual looks back and creates new awareness of self and situation from a new experience. This purposeful act creates opportunities for further learning (reflective learning) and practice (reflective practice).(1,2) Reflective learning occurs when this new information is integrated into existing knowledge structures and mental models, resulting in the transfer from superficial to deep learning.(3,4) There is increasing evidence that reflective learning can improve academic performance and clinical practice in medical students and healthcare professionals.(5) Reflective practice strategies have also improved clinical reasoning, diagnostic accuracy, and non-clinical attributes such as ethics, professionalism, communication and empathy.(6,7)
We conducted this qualitative study to explore the current state of reflective learning and practice in our postgraduate anaesthesia training programme. As part of anaesthetic teams, our residents observe and learn to manage real world challenges in their training towards professional competence. In the complex healthcare system, they may encounter stressful situations that challenge not only their clinical competencies but also their beliefs, attitudes and values.(8) Hence, it is necessary that we equip learners with the reflective capacity to manage these demands.
Sandars aptly described the stage and nature of reflective learning for these learners and novice practitioners as ‘reflection on action’.(2) This form of reflection typically occurs after a clinical experience. In order to transform the clinical experience into knowledge, our residents would need to review actively what had happened, what was done and what could be improved in the next instance to improve the outcome. This is the nature of the relationship as described by Kolb, that knowledge and practice are interdependent.(9)
The Accreditation Council for Graduate Medical Education-International stipulates a mandatory number of case logs in each of the anaesthetic subspecialties over three years of junior residency. Procedural expertise is facilitated through deliberate practice and protected clinical opportunities.(10) Despite deliberate experiential training, we observed that our residents were not improving their competence as they fulfilled the case numbers. The faculty observed that residents seldom reviewed their own performances and, as a result, struggled to build new knowledge from clinical experiences. The ability to formulate advanced anaesthetic management plans was poor. There were also concerns from the faculty that the residents were emulating the former’s clinical ‘actions’ but not inquiring or reflecting on the rationale of the management.
The purpose of our study was twofold. Firstly, we wanted to establish the state of reflective learning and practice in our anaesthesiology residents. Secondly, we wanted to identify the likely challenges in reflective learning. Unfortunately, local experience on reflective learning and practice is lacking. To date, there has only one published study that investigated the use of reflection in public health communications in medical students.(11) Hence, the state of reflective learning and practice in our postgraduate programmes in Singapore remained largely unknown.
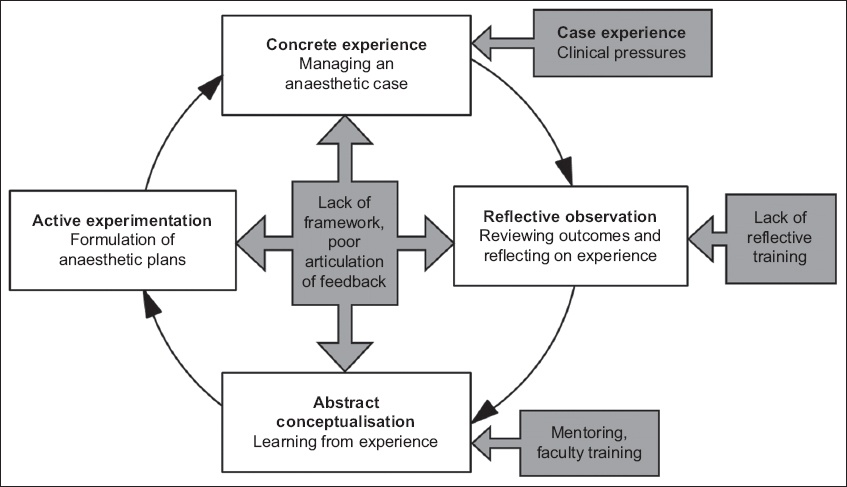
Our research purpose was underpinned by the experiential learning theory as described by Kolb (
Fig. 1
Flowchart shows Kolb’s experiential learning cycle, adapted for anaesthesia experiential learning. Black boxes indicate the influence of the challenges on experiential learning.
Our research questions were as follows: (a) What is the current state of reflective learning in junior anaesthesiology residents? and (b) what challenges did they encounter in reflective learning and practice?
METHODS
This study was conducted from 1 January 2018 to 31 October 2018. We adopted a constructivist approach to fill the knowledge gaps and build our knowledge on the state of reflective learning.(12) Through this approach, by focusing on the values, beliefs and ideologies of the residents, we hoped to explore their perceptions of their own reflective practices and how these could have been influenced by factors in the clinical learning environment.
The study was undertaken at the SingHealth Anaesthesia Residency Programme in Singapore. Institutional ethics approval was obtained from the SingHealth Centralised Institutional Board. A homogenous cohort of junior residents in their second and third year of training was included in the study.(13) This was to fulfil the purpose of exploring common experiences encountered by the junior residents. The inclusion criteria included junior residents in their second and third year of training who were doing the obstetric anaesthesia rotation in the Department of Women’s Anaesthesia, KK Women’s and Children’s Hospital, Singapore. The participants were informed about the study during the orientation briefing and invited to participate through email.
A focus group methodology was chosen to interview participants to gain in-depth insight into their experiences.(14) Two of the investigators (Goy and Ithnin) conducted the interviews. Participants’ responses and their interactions during the discussions were recorded. We observed and noted their agreements and disagreements in both verbal conversations and body language. Semi-structured interviews were used as the method of data collection.(15) The initial questions and probes were formulated based on the research questions. There were five questions, with 3–5 probes for each question. All interview sessions were audiotaped and transcribed verbatim by an independent professional transcriber.
The transcripts were then separately coded by three investigators (Lee, Goy and Ithnin). We independently categorised the codes into code tables and compared our findings in person. Emergent themes were identified and discussed through the analysis of the codes. We practised iteration in the data collection by performing the coding and analysis of the codes after the third focus group, in order to adjust the questions and probes to draw out more meaningful information from the participants. We also performed member checking by discussing these results with the participants to ensure the accuracy of our interpretation. These results were subsequently discussed at the education and faculty meeting for reflexive sharing and to ensure the rigour of the results.
Various strategies were employed to safeguard research quality in this study,(16) including the strategies of iterative data collection, analysis and thematic classification. Iterative data collection involves cycling between the processes of data collection and data analysis, which facilitates exploration of themes that were not explored in depth previously.(13) Data triangulation was performed, which involves corroborating the themes identified from the interviews with the feedback obtained from the residents’ end-of-posting feedback in order to ensure credibility and accuracy of the information. In our department, residents provide feedback on learning, difficulties encountered and their experience during the rotation during a face-to-face end-of-posting feedback session with the site’s Associate Programme Director. To facilitate transferability to the other postgraduate programmes in Singapore, we detailed the context and the experiences of the residents. In the discussions, we compared our findings with those of existing studies from different educational settings. In order to maintain the objectivity of our study, we presented the findings to faculty members at educational meetings. To overcome personal and epistemological reflexivity issues, we discussed our findings with our academic education committee, as well as faculty members in other training departments.
RESULTS
A total of 19 junior residents, aged 26–29 years, participated in the study. The seven focus group interviews lasted between 30 and 45 minutes.
We found that the current state of reflective practice after experiential learning was poor. The participants perceived that close to three quarters of the deliberate clinical experience did not result in reflection and learning. As one participant said, “Whether or not we do it [reflection] on a daily basis, it’s really very variable and dependent on the case. I think whenever something goes wrong, you will reflect unconsciously.”
The predominant stimuli for reflection and learning were experiences arising from medical errors, critical incidents and poor patient outcomes. In the absence of faculty guidance, residents concurred that ‘routine’ cases did not provide stimuli for reflective learning:
- “Adverse outcomes will stimulate me to reflect, because I feel at least things could have been prevented if I had changed my practice.”
- “When I’m writing the AIMS [anaesthesia critical incident] report, because it’s directly related to what you did and you realised what mistake you’ve made or what could have been prevented, it doesn’t feel great, because you reflect on what you missed out.”
Five main challenges were found, namely: (a) lack of an experiential learning framework; (b) need for reflective training; (c) quality of experiential triggers; (d) clinical pressures; and (e) poor articulation of learners’ needs and feedback. These challenges and their associated factors are presented in
Table I
Challenges in reflective learning and associated factors.
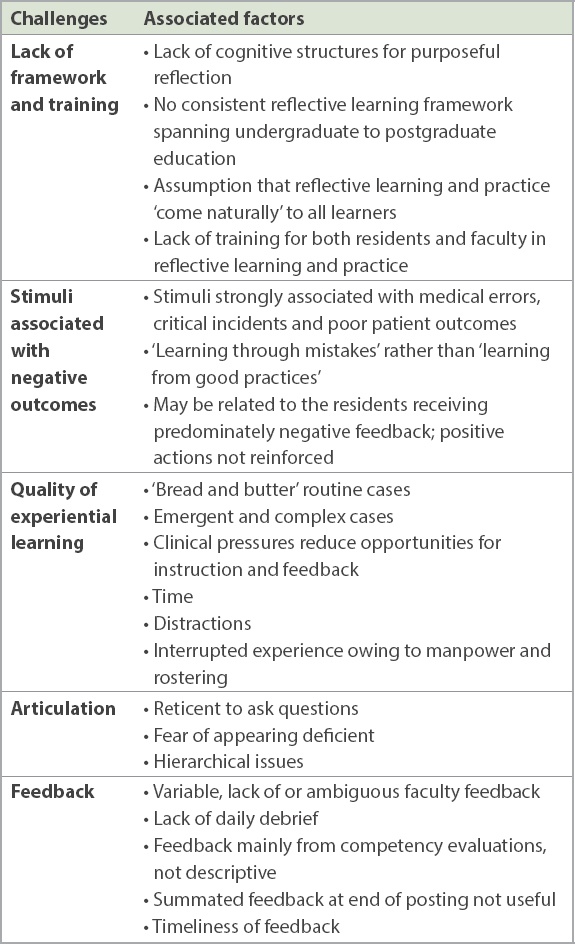
The participants had no knowledge of an experiential learning framework and also lacked training in reflective practice in undergraduate residency education: “Reflection for me is self-driven, but there is no framework for me to reflect and learn from every case.” As a result, they were unable to frame and integrate the information from new experiences: “I have not had any training on how of reflect, and in my mind, there is no particular framework. I do not know how to classify the points that occurred to me.”
The participants were of the opinion that the quality of the learning experience was important in reflective learning. Positive factors included faculty guidance and facilitation of the learning points, interesting clinical cases and unusual case presentations. Routine ‘bread and butter’ cases, which were associated with high volumes and fast turnover, did not trigger reflection: “Sometimes it’s just so routine, unless the faculty can ask certain questions that you probably didn’t think about.” They reported that thinking and reflecting on experience required protected time, space and opportunities. Multiple pressures that arose from the clinical learning environment were disruptive. These included fast patient turnovers, time pressures, and physical and psychological fatigue. Other competing commitment and distractions, such as administrative duties and examinations, also hindered reflective practice.
Participants were reticent in asking questions and clarifying their doubts with the faculty. It was concerning that they would rather leave questions unanswered than seek clarification from the faculty because of fears of appearing deficient. A participant said, “Any asking is possibly (casting) a doubt on your own abilities.”
They reported that poor feedback from the faculty did not facilitate reflection and learning. Examples of poor feedback included negative feedback, lack of timely feedback and feedback that was lacking in qualitative descriptors:
- “It is in our culture that people tend to only tell you negative points when you have done wrong, hence we tend to learn from negative experiences.”
- “Immediate feedback is more valuable for me to reflect. And I have expressed this a number of times to my seniors. I think the faculty are quite amenable to give direct feedback.”
- “The ‘New Innovations feedback’, there are two components – the numerical scale and the narrative. Most of the time, it’s just the ratings on the numerical scale. I feel that the specific narratives will probably help me to improve and learn more.”
The participants agreed that a debrief at the end of the clinical day would facilitate reflection and the formulation of thought processes. One participant said, “A short debrief can actually help me understand the case better and if, let’s say, in future I meet with something similar, then there will be the thought process there.”
DISCUSSION
This study showed that reflective learning and practice were poor in our training programme. Residents were unlikely to progress to the phases of abstract conceptualisation and experimentation in the absence of structured reflection.(9) These findings concurred with our observations that despite deliberate practice, new clinical experiences could not transition to new knowledge mental models. The absence of critical reflection also likely led to difficulties in self-examination, setting of goals and independence.(5) These findings are of concern, as anaesthetic practice involves dealing with highly stressful, demanding situations that require such skills. It is essential that our residents develop the ‘reflection on action’ reflective capacity before graduating and working as specialists.(17,18) Indeed, weak ‘reflection-on-action’ reflective capacity could potentially have a negative impact on the development of non-technical anaesthetic skills, including situation awareness, decision-making, teamwork, leadership, and management of stress and fatigue.(19)
In the absence of a mental model to frame the information on good practices received from new experiences, medical errors, critical incidents and poor outcomes were predominant stimuli for reflection. This could have been further exacerbated by the mandatory anaesthesia critical incident reporting process, which makes it mandatory for residents to submit a report on the root causes of the incident. While reporting could arguably be a reflective exercise, the obligatory reflection was performed in response to the error, and not their learning, and might not result in completion of the learning cycle.(18) Hence, there is a need to change the mindset of learners and clinical teachers. We need to shift the culture from learning from errors to learning from positive practices and outcomes.(20) This cultural change has to be nurtured in a safe and non-judgemental learning environment.(21) The short end-of-day debrief, as proposed by the residents, could be an excellent strategy to instil this cultural change.(22)
Our challenges were multifactorial in nature, which was consistent with other international studies.(5) The grey boxes in
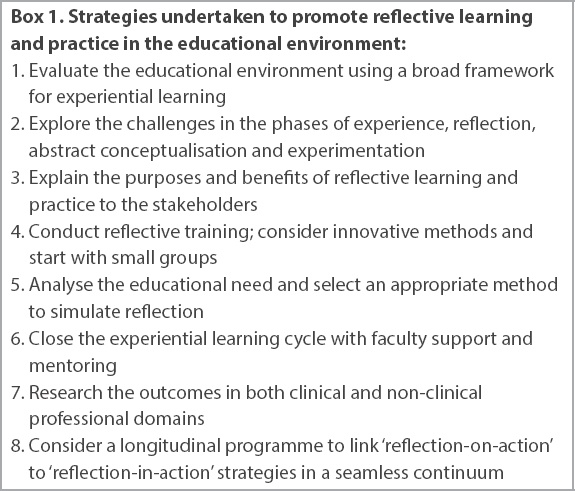
There are multiple models of reflective learning.(23) Most are simple to interpret and understand, and hence, theoretically, should be easy to adopt in our training system. (23) However, we predict that there could be some challenges in the introduction and implementation of the framework in our local programmes. Firstly, the purpose of adopting the framework in collaborative reflective learning and practice should be clearly explained to the residents and faculty.(24) Hodges recently proposed four purposes for reflective practice that are particularly relevant to anaesthetic practice and other postgraduate training. They are reflection as metacognition (thinking aloud on one’s plan or action), mindfulness (support), psychoanalysis (seeking interpretation for one’s thoughts) and confession (seeking judgment for one’s own decisions).(25) Secondly, studies have demonstrated that reflective practice can be taught and encouraged through professional practice.(5) In our context, both resident training and faculty training were necessary to optimise facilitated reflection. Features of effective faculty development include experiential learning with feedback and a diversity of other educational methods, including active roleplaying. Medical education conferences may offer formal faculty development sessions on facilitating reflection. However, cost and time commitment may be limiting features of these events. One strategy is to start teaching reflection with simple exercises that can be facilitated by a small group of trained faculty members. Lastly, reflective training efforts should be continuous and longitudinal in nature, to ideally allow a ‘reflection-on-action’ learner to progress into a ‘reflection-in-action’ reflective specialist.
Our results confirmed that new experiences alone do not necessarily lead to learning. While a stimulus is necessary to trigger interest and curiosity, reflection must be deliberate in order to achieve deeper learning and understanding.(26) Our residents’ perceptions that the role of clinical cases was to provide stimuli for reflection were only partially correct. While interesting and challenging cases provided ready stimuli for reflections, ‘run-of-the-mill’ experiences were important as well. We are of the opinion that while the complexity or novelty of the experience did matter, the critical element in the experience was faculty stimulation and instruction. With appropriate guidance, every clinical case could have been a good learning case.(27) We agree that for reflective learning to be meaningful and successful, structured time, space and preparations are essential.(28) Hence, educators need to strike a balance between maximising experiential exposure and the conditions for reflection and learning.
Articulating, asking questions, receiving feedback, critical reflecting and experimenting are necessary elements in the active learning process.(29) Weakness in one stage of learning can affect the residents’ overall ability to reflect and engage in self-directed learning. In our situation, the perceived lack of a secure environment for learning and feedback could have hindered reflective and experiential learning. Without articulation and feedback, the process of reflection and self-assessment could not be facilitated.(5) Hence, efforts at nurturing a trusting workplace and learning environment for both faculty and residents should go in tandem with reflective training.(27) We were also informed of the critical roles that feedback played in experiential learning. Our residents’ perception of what constituted negative or unhelpful feedback resonated well with that of other studies.(30) In our situation, training sessions on giving and receiving positive and constructive feedback would be essential as well.(31)
Based on our findings, we instituted a series of strategies over the 12 months prior to the writing of this study to improve reflective learning and practice in our programme. These strategies were based on the deficiencies in the current state of reflective practice in the rotation.
Box 1
Strategies undertaken to promote reflective learning and practice in the educational environment:
This study has several limitations. First, both interviewers were senior clinicians and educators in our unit. While the interviewers were cognisant of personal and epistemological reflexivity influences, issues relating to power dynamics and hierarchy could have influenced the participants’ responses. One of the challenges we faced was finding context-knowledgeable professional interviewers to ameliorate these issues. Further, changing sociocultural influences requires time and system changes. Second, owing to the limited number of residents per training rotation and work arrangements, we were unable to achieve the ideal number of at least three participants per focus group. However, in-depth explorations were performed with at least two participants per focus group and data saturation was achieved. Third, as reflective learning and practice are context dependent, the transferability of our results to other educational environments should be carefully assessed. Differing training methods in other settings could yield varying observations and outcomes. Lastly, it has been suggested that the capacity to reflect could be related to the seniority and experience of the learners.(33) Hence, it is likely that senior residents, being more mature practitioners, would have greater reflective capacity. Thus, our findings may not be entirely translatable to a senior residency training programme.
Research in reflective learning and practice is currently rudimentary in Singapore. This gives us exciting opportunities to inquire, reflect and research – what is the impact of our interventions on undergraduate and postgraduate education, and how can we incorporate our patients’ feedback and/or outcomes in reflective practice?
Our study described the current state of reflective learning and practice in anaesthesia training. We described the challenges encountered by the residents and proposed some strategies to stimulate reflective learning. We believe that similar knowledge gaps and challenges are present in other programmes in Singapore. In order to nurture the next generation of reflective practitioners, the reflective capacity of today’s residents needs to be built up. We herein call for a concerted national effort to instil reflective practice.


